|
An Audiovisual Intervention’s
Effects on Psychological Barriers toward initiating
Insulin Therapy among diabetic type 2 patients:
A randomized controlled trial
Faisal Jammah
S Alghamdi
(1)
Mazen Ferwana
(2)
Mohammed Fahad Alsaif
(1)
Fahad Nasser Algahtani
(1)
Emad Masuadi (1)
(1) College of Medicine, King Saud Bin Abdulaziz
University (KSAU-HS), Riyadh, Saudi Arabia
(2) Consultant & Trainer, Family Medicine,
King Abdulaziz Medical City, NGHA, Professor,
King Saud bin Abdulaziz University for Health
Sciences, Co-Director, National & Gulf Center
for Evidence Based Health Practice
Correspondence:
Faisal Jammah S Alghamdi, MBBS
Medical Intern, College of Medicine, KSAU-HS
P.O. Box 22490, Riyadh 11426, Saudi Arabia
Tel: +966566367778
Email: fj.gh@outlook.com
Received: November 2018; Accepted: December
2018; Published: January 1, 2019
Citation: Faisal Jammah S Alghamdi, Mazen Ferwana,
Mohammed Fahad Alsaif, Fahad Nasser Algahtani,
Emad Masuadi. An Audiovisual Intervention’s
Effects on Psychological Barriers toward initiating
Insulin Therapy among diabetic type 2 patients:
A randomized controlled trial. World Family
Medicine. 2019; 17(1): 29-35.DOI: 10.5742MEWFM.2019.93596
|
Abstract
Introduction: This study evaluates
the effectiveness of educational videos
against patients’ fixed beliefs and
lack of knowledge in comparison with traditional
educational methods. It investigates the
effectiveness of these tools in overcoming
patients’ psychological barriers
toward insulin therapy.
Methods: This
randomized, controlled trial used the
validated insulin treatment appraisal
scale (ITAS) to evaluate patients’
psychological barriers. An educational
video and brochure were developed, each
containing the same contents. The study
was conducted in King Abdulaziz city housing
with a total sample size of 126, divided
into an intervention group (who were shown
the video) and a control group (who were
given the brochure). Both groups filled
out the same questionnaire before the
intervention, immediately after the intervention,
and six weeks later.
Results:
Neither educational method showed superiority
to the other. Most of the questionnaire
items had a nonsignificant p-value for
both methods, and even when one intervention
method was effective, the other method
showed similar effectiveness.
Conclusion:
This study showed no superiority of
the video over the brochure, which cost
less and required less effort to produce.
Trial registration
number: NCT03544645
Key words:
audiovisual; diabetes type 2; educational
intervention; insulin therapy; psychological
insulin barriers.
|
Insulin should be prescribed more frequently
among type 2 diabetic patients, especially when
oral medications alone are not effective anymore
[1]. Despite being the most effective diabetes
treatment, patients often feel reluctant to
initiate insulin therapy when it is needed.
Many studies relate this reluctance to reasons
such as fear of disease progression, needle
anxiety, feelings of guilt and failure, concerns
about hypoglycemia, sense of loss of control
over one’s life, reduced quality of life,
and the fear of being stigmatized [1-7]. All
these reasons have contributed to the prevalence
of uncontrolled diabetes; a survey conducted
in the USA showed that the percentage of controlled
diabetic patients was only 36% [8], and a 2012
study in the Al Hassa region of Saudi Arabia
showed that the percentage of uncontrolled diabetic
patients was 69% [9].
The impact of most of these reasons are overestimated
by patients and can be overcome with an insulin
analogue and a new delivery method. For example,
a novo pen, which many studies have found to
be less painful, is easier to carry around than
traditional delivery methods and leads to less
hypoglycemic events [10-12]. The fact that patients
still so frequently cite the reasons above indicates
that up-to-date methods are not being provided
to patients, which could be accomplished through
traditional educational methods such as brochures,
leaflets, or face-to-face discussions [13].
A newer educational technology is educational
videos, and many studies emphasize the effectiveness
of this method [14-18]. In one study, a video-based
lifestyle educational trial was designed for
newly diagnosed type 2 diabetics, who were divided
into a video education group and a control group.
The video education group showed more improvement
in general knowledge related to lifestyle than
the control group [14]. Another study about
heart failure patients revealed that patients
who received video education showed less signs
and symptoms of heart failure, such as edema,
fatigue, and dyspnea, than another group that
received only traditional education [15]. Even
if we compare video education with other newer
methods such as internet research, video education
is more effective because patients are more
likely to review all the information provided
to them [16]. In addition, another study found
that video intervention was one of the best
methods to increase the knowledge of health
issues, such as certain disease complications,
in people with low literacy [17].
Furthermore, a systematic review that included
40 studies related to video intervention showed
how video education was effective in three major
ways: supporting the treatment decision, reducing
anxiety, and supporting coping skills to increase
self-care practices [18]. Since there have been
no previous studies comparing the difference
in effects between traditional and non-traditional
education methods on diabetic patients’
attitudes in Saudi Arabia, this study aims to
compare the impact of audiovisual educational
materials versus printed educational materials
on type 2 diabetic patients’ knowledge,
attitudes, and practices towards insulin therapy.
It does so by assessing the patients before,
immediately after, and 6 weeks after the intervention.
We conducted a randomized controlled trial
on type 2 diabetic patients who agreed to participate
in the study after screening them for inclusion
and exclusion criteria. The target population
of the study was type 2 diabetic patients who
had an A1c of 8 mg/dL or above, were aged 30
to 70 years, and had not yet begun insulin therapy.
Patients currently experiencing pregnancy, blindness,
profound vision loss, or severe mental problems
such as psychosis were excluded.
The study was conducted from March to June
2017 in a community-based polyclinic located
in the King Abdulaziz city housing for the National
Guard in Riyadh, Saudi Arabia. This polyclinic
includes primary care centers and serves about
60,000 individuals, consisting of soldiers and
their families as well as the professionals
who work there and their families. We developed
an educational video and brochure, both of which
contained the same content about knowledge,
attitude, behavior, and psychological barriers
toward insulin therapy. The intervention group
was shown the educational video and the control
group was given the brochure. Both groups filled
out a questionnaire before the intervention,
then immediately after the intervention filled
out the same questionnaire to assess the materials’
immediate effects. Six weeks later, both groups
filled out the same questionnaire once more
to measure the long-term effects. The immediate
and long-term effects of both groups were compared
to assess the materials’ effects on participants’
knowledge, attitudes, behaviors, and psychological
barriers toward insulin therapy.
A computerized sequence in Microsoft Excel
2016 generated a randomized list of patients,
allocating participants into 2 groups: an audiovisual
intervention group and a printed material control
group. A serially numbered opaque sealed envelope
(SNOSE) contained these group assignments. The
total sample size was 126 patients (63 in each
group), which afforded us an 80% power to detect
a difference of at least 5% in the mean knowledge
percentage between the two groups, with an equal
standard deviation of 10% and a significance
level () of 5% using two proportions (z-test).
The validated insulin treatment appraisal scale
(ITAS) questionnaire was used [19]. It is available
on the internet free of charge, and permission
to use it was obtained. The questionnaire measured
the following variables: attitude, knowledge,
practice, and behavior. It was translated into
Arabic and pre-tested.
The educational video, which we developed and
validated for this study and presented to the
intervention group, aimed to address the psychological
barriers mentioned in the questionnaire and
tried to correct patients’
misconceptions about insulin therapy. More specifically,
it aimed to overcome the barriers by briefly explaining
the pathophysiology of type 2 diabetes and the
ways to manage type 2 diabetes, focusing especially
on the advantages, adverse effects, and misconceptions
about insulin therapy. Its content was developed
based on the American Diabetes Association’s
2017 Standards of Medical Care in Diabetes [20];
the validation process included family physicians
to ensure that the content was appropriate for
the patients and medical students to ensure the
quality of the design and avoid any language mistakes;
it also included type 2 diabetic patients with
similar inclusion and exclusion criteria of this
study to ensure that the video is suitable for
them in terms of language and approach. The validation
paper has been published separately (27), and
the video with English subtitles can be accessed
from the link in the reference list [21].For each
item on the questionnaire, two p-values were measured.
The first was obtained with McNemar’s test,
to measure the effect of each intervention individually.
The second was obtained using a two-proportion
z-test to compare the two interventions and determine
if either was superior. Results with a p <
0.05 were considered significant. IBM SPSS Statistics
20, manufactured by IBM Corp., was used for data
analysis.
Ethics
This study was sponsored and ethically approved
by King Abdullah International Medical Research
Center’s (KAIMRC) ethic committee with
ID number (SP16/235), and all patients provided
written consent. It was also registered in the
trial registry, clinicaltrial.gov, with a trial
registration number of NCT03544645.
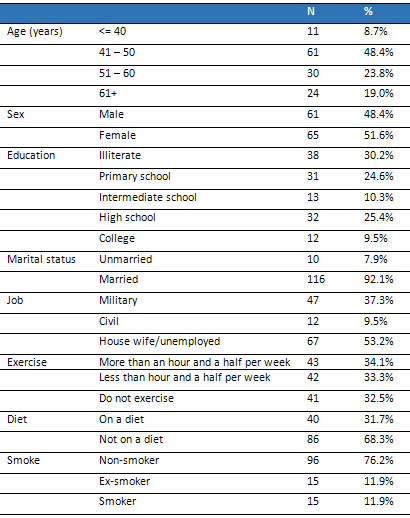
The study included 126 diabetic patients, with
no losses during the study. Patients’ demographics
are presented in Table 1. Table 2 shows the
effects of the two intervention methods (the
video and the brochure) regarding patients’
fixed beliefs, namely their psychological barriers
to insulin therapy (determined through 10 questions),
and regarding their understanding of insulin
therapy as the ideal treatment for their condition
(2 questions, q6 and q7, in Table 2). The percentages
in Table 2 represent the participants who agreed
with the questions’ statements, and each
question had 3 main p-values: one for the effect
of the video, one for the effect of the brochure,
and the last to show any superiority in method,
whether it was for the video or the brochure.
The different p-values measure the reductions
in barriers between before and immediately after
the intervention, as well as the reduction between
before and 6 weeks after the intervention.
As determined by McNemar’s test, the questions
related to the psychological barriers to insulin
therapy (questions 1 and 3: “I am worried
about starting insulin therapy” and “Taking
insulin means my health will deteriorate”)
showed significant p-values (<0.05) for both
the video and the brochure. Interestingly, questions
11 and 12 (“Taking insulin increases the
risk of low blood glucose levels” and “Insulin
causes weight gain”) showed positive p-values
for both the brochure and video, but the reductions
were of negative value and, since the question
was not a negative statement, these values were
significant for their reverse outcomes. A reverse
outcome here means that instead of decreasing
the barriers, the intervention methods increased
them , although these barriers were addressed
directly with both methods.
There were no significant p-values for the
other barriers related to insulin therapy, indicating
that neither intervention was effective in this
regard. However, q6 and q7 (“Taking insulin
helps to prevent complications of diabetes”
and “Taking insulin helps to improve my
health,” respectively), which were related
to the benefits of insulin but not psychological
barriers toward insulin therapy, showed significant
p-values for both interventions.
As for the two-proportion z-tests used to compare
the two interventions, most p-values were non-significant.
That is, even when the video showed effectiveness,
the brochure showed an equal effect; thus, neither
method appeared superior to the other.
Table 1: Participants’
Demographics
Click here for Table
2: Questionnaire Items
Although both interventions had a slight effect,
it was still not large enough to alter patients’
fixed beliefs and behaviors. The interventions
reinforced the positive ideas patients already
had about the benefits of insulin therapy, but
were not sufficient to break their psychological
barriers to insulin therapy, such as feelings
of guilt and failure, fear of disease progression,
feelings of a loss of control over one’s
life, and the fear of being stigmatized, even
though both intervention methods addressed these
beliefs directly. In fact, patients’ worries
about hypoglycemic attacks and weight gain increased
at the mere mention of them in the interventions,
even though the interventions indicated that
new methods could help overcome these problems.
Overall, neither method was found to be superior.
A meta-analysis has shown that video interventions
are effective in some settings such as breast
self-examination, prostate cancer screening,
sunscreen adherence, self-care in patients with
heart failure, and HIV testing and treatment
adherence [22]. However, this study shows that
such an intervention is not effective in changing
overall behaviors or attitudes, nor fixed beliefs
toward insulin therapy, such as psychological
barriers. Thus, the intervention’s goal
plays an important role in its impact.
The result of this study raises the question
of whether multifaceted intervention could be
more effective than one-method intervention.
One study that targeted diabetic patients with
multifaceted interventions, such as problem-based
learning sessions and educator-patient face-to-face
sessions, showed improvements in their A1C and
blood pressure [23]. In addition, two studies
on multifaceted interventions showed improvements
in drug adherence for post ACS and anti-depressant
drugs using booklets, voice messages, and counseling
interventions [24-25].
The present study had several limitations and
strengths. The limitations included a sample
limited to a clinic located in housing for National
Guard soldiers, which may not represent the
population of Riyadh as a whole. The strengths
include the study’s randomized approach,
which helped minimize bias, as well as the high
response rate, strict inclusion criteria, the
consistency of the research method, the follow-up
after six weeks, and and the fact that the educational
video was validated by the authors of this study.
Audiovisual methods such as educational
videos are important sources for delivering
different kinds of information. This
study demonstrates that these methods
can be useful for delivering new information
and increasing people’s general
knowledge, but sometimes fall short
in changing people’s pre-existing
fixed beliefs, such as psychological
barriers regarding insulin therapy.
The results of the study raise the question
of whether educational materials are
indeed superior to doctor–patient
educational sessions, which are more
interactive and allow the patient to
ask questions. It also suggests that
a multifaceted intervention could be
more effective than a one-method intervention.
Future research should consider what
further efforts are required to change
misleading information that people believe.
Determining what new technologies should
be utilized as intervention methods
is a wide research field with a promising
future. One such technology is social
media, which is now widely accepted
and has many active users. One study
has demonstrated that social media can
be effective as an intervention method
to increase patients’ physical
activity [26], but further research
on this subject is lacking.
Funding source: The research
was supported by King Abdullah International
Medical Research Center (KAIMRC) [Grant
Number: SP16\235]. The funder had no
role in study design; in the collection,
analysis and interpretation of data;
in the writing of the report, and in
the decision to submit the article for
publication.
Acknowledgments: We give special
thanks to the National Guard Health
Affair department and College of Medicine,
as well as King Saud Bin Abdulaziz University
for Health Science, for their consultations
and the permission to use their faculties.
We would also like to thank Editage
(www.editage.com) for English language
editing.
1. Edelman S, Pettus J. Challenges associated
with insulin therapy in type 2 diabetes
mellitus. Am. J. Med. 2014;127:S11–6.
2. Bogatean MP, Hâncu N. People
with type 2 diabetes facing the reality
of starting insulin therapy: factors involved
in psychological insulin resistance. Pract.
Diabetes Int. 2004;21:247–52.
3. Korytkowski M. When oral agents fail:
practical barriers to starting insulin.
Int. J. Obes. Relat. Metab. Disord. 2002;26
Suppl 3:S18–24.
4. Funnell MM. Overcoming barriers to
the initiation of insulin therapy. Clin.
Diabetes. 2007;25:36–38.
5. Davis SN, Renda SM. Psychological insulin
resistance: overcoming barriers to starting
insulin therapy. Diabetes Educ. 2006;
32 Suppl 4:146S–52S.
6. Peragallo-Dittko V. Removing barriers
to insulin therapy. Diabetes Educ. 2007;33
Suppl 3:60S–5S.
7. Brod M, Kongsø JH, Lessard S,
Christensen TL. Psychological insulin
resistance: patient beliefs and implications
for diabetes management. Qual. Life Res.
2009;18:23–32.
8. Koro CE, Bowlin SJ, Bourgeois N, Fedder
DO. Glycemic control from 1988 to 2000
among U.S. adults diagnosed with type
2 diabetes: a preliminary report. Diabetes
Care. 2004;27:17–20.
9. Khan AR, Al-Abdul Lateef ZN, Al Aithan
MA, Bu-Khamseen MA, Al Ibrahim I, Khan
SA. Factors contributing to non-compliance
among diabetics attending primary health
centers in the Al Hasa district of Saudi
Arabia. J Fam Commun Med. 2012;19:26–32.
10. Kadiri A, Chraibi A, Marouan F et
al. Comparison of NovoPen 3 and syringes/vials
in the acceptance of insulin therapy in
NIDDM patients with secondary failure
to oral hypoglycaemic agents. Diabetes
Res. Clin. Pract. 1998;41:15–23.
11. Tschiedel B, Almeida O, Redfearn J,
Flacke F. Initial experience and evaluation
of reusable insulin pen devices among
patients with diabetes in emerging countries.
Diabetes Ther. 2014;5:545–55.
12. American Diabetes Association, Standards
of medical care in diabetes—2008.
Diabetes Care. 2008;31 Suppl 1:S12–54.
13. Khan MA, Shah S, Grudzien A et al.
A diabetes education multimedia program
in the waiting room setting. Diabetes
Ther. 2011;2:178–88.
14. Dyson PA, Beatty S, Matthews DR. An
assessment of lifestyle video education
for people newly diagnosed with type 2
diabetes. J Hum Nutr Diet. 2010;23:353–59.
15. Albert NM, Buchsbaum R, Li J. Randomized
study of the effect of video education
on heart failure healthcare utilization,
symptoms, and self-care behaviors. Patient
Educ Couns. 2007;69:129–39.
16. Frosch DL, Kaplan RM, Felitti VJ.
A randomized controlled trial comparing
internet and video to facilitate patient
education for men considering the prostate
specific antigen test. J. Gen. Intern.
Med. 2003;18:781–87.
17. Gerber BS, Brodsky IG, Lawless KA
et al. Implementation and evaluation of
a low-literacy diabetes education computer
multimedia application. Diabetes Care.
2005;28:1574–80.
18. Krouse HJ. Video modelling to educate
patients. J Adv Nurs 2001;33:748–57.
19. Snoek F, Skovlund S, Pouwer F. Development
and validation of the insulin treatment
appraisal scale (ITAS) in patients with
type 2 diabetes. Health Qual Life Outcomes.
2007;5:69.
20. American Diabetes Association, 1.
Promoting health and reducing disparities
in populations. Diabetes Care. 2017; 40:S6–10.
21. Alsaif M. Patients’ barriers
towards insulin therapy 2016. https://www.youtube.com/watch?v=Ye9SRh59pjg&t=112s.
Accessed 16 Oct 2018
22. Tuong W, Larsen ER, Armstrong AW.
Videos to influence: a systematic review
of effectiveness of video-based education
in modifying health behaviors. J Behav
Med 2014;37:218–33.
23. Piatt GA, Anderson RM, Brooks MM et
al. 3-year follow-up of clinical and behavioral
improvements following a multifaceted
diabetes care intervention: results of
a randomized controlled trial. Diabetes
Educ. 2010;36:301–9.24. Ho PM, Lambert-Kerzner
A, Carey EP et al. Multifaceted intervention
to improve medication adherence and secondary
prevention measures after acute coronary
syndrome hospital discharge: a randomized
clinical trial. JAMA Intern. Med. 2014;174:186–93.
25. Katon WA, Robinson P, Von Korff M
et al . A Multifaceted intervention to
improve treatment of depression in primary
care. Arch Gen Psychiatry. 1996;53:924–32.
26. Zhang J, Brackbill D, Yang S, Centola
D. Identifying the effects of social media
on health behavior: data from a large-scale
online experiment. Data Brief. 2015;5:453–57.
27. Fahad Algahtani, Mazen Ferwana, Mohammad
Alsaif, Faisal Alghamdi. Validation of
Audiovisual Educational Tool that discusses
psychological insulin barriers for type
2 diabetic patients. World Family Medicine.
2019; 17(1): 23-28.DOI: 10.5742MEWFM.2019.93595
|

