|
Radiofrequency
surgery:
offering a novel approach to ano-rectal diseases
|
|

Author
Pravin J. Gupta M.S
Address for correspondence
Pravin J. Gupta M.S
Consulting Proctologist
Gupta Nursing Home
D/9, Laxminagar
NAGPUR - 440022
India
E-mail: drpjg_ngp@sancharnet.in,
drpjg@yahoo.co.in
Fax: 49 712 2547837
Phone: 49 712 2231047

ABSTRACT
Background - Radiofrequency
surgery is a method of utilizing high frequency [3.8 to 4MHz]
radio wave energy to incise, excise, or coagulate tissues.
Radiofrequency (RF) is a relatively new modality that is being
used for ano-rectal surgeries with increasing frequency. Radiofrequency
energy consists of an alternating current that moves from
an active electrode that is used within the area of treatment
to dispersive electrodes that are placed on the patient. As
the RF energy is applied, frictional heating of tissues results,
with cell death occurring at temperatures between 60 and 1000º
C.
Objectiveb - This
paper discusses pre-clinical and early clinical experience
with radiofrequency for various ano-rectal procedures namely
hemorrhoids, anal fistula, anal polyps, sinuses and anal papillae.
An Ellman dual frequency radiofrequency generator was used
to carry out the procedures. This study is intended to be
somewhat of a " how we do it" manual, explaining
the principles of radiofrequency.
Conclusion - Radiofrequency
proctological procedures are simple to perform with many advantages
over the more traditional techniques. The procedures take
less operative time, the postoperative recovery is accelerated
and the incidences of complications are negligible. Nevertheless,
randomized and comparative evaluation with conventional techniques
is called for to establish the long-term efficacy and reliability
of radiofrequency surgery.
Keywords - Radiofrequency,
Proctology, Electrosurgery, Hemorrhoids, Anal fistula
INTRODUCTION TO RADIOFREQUENCY
SURGERY
The use of electric currents in medicine has
been documented almost since electricity itself was discovered.
Low frequency alternating currents are used in physiotherapy
for their ability to cause contractions in muscle fibres.
Radiofrequency is a refined type of electro
surgery that utilizes a wave of electrons at a frequency between
2 and 4MHz to incise, excise, ablate or coagulate the targeted
tissue (1).
Radiofrequency surgery has a lengthy documented
history of use in oral, ophthalmic, plastic, and gynecology
surgery. It was first used for the treatment of snoring. Gradually,
its use in the practice of dermatology (2), cosmetology, cardiology,
neurosurgery, hepatology, and ENT (3-4) procedures gained
momentum and popularity. It has multi-faceted usages in the
respective medical fields (5). However, there have been few
published reports of its use in proctology.
Surgeons and proctologists have used this instrument
very sparingly, and that too more out of curiosity than a
serious attempt to utilize its vast potentials. The reason
perhaps, might be that they were satisfied with the results
of the conventional techniques employed by them, or were not
sure about the use of this tool in the ano-rectal surgery
for want of sufficient literature on the subject.
For a surgeon practicing proctology, there are
few important goals to achieve. The aim of attempting a new
technique should be of minimizing tissue damage and obtaining
an assured hemostasis during reconstruction, excision, or
ablation process.
Radio surgery can simply be termed as an electro
surgery at radiofrequency. The term 'radio' is used because
the frequency of the device creating these waves is comparable
to radiowave frequency used for broadcasting. It is necessary
here to dispel any possible misconception about radio surgery
by discussing two other, older modalities namely, 'electrocautery'
and 'hyfrecation' that are quite different from radio surgery.
Electrocautery involves the passage of low frequency,
low voltage, and low wattage alternating current (0.5 - 1.5
MHz) through the electrode, which resists the flow of current
and becomes hot. In electrocautery, the heat [rather than
the radio wave is transferred to the soft tissue by convection.
Massive cell destruction results from the application of cautery
and the destruction caused by this cauterization are equivalent
to that of a third degree burn.
While in hyfrecation, a highly modulated high
frequency current of low wattage and high voltage is supplied
to the electrode, and the surface of the tissue is burnt by
a spark, which is produced between the tip of the electrode
and the tissue. Its effect is mainly superficial and it cannot
be used to incise the tissue.
The high frequency radio surgery and its results
should also not be confused with diathermy, electric cauterization,
or spark producer. With radiofrequency, the targeted tissue
temperatures stay localized within a 60-100°C range thus
limiting heat dissipation and damage to adjacent tissue. In
contrast, electrocautery, diathermy, or laser temperatures
are significantly higher (750-900°C) which result in a
very high heat propagation, which is far in excess of the
desired therapeutic need (6).
Electro surgical machines operating at frequencies
below 3 MHz causes the electrode itself to heat and it has
been found that these electrodes, if made of steel, tend to
melt away with repeated use. It has been determined that the
ideal frequency for achieving effortless cutting of tissues
is approximately 4 MHz (7).
Radiofrequency energy has been used extensively
in many different medical applications and specialties for
its ability to achieve a precise and controlled thermal ablation
of soft tissue. The heat for this ablation is generated by
a natural resistance of the tissue, which comes in the path
of the waves released through the electrode tip of the device.
The cellular water in the soft tissues gets heated and when
the temperature reaches 1000C, it starts boiling and produces
steam, which results in cellular molecular dissolution of
individual tissue cells. The cells exposed to these waves
are destroyed while the surrounding tissues remain unaffected.
This property of radiofrequency eliminates the possibility
of undue damage to the normal tissues, while improving the
surgical precision (8).
The radiofrequency unit functions with the active
electrode concentrating the high frequency energy at its tip,
and then transmitting it to the passive electrode which returns
the waves to the unit, making them more effective (9).
The radiofrequency unit- While there are different
radiofrequency units in the market, we found the Ellman dual
frequency 4MHz [Ellman International Inc, Oceanside, USA]
with a proven and successful history of its efficacy, and
being available with a multitude of electrode tips, is quite
useful to carry out various proctological procedures. The
unit produces output power of 100 Watts at two different frequencies
i.e. 4MHz and 1.7MHz. While the frequency of 4MHz is used
for four standard settings like 1. Cutting, 2. Cutting and
Coagulation, 3. Pure coagulation and 4.Fulguration, the frequency
of 1.7MHz is used for bipolar coagulation (10).. The unit
has a digital display and audible signal to indicate when
the unit is activated. The output power intensity to be delivered
through the electrode can be preset between 1 and 100.

Figure 1: Radio Surgical Unit
The high frequency current delivered by the
unit is modified by filtering and rectification to produce
one of the four waveforms, namely:
- Fully filtered - suitable for cutting-produces
least lateral heat,
- Fully rectified - suitable for cutting
but which also produces lateral heat to coagulate,
- Partially rectified modulated - suitable
for coagulation and which generates maximum lateral heat,
- Fulguration - spark gap waveform-
to produce desiccation or dehydration.
The fifth mode of waveform is bipolar, which
is primarily used in microsurgery and as haemostatic current
of high precision in wet or dry areas, using a pair of tweezers
as electrodes.
An 'antenna' is used to focus the "radio
wave" which unlike traditional electro surgical units,
does not need to be in contact with the skin of the patient.
It could rather be placed in close proximity of the operating
field. The unit is activated by a foot pedal. The 'active'
or patient electrode is interchangeable with four different
modes of activities (11).
- A Needle electrode, which is used for making
incisions;
- Loop electrodes, which are used for excision
and shaping tissues;
- Ball electrode, which is used for coagulation;
and
- Rod electrodes, which are used for fulguration
and desiccation of the tissues.
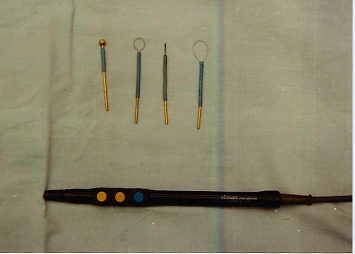
Figure 2- Hand piece and electrodes
of the radiofrequency device
We have been working with this equipment for
thelast 5 years to perform most of the proctological surgeries.
The property of simultaneous cutting and coagulation achieved
by this machine has attracted us most. Such versatility of
the tool is of utmost utility in most procedures performed
within the ano-rectal area, which is quite vascular and having
very limited accessibility. While operating in such a difficult
area, bleeding and oozing from the tissue often hampers clear
vision of the operative field, rendering the procedure difficult
and a time-consuming job. Radiofrequency surgical techniques
successfully overcome these deficiencies.
Indications of 3.8 - 4.0MHz dual frequency
Radio surgery -
Radiofrequency surgery can be used to tackle a variety of
anal lesions. They include-
- Hypertrophied anal papillae
- External hemorrhoids
- Sentinel tags in anal fissures
- Perianal warts and condylomata
- Rectal polyps
- Fibrous anal polyps
- Perianal and pilonidal sinuses
- Post fissure antibiomas
- Perianal papillomas
- Biopsies
- Fistula in ano
- Hemorrhoids
- Rectal prolapse
Surgical Techniques
Most applications are accomplished with under local anesthesia,
short-term general anesthesia or under a caudal block.
While many different electrodes are available with the unit,
we could perform most of the procedures using the loop, the
ball and the fine needle electrodes.
Hypertrophied Anal Papilla
They immediately disappear on coming in contact with the activated
ball electrode in coagulation mode (12).
External Hemorrhoids.
Small masses are coagulated with the ball electrode. However,
a large sized mass is required to be shaved off with the round
loop electrode kept in a cutting and coagulation mode. Any
bleeders from the base could well be coagulated with the ball
electrode.
Sentinel Piles in Fissure in Ano
Sentinel pile or tags are a common accompaniment of chronic
anal fissures. If the tag is small, it could be directly coagulated
with a ball electrode. In case it is large, then it is excised
with the round loop by first securing the bleeding points
and coagulating them thereafter (13).
Perianal Warts and Condylomata
These could be shaved off using a loop electrode in cut and
coagulation mode. Once all of them are removed, the operated
area is 'sterilized' by rolling a ball electrode on coagulation
mode to ensure removal of invisible warts and the viral colony.
The intra-anal warts could preferably be coagulated rather
than being excised.
Rectal Polyp
It is better if they are dealt with within the anal canal.
A longer length ball electrode is passed through the proctoscope,
and a coagulation field is encircled around the base of the
polyp. The pedicle is then coagulated until the mass is separated.
This ensures a negligible bleeding which could be secured
by coagulation with the help of the ball electrode in coagulation
mode.
Fibrous anal polyps
These are forms of exaggerated anal papillae. These could
be coagulated in situ using the ball electrode, but
when these are large enough, these may be shaved off with
a loop electrode after coagulating the base (14).
Perianal and Para sacral Sinuses
These include the pilonidal sinuses, post anal sinuses, and
post-traumatic sinuses. Methylene blue dye mixed with hydrogen
peroxide is injected in the sinus opening, which spreads out
in the sinus tract. The tracts so identified, are then incised
and laid opened with the needle electrode. The bleeding points
are secured by coagulating them with the ball electrode (15).
The wound is left open to heal by secondary intension.
Perianal Papillomas
These can precisely be removed using a loop electrode of a
suitable size. The raw area left behind may require a touch
of a ball electrode in coagulation mode to arrest any oozing
from the base.
Perianal Antibiomas
These are also known as antibiotic granuloma, organized abscess,
sterile abscess etc. The aim of treatment is to curette the
complete cavity, which could be achieved by incising the center
of the lump using a needle electrode in cut and coagulation
mode. All the granulation tissues, which feel hard with little
bleeding, are scrapped out with a round loop electrode until
a soft red base is reached.
Biopsies
Biopsies can be performed for suspected growths in and out
of the anus. A round loop electrode is the best tool. It should
be used on a cutting mode, so that with only a minimum lateral
thermal damage, the histology is not distorted (16).
Fistula in Ano
With a needle electrode on cut/coag mode, the fistula tract
is slit opened over the director probe, which is inserted
in the tract. The edges of the wound are shaved off by the
loop electrode to create a pear shaped wound tapering towards
the anus. The bleeding points are held in the hemostat and
are coagulated (17).
Hemorrhoids
Radiofrequency surgery is useful in the treatment of both,
early and advanced grades of hemorrhoids. The non- prolapsing
internal hemorrhoids could be directly coagulated in-situ
with the ball electrode of a sufficient length under a surface
anesthesia as an office procedure (18).
The advanced and prolapsing hemorrhoids are first ablated
with a ball electrode and then the ablated hemorrhoidal mass
is plicated with absorbable sutures to ensure fixation of
the anal cushions to the underlying structures. The results
of this procedure are more assuring when compared with the
conventional surgical techniques (19).
Rectal Prolapse
Radiofrequency has been used as an adjuvant therapy in elderly
patients with rectal prolapse. A circumferential coagulation
of the anoderm is made with the ball electrode and then a
Thiersch's stitch is tied to encircle the anal verge. Radiofrequency
coagulation induces fibrosis and create a zone of band around
the anal verge which helps in tightening the anal opening
and preventing prolapse (20).
Post-Operative Care
Almost all the abovementioned procedures are carried out as
a day care surgery. Analgesics, antibiotics and stool softeners
are prescribed according to the requirement. No specific wound
care is found needed.
Complications
No major complications have been encountered with these procedures.
Few minor ones to mention are:
- Deep dissection can cause
more scarring and longer time for healing of the wounds.
- Excessive release of power produces more
smoke and charring.
- Accidental burns either on the patient or
on operator due to unintended activation of hand piece have
been reported.
Precautions to be taken while operating with
the radiofrequency unit
Approximately ten seconds should be allowed for the tissues
to cool between repeat applications of the electrodes. The
two factors, which go to make this a good technique, involve
the accuracy in power setting on the unit and the swift action
of the cutting stroke.
Radiofrequency procedure should not be employed
by, or on anyone who wears a pacemaker. The instrument should
not be used in the presence of flammable or explosive liquids
or gases. The skin under treatment should not be prepped with
alcohol.
If proper settings are not known, the operator
should start with a low power setting and cautiously increase
power until an ideal cut is accomplished, without a tissue
drag and no sparking. The finer the electrode used, the less
would be the lateral heat spread and thus causing least damage
to the adjacent tissues. It is recommended that a hands-on
introductory course be taken before attempting the use of
this technology.
Comparison with other equipments
The other equipments used in the field of ano-rectal surgery
include the Infrared coagulator, Cryogun, Lasers and Electrocautry21,
22. A brief account of their comparison with the radiofrequency
is as below.
| RADIOFREQUENCY |
INFRA RED COAGULATION |
| Multiple applications/uses in proctology
surgery. |
Limited to coagulating bleeding internal
hemorrhoids. |
| Can cut, coagulate or fulgurate. |
Can only coagulate. |
| Low recurrence rate after treatment. |
High recurrence rate in hemorrhoids. |
| RADIOFREQUENCY |
ELECTROCAUTERY OR BOVIE |
| Simultaneous cut and coagulation. |
Requires different modes and adjustments
for different applications. |
| Minimal smoke production. |
Produces excessive smoke. |
| Minimal surrounding tissue damage. |
Tissue damage like 3rd degree burns. |
| Heats tissues below 1000 C. |
Raises tissue temperature above 5000C. |
| Sterilizes tissues under application. |
Can cause postoperative sepsis. |
| Minimal scarring creates soft supple scar.
|
Gross scarring and fibrosis. |
| Faster healing. |
Slow healing. |
|
RADIOFREQUENCY
|
CRYOSURGERY |
| Tissue interaction can be predetermined with power setting
selection. |
Difficult to achieve precise tissue destruction. |
| No tissue adherence or charring. |
Probes often stick to the site of application and cause
detachment of the tissue with bleeding. |
| Minimal postoperative edema and discharge. |
Extensive edema and profuse discharge from the treated
area. |
| Result is immediately visible. |
Uncertainty of result due to variable tissue response. |
| Multiple uses in proctology. |
Used for the treatment of hemorrhoids alone. |
|
RADIOFREQUENCY
|
LASER |
| Adaptable for multiple uses in proctology. |
Limited applications in proctology surgery. |
| Equally effective for cutting and coagulation. |
Good cutting effect but poor coagulation. |
| Unit cost much less. |
High instrument cost. |
| Portable. |
Limited mobility. |
| Inexpensive treatment. |
Costly treatment. |
| Easy anal canal access due to variable electrodes. |
Limited access in the anal canal. |
| Faster healing. |
Risk of misdirected reflected beam and delayed wound
healing. |
Other advantages of radiofrequency
surgery -
Radiofrequency surgery allows cutting without pressure, and,
consequently, there is little tissue damage and minimal scarring
(24). The electrode tip is sterile, as is all the tissue being
exposed to it (25). Healing is by granulation, with a soft
and supple scar26. It could be performed with ease even in
the depth and in difficult areas like the anal canal. There
are minimal incidences of postoperative infection, thereby
achieving faster wound healing with negligible use of sutures
etc.
The electrodes are reusable
and may be kept in cold sterilization solution when not in
use.
CONCLUSION
Use of radiofrequency in performance of various
proctology surgeries results in less trauma to the cells,
less fibrous scarring and less postoperative discomfort. The
procedures are cost effective as no expenses of recurring
nature are incurred. The radiofrequency tool having a versatile
use in various surgical procedures can prove handy for the
practicing surgeons.

REFERENCES
| 1. |
Fernando HC, Hoyos AD, Litle
V, Belani CP, Luketich JD. Radiofrequency ablation: identification
of the ideal patient. Clin Lung Cancer. 2004; 6:149-153. |
| 2. |
Rex J, Ribera M, Bielsa I,
Paradelo C, Ferrandiz C. Surgical management of rhinophyma:
report of eight patients treated with electrosection.
Dermatol Surg 2002; 28: 347-349. |
| 3. |
Wedman J, Miljeteig H.Treatment
of simple snoring using radio waves for coagulation of
uvula and soft palate: a day-case surgery procedure. Laryngoscope.
2002; 112: 1256-1259. |
| 4. |
Plant RL. Radiofrequency treatment
of tonsillar hypertrophy. Laryngoscope 2002; 112: 20-22. |
| 5. |
Weber JC, Navarra G, Jiao LR,
Nicholls JP, Jensen SL, Habib NA. New technique for liver
resection using heat coagulative necrosis. Ann.Surg.2002;
236: 560-563. |
| 6. |
Glover JL, Bendick PJ, Link
WJ. The use of thermal knives in surgery: Electrosurgery,
lasers, plasma scalpel. Curr Probl Surg1978; 15:1-78. |
| 7. |
Bridenstine JB. Use of ultra-high
frequency electrosurgery (radiosurgery) for cosmetic surgical
procedures. Dermatol Surg 1998; 24:397-400. |
| 8. |
Hettinger DF. Soft tissue surgery
using Radiowave techniques. J.Am.Podiatr.Med.Assoc. 1997;
87: 131-135. |
| 9. |
Valinsky MS, Hettinger DF,
Gennett PM. Treatment of verrucae via radiowave surgery.
J Am Podtr Med Assoc 1990; 80: 482-488. |
| 10. |
Brown J.S. Radio surgery for
minor opeations in general practice. Cosmetic Dermatology,
2000:33-36. |
| 11. |
Hurwitz JJ, Johnson D, Howarth
D, Molgat M. High-frequency radio wave electosection of
full-thickness eyelid tissues. Can J Ophthalmol. 1992;
28: 28-31. |
| 12. |
Gupta PJ. Removal of hypertrophied
anal papillae and fibrous anal polyps increases patient
satisfaction after anal fissure surgery. Tech Coloproctol.
2003; 7: 155-158. |
| 13. |
Gupta PJ. Sphincterotomy with
radio frequency surgery: a new treatment technique of
fissure in ano and associated pathologies. Rom J Gastroenterol.
2003; 12: 37-40. |
| 14. |
Gupta PJ. Current trends of
management for fissure in ano. Rom J Gastroenterol. 2002;
11: 25-27. |
| 15. |
Gupta PJ. Pilonidal sinotomy
with radiofrequency. J Coll Physicians Surg Pak. 2003;
13: 540-541. |
| 16. |
Saidi MH, Setzler FD Jr., Saddler
RK, Farhart SA, Akright BD. Comparison of office loop
electro surgical conization and cold knife conization.
J Am Assoc Gynecol laparosc. 1994; 1: 135-139. |
| 17. |
Gupta PJ. Anal Fistulotomy
with Radiofrequency. Dig Surg 2004; 21: 72-73. |
| 18. |
Gupta PJ. Novel technique:
radiofrequency coagulation--a treatment alternative for
early-stage hemorrhoids. MedGenMed. 2002; 4: 1. |
| 19. |
Gupta PJ. Radiofrequency ablation
and plication of hemorrhoids. Tech Coloproctol. 2003;
7: 45-50; discussion 50. |
| 20. |
Gupta PJ.Radiofrequency coagulation
with Thiersch's Operation- A better palliative treatment
in prolapse rectum. Curr Surg 2002; 59: 567-569. |
| 21. |
Turner RJ, Cohen RA, Voet RL,
Stephens SR, Weinstein SA. Analysis of tissue margins
of cone biopsy specimens obtained with " cold Knife",
CO2 and Nd: YAG lasers and a radiofrequency surgical unit.
J Reprod Med 37: 607-610. |
| 22. |
Goncalves JC, Martins C. Debulking
of skin cancers with radio frequency before cryosurgery.
Dermatol Surg. 1997; 23: 253-256; discussion 256-257. |
| 23. |
Sadick NS, Makino Y. Selective
electro-thermolysis in aesthetic medicine: a review. Lasers
Surg Med. 2004; 34: 91-97. |
| 24. |
Hofmann A, Wustner M, Ciric
B. Radiowave Surgery Case Report. Int J Aest Rest Surg
1996; 4: 131-133. |
| 25. |
Pfenninger JL, DeWitt DE. Radio
frequency surgery. In Pfenninger JL, Fowler GC edits.
Procedures for primary care physicians. Mosby; 1994. St.Louis:
pp 91-101. |
| 26. |
Brown J.S. Radiosurgery. In
Minor Surgery a text and atlas. 3rd edition; London. Chapman
and Hall: pp 324-325. |
|


