|
An investigation into the outcomes
of biliary atresia in Sulaimani, Iraq
Adnan Mohammed Hasan (1)
Mahdi Aziz Hama Marif (2)
Mohammed Fadhil Abbas (3)
(1) Professor
of Pediatrics, College of Medicine, University
of Sulaimani
(2) Pediatric Surgeon, M.B.Ch.B. - D.G.S. -
F.I.B.M.S, College of Medicine, University of
Sulaimani
(3) Pediatrician, M.B.Ch.B. - CABP – FIBMS
Corresponding author:
Adnan
Mohammed Hasan
Professor of Pediatrics, College of Medicine,
University of Sulaimani
Kurdistan, Iraq
Email: adnan.hasan@univsul.edu.iq
Received: February 15, 2019; Accepted: March
2019; Published: April 1, 2019
Citation: Adnan Mohammed Hasan, Mahdi Aziz Hama
Marif, Mohammed Fadhil Abbas. An investigation
into the outcomes of biliary atresia in Sulaimani,
Iraq. World Family Medicine. 2019; 17(4): 11-16.
DOI: 10.5742MEWFM.2019.93631
|
Abstract
Background and objective:
Biliary atresia (BA) is a rare childhood
disease that is associated with renal
failure, cirrhosis, and death. This disease
is typically treated through Kasai portoenterostomy
which can be associated with some preoperative
and postoperative complications. In this
regard, the present study was aimed at
investigating the relationship between
early diagnosis of biliary atresia and
its outcomes and complications following
Kasai portoenterostomy.
Methods:
In a retrospective study, 20 infants with
biliary atresia who were treated through
Kasai portoenterostomy or who did not
receive treatment, were investigated.
Required data were collected from their
files and analyzed using Pearson Chi-square
test through SPSS 20.0.
Results: The results of the present
study indicated liver biopsy was an accurate
method to diagnose biliary atresia. Stool
color was found to be an important clinical
indicator on presentation of BA. It was
also seen that both groups of infants
who received Kasai treatment did not develop
cholangitis. Also, liver cirrhosis and
portal hypertension were complications
that were seen in both groups of patients
who received and did not receive Kasai
treatment. There was a significant relationship
between early diagnosis of BA and survival
more than 6 months. However, there was
no significant relationship between receiving
Kasai treatment and mortality rate.
Conclusion: Infants with biliary
atresia survive more in cases of early
diagnosis and referral for surgery; therefore,
pediatric centers are highly recommended
to perform evaluations for BA once they
notice neonatal jaundice lasting more
than 2 weeks. Effective postoperative
care is also recommended for favorable
outcomes of Kasai portoenterostomy.
Key words:
biliary atresia, Kasai portoenterostomy,
renal failure, retrospective study,
the Kurdistan Region of Iraq
|
Biliary atresia (BA) is a rare pediatric cholangio-destructive
disease that has adverse effects on both the
extra- and intra-hepatic biliary tract, and
if it is not treated in a timely manner, renal
failure, cirrhosis, and death can be among its
outcomes [1, 2]. The prevalence of this disease
has been reported to vary from 1 out of 8,000
to 1 out of 18,000 live births [3]. BA is usually
non-syndromic and has an isolated anomaly [4];
however, it is sometimes associated with various
congenital anomalies such as absence of cardiac
defects, retro-hepatic inferior vena cava, preduodenal
portal vein, situs inversus, asplenia, or polysplenia
[5, 6].
Development of BA has been related to different
factors; however, recent studies have reported
that it is likely to be related to gene mutations
[7]. During the first weeks of life, children
with BA do not have any clinical signs, but
2-6 weeks after birth, they become increasingly
jaundiced [8]. Other clinical signs of BA can
include liver growth in size and firmness, anemia,
malnutrition diarrhea, prolonged bleeding from
the umbilical stump, and splenomegaly [9].
Numerous methods have been proposed and tried
for the diagnosis of BA in neonates; however,
very few of them have acceptable accuracy. Liver
biopsy has been reported as the most helpful
examination for BA with a diagnostic accuracy
of >90%. It should also be noted that liver
biopsy is most accurate if it is performed after
6 weeks of age because most features of BA may
be absent before this age, and in that case,
an intra-operative cholangiogram may be required
[10].
Kasai portoenterostomy, also called hepatoportoenterostomy,
was proposed by Morio Kasai in 1959 as an operative
treatment for biliary obstruction in infants
with non-correctable atresia [11]. In order
to stimulate bile flow, reduce hepatic inflammation,
prevent postoperative cholangitis, and decrease
progressive fibrosis associated with BA, adjuvant
medical therapy is commonly conducted after
Kasai portoenterostomy [12]. Liver transplantation
is used as a treatment method for those cases
where the liver is severely impaired due to
delayed diagnosis [13].
Although Kasai portoenterostomy is reported
to be the most preferred treatment for BA, it
has been associated with some preoperative complications
such as ventilator associated pneumonia, electrolyte
imbalance, DIC, hemorrhage, and sepsis [14]
and postoperative complications including portal
hypertension, liver failure, upper gastrointestinal
bleed, and cholangitis [15].
The present study was carried out in the Pediatrics
Teaching Hospital, Shar Hospital, and Shorsh
Hospital in Sulaimani, the Kurdistan Region
of Iraq, to examine the relationship between
early diagnosis of biliary atresia and its outcomes
and complications following Kasai portoenterostomy.
The present investigation was a retrospective
study that was carried out on 20 infants with
biliary atresia hospitalized in the Pediatrics
Teaching Hospital of Sulaimani, the Kurdistan
Region of Iraq. Data collection was carried
out from September 1, 2012 to September 1, 2016.
Convenience sampling was utilized to select
the study sample. Both groups of infants who
had received Kasai portoenterostomy (Kasai group)
and those who had received no treatment (no-treatment
group) were included in the study. After the
selection of the infants, their demographic
and pediatric characteristics including age,
sex, place of residence, weight at the time
of diagnosis, associated congenital abnormalities,
age at the time of evaluation, color of stool,
and color of urine were obtained from their
files; as well as data on their liver enzymes
at diagnosis time, ultrasonographic findings,
and liver biopsy findings. In addition, data
on complications and outcomes of BA were obtained
from the patients who had undergone Kasai portoenterostomy
and from those who had not. All required data
of the surviving infants were obtained from
the GIT department in the Pediatrics Teaching
Hospital and Pediatric Surgical Department in
Shar Hospital of Sulaimani, the Kurdistan Region
of Iraq. Moreover, data of the infants who had
died were obtained from the Histopathological
Department of Shorsh Hospital, Sulaimani.
The collected data were analyzed using Pearson
Chi-square test through Statistics Package for
Social Science (SPSS) version 21. The results
are expressed in form of numbers and percentages.
The level of statistical significance was set
at p<0.05.
The study was approved by the Ethics and Scientific
Committee of College of Medicine, University
of Sulaimani. Moreover, the infants’ parents
were contacted to obtain their verbal consent
for participation in the study.
The
results
of
the
present
study
revealed
that
of
the
20
infants
with
BA,
14
were
female
(70%)
and
6
were
male
(30%).
They
also
showed
that
the
infants’
age
during
liver
biopsy
was
less
than
1
month
(1
infant),
1-2
months
(6
infants),
and
more
than
2
months
(13
infants).
Moreover,
it
was
seen
that
14
infants
weighed
more
than
3.5
kg
and
6
less
than
3.5
kg
(See
Table
1).Regarding
the
patients’
clinical
characteristics,
the
results
indicated
that
3
infants
had
clinical
presentation
before
6
weeks
of
age
(15%)
and
17
after
6
weeks
of
life
(85%).
It
was
also
observed
that
the
stool
color
was
pale
in
18
infants
(90%)
and
normal
in
2
patients
(10%).
Moreover,
the
urine
color
was
dark
in
11
infants
(55%)
and
normal
in
9
patients
(9%)
(See
Table
2).
Table
1:
The
infants’
demographic
characteristics
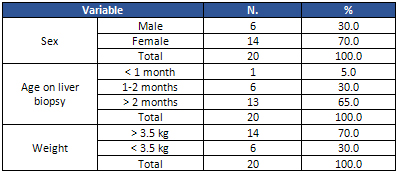
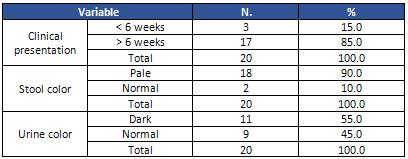
Table
2:
The
infants’
clinical
features
With
regard
to
the
laboratory
findings
of
the
patients,
the
results
demonstrated
that
liver
enzymes
increased
2
fold
in
16
infants
(80%)
and
less
than
2
fold
in
4
cases
(20%).
The
ultrasound
findings
revealed
that
7
infants
had
triangular
cords
(35%)
and
13
had
gallbladder
of
shorter
than
1.5
cm
(65%).
In
addition,
liver
biopsy
findings
showed
that
Lee
Index
score
was
more
than
7
in
14
infants
(70%)
and
unknown
in
6
patients
(30%)
(See
Table
3).According
to
the
results,
of
the
8
infants
who
had
received
Kasai
portoenterostomy,
7
had
cholangitis
as
a
postoperative
complication.
On
the
other
hand,
none
of
the
infants
who
did
not
receive
Kasai
portoenterostomy
developed
postoperative
cholangitis.
In
this
regard,
the
two
groups
were
significantly
different
(p=0.000).
The
two
groups
were
not
significantly
different
in
terms
of
developing
liver
cirrhosis;
6
infants
in
the
Kasai
group
and
11
in
the
no-treatment
group
had
it
(p=0.306).
Also,
the
two
groups
were
not
significantly
different
in
terms
of
portal
hypertension;
4
patients
in
the
Kasai
group
and
9
in
the
no-treatment
group
had
it
(p=0.251).
The
results
also
indicated
that
the
two
groups
were
not
different
in
the
two
groups
regarding
failure
to
thrive;
5
patients
in
each
group
failed
to
thrive
(p=0.361).
Moreover,
7
infants
in
the
Kasai
group
and
12
in
the
no-treatment
group
died,
but
this
difference
was
not
significant
(p=0.209)
(See
Table
4).
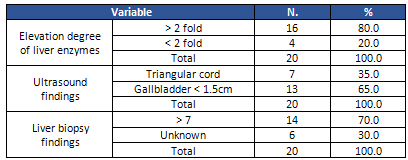
Table
3:
The
infants’
laboratory
findings
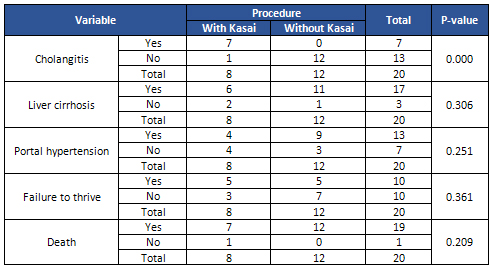
Table
4:
BA
outcomes
and
complications
in
the
two
groups
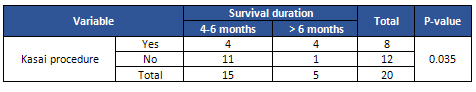
The
results
also
indicated
that
in
the
group
with
Kasai
treatment,
4
infants
survived
4-6
months
and
6
more
than
6
months,
and
in
the
group
without
Kasai
treatment,
11
patients
survived
4-6
months
and
1
more
than
6
months.
The
two
groups
were
significantly
different
in
this
regard
(p<0.05),
and
the
infants
who
received
Kasai
treatment
survived
longer
(See
Table
5).
Table
5:
Survival
duration
in
the
two
groups
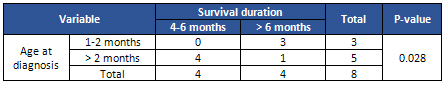
According
to
the
results
regarding
the
association
between
early/late
diagnosis
of
BA
and
the
patients’
survival
duration,
all
of
the
patients
who
were
diagnosed
during
1-2
months
of
age
survived
beyond
6
months,
while
only
1
of
the
4
infants
who
were
diagnosed
after
2
months
of
age
survived
more
than
6
months.
This
difference
was
significant
(p<0.05)
(See
Table
6).
Table
6:
Association
between
survival
duration
and
late/early
diagnosis
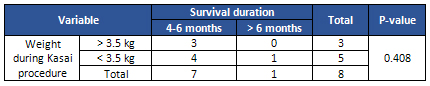
Furthermore,
regarding
the
association
between
the
infants’
weight
during
Kasai
treatment
and
their
mortality,
the
results
revealed
that
none
of
the
3
patients
who
weighed
over
3.5
kg
died,
while
1
of
the
4
weighing
less
than
3.5
kg
died;
however,
this
difference
was
not
significant
(p>0.05)
(See
Table
7).
Table
7:
Association
between
survival
duration
and
weight
during
Kasai
treatment
|

