|
Knowledge, Attitude and Practice
of Health Care Workers Towards HIV Patients
at Primary Health Care level in southwestern
Saudi Arabia: Twenty-five years after the initial
report
Hasan
M. Alzahrani (1)
Nabil J. Awadalla (2,3)
Rawan A. Hadi (4)
Fahd H. AlTameem (5)
Mona H. Alkhayri (4)
Amal Y. Moshebah (4)
Abdulaziz H. Alqarni (4)
Faisal E. Al-Salateen (4)
Abdulrahman A. Alqahtani (4)
Ahmad A. Mahfouz (2,6)
(1) Department of Emergency Medicine, King Khalid
University Medical City, Abha, Saudi Arabia
(2) Department of Family and Community Medicine,
College of Medicine, King Khalid University,
Abha, Saudi Arabia
(3) Department of Community Medicine, College
of Medicine, Mansoura University, Egypt
(4) Medical Intern/student, College of Medicine,
King Khalid University, Abha
(5) Ahad Rafidah Hospital, Saudi Arabia
(6) Department of Epidemiology, High Institute
of Public Health, Alexandria University, Egypt
Correspondence:
Professor Ahmad A. Mahfouz
Department of Family and Community Medicine,
College of Medicine,
King Khalid University, Abha,
Saudi Arabia
Email: mahfouz2005@gmail.com
Received: April 2019; Accepted: May 2019; Published:
June 1, 2019. Citation: Hasan Alzahrani et al.
Knowledge, Attitude and Practice of Health Care
Workers Towards HIV Patients at Primary Health
Care level in southwestern Saudi Arabia: Twenty-five
years after the initial report. World Family
Medicine. 2019; 17(6): 4-8. DOI: 10.5742MEWFM.2019.93653
|
Abstract
The objective of the present study was
to critically review the existing knowledge,
attitude and practices of HCWs towards
HIV. A cross-sectional study was conducted
in Primary Health Care centers in Abha
and Khamis Mushait cities of Aseer region,
southwestern Saudi Arabia. All HCWs (physicians,
nurses, lab technicians and dentists)
were invited to participate in the study.
A validated self-administered structured
questionnaire was used to collect data
about HCWs’ personal and professional
characteristics; knowledge of HIV infection
and transmission; attitudes towards HIV/AIDS
patients and practices. A total of 372
HCWs were included in the study. Out of
them 23.9% were unable to identify tattooing
and ear piercing as methods for transmission.
A considerable proportion failed to mention
blood transfusion (3.8%), unprotected
sex (6.7%) and uncleanneedles (4.0%) as
possible methods for disease transmission.
Additionally, 36.8% of HCWs have a misconception
that kissing could transmit HIV and about
misbelieved that sharing eating and drinking
utensils (23.1%), swimming pool (18.8%)
and living with AIDs patients (17.5%)
could transmit infection. Stigmatizing
attitude was detected. In conclusion,
poor knowledge and stigmatizing attitude
toward HIV patients are evident in HCWs.
Health education programs should be adopted
to improve HCWs’ knowledge about
transmission mode and combat HIV stigma.
Key words:
HIV/AIDS; healthcare workers, Knowledge,
attitude, stigma, Saudi Arabia
|
According to recent WHO statistics, there were
globally approximately 36.7 million people living
with the human immunodeficiency virus (HIV)
at the end of 2016(1). A recent report by the
Saudi Ministry of Health in 2018, including
data obtained from 20 HIV treatment centers
located in different regions of the Kingdom,
showed that there were 6,256 people living with
HIV and knew their status by the end of 2017,
which is equivalent to 76% of the estimated
number of people living with HIV in Saudi Arabia
(2).
A study performed in 2015 in Jeddah, Saudi Arabia,
among the general population showed lack of
proper knowledge about the disease and more
than 40% think that HIV positive people should
be isolated (3). Similarly, a study among male
dental students in Saudi Arabia showed lack
of knowledge regarding HIV/AIDS transmission
and means for prevention in addition to unfavorable
attitudes towards HIV/AIDS individuals (4).
It was well known that the traditional primary
health care approach of health promotion and
disease prevention that focuses on case-finding,
continuity of care and problem resolution, adapts
well to HIV/AIDS. Primary care is holistic,
patient based, and has as its focus healing
rather than cure. Primary care physicians have
a role in the prevention of HIV infection, in
identifying asymptomatic seropositive people,
in offering early therapeutic interventions,
in the early detection of opportunistic infections
and HIV-related malignancies, and in the ongoing
management of chronic ill-health. There is also
a role for primary care physicians in the psychosocial
management of people with HIV/AIDS, in supporting
those close to the patient, and in educating
the community in general about the social parameters
of HIV/AIDS (5).
In 1995 two published articles addressed the
awareness of HIV among primary health care workers
in Aseer region, Saudi Arabia. They found massive
defects in their knowledge (6, 7). Recent data
regarding knowledge, attitude and practices
of primary healthcare workers in Saudi Arabia
in general and in the Aseer region in particular,
are scarce and even lacking. The aim of the
present work is to study the current knowledge,
attitude and practices (KAP) of primary healthcare
workers towards HIV in Abha and Khamis Mushait
cities of Aseer region, Saudi Arabia.
The present cross-sectional study was conducted
in primary health care centers in Abha and Khamis
Mushait cities of Aseer region, southwestern
Saudi Arabia in 2017. All health care workers
(physicians, nurses, lab technicians and dentists)
were invited to participate in the study. Administrative
personnel not in direct contact with patients’
care were not included.
Data were collected through self-administered
validated structured questionnaire (4). The
questionnaire covered the following four major
areas; demographic data including age, sex,
and nationality, professional data including
type of profession, how long they have been
working, have they provided care towards HIV
patients. The questionnaire included 14 closed-ended
question about knowledge of HIV infection and
transmission. The questionnaire also covered
attitudes regarding treating HIV patients, the
right of health personnel to practice and willingness
to treat.
Data were verified, coded and analyzed using
the Statistical Package for Social Sciences
(SPSS). Frequencies and percentages were used
to present the results.
The study protocol was approved by the research
ethical committee of King Khalid University
(REC#2017-04-03). All the necessary official
permissions were obtained before data collection.
Written consent was taken from the participants.
Collected data were kept strictly confidential
and used only for the research purposes.
Description
of
the
Study
Sample
The
present
study
included
372
Health
Care
Workers
(HCWs).
Almost
half
of
the
study
sample
were
from
Abha
city
(199,
53.5%)
and
the
rest
were
from
Khamis
Mushait
city.
The
majority
of
HCWs
were
females
(228,
61.3%)
and
Saudis
(318,
85.5%).
The
highest
frequent
age
group
was
20-30
years
(181,
48.7%)
followed
by
31
to
40
years
(149,
40.1%).
Dentists
represented
47.6%
(177)
of
the
study
sample
followed
by
physicians
(95,
25.5%)
and
nurses
(78,
21.0%).
The
highest
frequent
period
of
work
was
5-10
years
(160,
43.0%)
followed
by
less
than
5
years
(105,
28.2%).
Failure
to
identify
the
well-known
modes
of
HIV
transmission
Table
1
shows
the
wrong
beliefs
among
HCWs
regarding
HIV
modes
of
transmission.
Regarding
the
failure
to
identify
the
well-known
modes
of
HIV
transmission,
the
highest
failed
mode
to
be
mentioned
was
via
tattoos
or
ear
piercing
(89,
23.9%).
The
least
unidentified
mode
was
blood
transfusion
from
an
infected
person
(14,
3.8%).
On
the
other
hand,
unprotected
sex
and
using
unclean
needles
was
not
mentioned
by
(6.7
%
and
4.0%,
respectively).
No
significant
differences
(P>
0.05)
were
found
by
gender,
nationality,
age,
profession
and
duration
of
employment.
Table
1:
Wrong
Beliefs
in
Modes
of
transmission
of
HIV
as
mentioned
by
PHCCs
workers
in
the
study
area,
2017
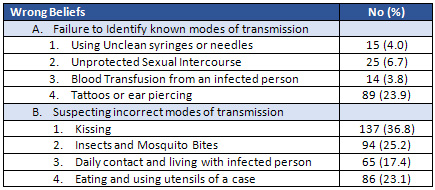
Suspecting
Incorrect
modes
of
HIV
transmission
Regarding
incorrect
knowledge
of
modes
of
HIV
transmission,
the
highest
wrong
modes
mentioned
by
HCWs
was
via
kissing
(137,
36.8%),
followed
by
mosquitos
and
other
insects
bites
(94,
25.2%)
and
via
sharing
plates,
cups,
and
utensils
(86,
23.1%).
The
least
mentioned
incorrect
modes
of
transmission
were
via
sitting
in
a
hot
tub
or
a
swimming
pool
(70,
18.8%),
via
living
with
a
person
with
AIDs
(65,
17.5%)
and
through
the
air
(coughing
or
staying
in
the
same
room
as
someone
infected
with
HIV
(56,
15.1%).
No
significant
differences
(P>
0.05)
were
found
by
gender,
nationality,
age,
profession
and
duration
of
employment.
Other
wrong
knowledge
mentioned
by
HCWs
were
the
presence
of
a
vaccine
that
can
stop
getting
HIV
(38,
10.2%)
and
that
the
people
who
have
been
infected
with
HIV
quickly
show
serious
signs
of
being
infected
(63,
16.9%).
Attitudes
towards
HIV
Patients
Regarding
attitudes
towards
HIV
patients,
the
highest
frequent
response
was
feeling
uncomfortable
when
eating
meals
prepared
by
a
person
with
HIV
(209,
56.2%).
Almost
one
out
of
each
ten
HCWs
(39,
10.5%)
stated
that
HIV
patients
should
be
ashamed
of
themselves,
they
deserve
what
they
get
(32,
8.6%)
and
only
promiscuous
people
get
HIV
(28,
7.5%).
On
the
other
hand,
more
than
two-thirds
of
HCWs
(295,
79.3%)
mentioned
that
they
were
empathetic
with
HIV
patients.
Preventive
activities
during
practice
Regarding
preventive
activities
during
practice,
one-third
of
HCWs
(142,
38.2%)
mentioned
that
spills
of
blood
or
body
fluids
are
decontaminated
by
sodium
hypochlorite
solution.
Two-thirds
(267,
71.8%)
mentioned
that
the
work
provides
protective
equipment
for
HCWs
to
prevent
the
spread
of
HIV
and
identified
the
use
of
liquid
detergent
and
running
for
hand
washing
to
prevent
the
spread
of
HIV
(243,
65.3%).
|

