|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor)
DOI:10.5742/MEWFM.2019.93610
|
........................................................
|
|
Editorial
Dr.
Abdulrazak Abyad
DOI: 10.5742/MEWFM.2019.93623
Original Contribution
Self-monitoring
of Blood Glucose Among Type-2 Diabetic Patients:
An Analytical Cross-Sectional Study
[pdf]
Ahmed S. Alzahrani, Rishi K. Bharti, Hassan
M. Al-musa, Shweta Chaudhary
DOI: 10.5742/MEWFM.2019.93624
White
coat hypertension may actually be an acute phase
reactant in the body
[pdf]
Mehmet Rami Helvaci, Orhan Ayyildiz, Orhan Ekrem
Muftuoglu, Mehmet Gundogdu, Abdulrazak Abyad,
Lesley Pocock
DOI: 10.5742/MEWFM.2019.93625
Case Report
An
Unusual Persistent Mullerian Duct Syndrome in
a child in Abha city: A Case Report
[pdf]
Youssef Ali Mohamad Alqahtani, Abdulrazak Tamim
Abdulrazak, Hessa Gilban, Rasha Mirdad, Ashwaq
Y. Asiri, Rishi Kumar Bharti, Shweta Chaudhary
DOI: 10.5742/MEWFM.2019.93628
Population and Community
Studies
Prevalence
of abdominal obesity and its associated comorbid
condition in adult Yemeni people of Sana’a
City
[pdf]
Mohammed Ahmed Bamashmos
DOI: 10.5742/MEWFM.2019.93626
Smoking
may even cause irritable bowel syndrome
[pdf]
Mehmet Rami Helvaci, Guner Dede, Yasin Yildirim,
Semih Salaz, Abdulrazak Abyad, Lesley Pocock
DOI: 10.5742/MEWFM.2019.93629
Systematic
literature review on early onset dementia
[pdf]
Wendy Eskine
DOI: 10.5742/MEWFM.2019.93627
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
AUSTRALIA
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| March 2019 - Volume
17, Issue 3 |
|
|
White coat hypertension may
actually be an acute phase reactant in the body
Mehmet Rami Helvaci (1)
Orhan Ayyildiz (1)
Orhan Ekrem Muftuoglu (1)
Mehmet Gundogdu
(1)
Abdulrazak Abyad (2)
Lesley Pocock (3)
(1) Professor of Internal Medicine, MD
(2) Middle-East Academy for Medicine of Aging,
MD, MPH, MBA, AGSF
(3) medi-WORLD International
Corresponding author:
Mehmet
Rami Helvaci, MD
07400, ALANYA, Turkey
Phone: 00-90-506-4708759
Email: mramihelvaci@hotmail.com
|
Abstract
Background: We tried
to understand the significance of white
coat hypertension (WCH), clinically.
Methods: We took consecutive underweight
patients in the first phase, and age-matched
consecutive patients with normal weight,
overweight, and obesity in the second
phase of the study.
Results: Although we were able
to detect 50 cases in the underweight
group with a mean age of 24.7 years, we
were only able to detect nine age-matched
cases in the obesity group, thus the obesity
group was not taken for comparison. There
were gradual and statistically significant
increases in the prevalence of WCH beside
the gradual and significant decreases
in the sustained normotension (NT) from
the underweight towards the normal weight
and overweight groups. Eventually, only
31.8% of the overweight cases had sustained
NT although they had very young mean age.
Conclusions: Due to the gradually
increased prevalence of WCH from the underweight
towards the normal weight and overweight
groups and the very low prevalence of
sustained NT in the overweight group despite
their very young mean ageand the already
known increased prevalence of hypertension,
impaired fasting glucose, impaired glucose
tolerance, type 2 diabetes mellitus, hypertriglyceridemia,
hyperbetalipoproteinemia, dyslipidemia,
coronary artery disease, chronic obstructive
pulmonary disease, cirrhosis, chronic
renal disease, and stroke and an increased
all-cause mortality rate in the same direction,
WCH may actually be an acute phase reactant,
mainly alarming overweight and obesity
and many associated health problems
in future.
Key words:
White coat hypertension, acute phase reactant,
overweight, obesity
|
In recent years, overweight and obesity have
become major health problems particularly in
developed countries. For example, 30% of adults
in the United States can be classified as obese
(1). Overweight and obesity are characterized
by increased mass of adipose cells that result
from a systemic imbalance between food intake
and energy expenditure, and they are associated
with increased levels of inflammatory parameters
and many systemic disorders including white
coat hypertension (WCH), hypertension (HT),
impaired fasting glucose (IFG), impaired glucose
tolerance (IGT), type 2 diabetes mellitus (DM),
hypertriglyceridemia, hyperbetalipoproteinemia,
dyslipidemia, coronary artery disease (CAD),
chronic obstructive pulmonary disease (COPD),
cirrhosis, chronic renal disease (CRD), stroke,
and an increased all-cause mortality rate (2-5).
Additionally, obesity is highly correlated with
dietary intake of increased calories and fat,
both of which were linked to several types of
cancers (6). For example, in a recent study
performed among 900,000 people it was found
that obese individuals were more likely to die
from a number of cancers including breast, colon,
and prostate (7). On the other hand, cardiovascular
death, myocardial infarction, and stroke are
the most common causes of deaths particularly
in the developed countries again, and most of
them are related with increased blood pressure
(BP) (8). Therefore BP control is the mainstay
for prevention of cardiovascular deaths. But
diagnosis and management of HT is difficult
due to the fact that BP varies greatly depending
on physical and mental stresses. WCH is a well-known
clinical entity defined as a persistently elevated
BP in the doctor's office whereas normal in
other conditions, and prognostic significance
of it remains controversial (9, 10). For instance,
it was reported in an Ohasama study that WCH
is a risk factor for development of home HT
(11). Similarly, 46.9% of cases with WCH versus
22.2% of cases with sustained normotension (NT)
progressed to home HT in an eight-year follow
up study (12). So the results demonstrated that
WCH is a transitional condition eventually terminating
with home HT. Additionally, intima-media thickness
and cross-sectional area of carotid artery were
found as similar in patients with WCH and HT,
which were significantly higher than the sustained
NT cases so authors concluded that there is
target organ damage in WCH therefore it should
not be considered as an innocent trait, clinically
(13). Similarly, complication risks of WCH were
different from subjects with sustained NT in
another study (14). On the other hand, there
was not any proof that WCH exhibits a clearly
higher risk for cardiovascular events in the
above 7.4-year follow up study (10). So most
of the already performed studies about WCH have
just focused on the progression to home HT in
time or whether WCH causes any target organ
damage or not. We therefore tried to understand
some other possible clinical consequences of
WCH in the present study.
The
study
was
performed
in
the
Internal
Medicine
Polyclinic
of
the
Dumlupinar
University
between
August
2005
and
August
2006
in
two
phases.
In
the
first
phase,
we
took
consecutive
underweight
patients
between
the
ages
of
15
and
70
years
to
be
able
to
see
the
possible
consequences
of
weight
on
BP
and
to
avoid
debility
induced
weight
loss
in
elders.
In
the
second
phase,
age-matched
consecutive
cases
with
normal
weight,
overweight,
and
obesity
were
detected.
Their
medical
histories
including
smoking
habit
and
medications
were
learnt,
and
a
routine
check
up
procedure
was
performed.
Current
regular
smokers
at
least
for
the
last
6
months
and
cases
with
a
previous
smoking
history
of
at
least
five
pack-years
were
accepted
as
smokers,
and
cigar
or
pipe
smokers
were
excluded.
Insulin
using
diabetics
and
patients
with
devastating
illnesses
including
malignancies,
acute
or
chronic
renal
failure,
chronic
liver
diseases,
hyper-
or
hypothyroidism,
and
heart
failure
were
excluded
to
avoid
their
possible
effects
on
weight.
Body
mass
index
(BMI)
of
each
case
was
calculated
by
the
measurements
of
the
Same
Physician
instead
of
verbal
expressions.
Weight
in
kilograms
is
divided
by
height
in
meters
squared,
and
underweight
is
defined
as
a
BMI
of
lower
than
18.5,
normal
weight
between
18.5-24.9,
overweight
between
25-29.9,
and
obesity
as
a
BMI
of
30.0
kg/m(2)
or
higher
(15).
Office
blood
pressure
(OBP)
was
checked
after
a
5-minute
rest
in
seated
position
with
the
mercury
sphygmomanometer
on
three
visits,
and
no
smoking
was
permitted
during
the
previous
2
hours.
A
10-day
twice
daily
measurement
of
blood
pressure
at
home
(HBP)
was
obtained
in
all
cases
even
in
normotensives
in
the
office
due
to
the
risk
of
masked
HT
after
a
10-minute
education
session
about
proper
BP
measurement
techniques
(16).
The
education
included
recommendation
of
upper
arm
while
discouraging
wrist
and
finger
devices,
using
a
standard
adult
cuff
with
bladder
sizes
of
12
x
26
cm
for
arm
circumferences
up
to
33
cm
in
length
and
a
large
adult
cuff
with
bladder
sizes
of
12
x
40
cm
for
arm
circumferences
up
to
50
cm
in
length,
and
taking
a
rest
at
least
for
a
period
of
5
minutes
in
the
seated
position
before
measurement.
An
additional
24-hour
ambulatory
blood
pressure
monitoring
(ABP)
was
not
required
due
to
the
equal
effectiveness
of
the
ABP
and
HBP
measurement
techniques
for
the
diagnosis
of
WCH
and
HT
(17,
18).
Eventually,
HT
is
defined
as
a
BP
of
135/85
mmHg
or
greater
on
mean
HBP
values
(16).
WCH
is
defined
as
an
OBP
of
140/90
mmHg
or
greater,
but
a
mean
HBP
value
of
lower
than
135/85
mmHg,
sustained
NT
as
an
OBP
of
lower
than
140/90
mmHg
together
with
an
average
HBP
of
lower
than
135/85
mmHg,
and
masked
HT
as
an
OBP
of
lower
than
140/90
mmHg
but
a
mean
HBP
of
135/85
mmHg
or
greater
(16).
Prevalence
of
smoking,
sustained
NT,
WCH,
and
HT
were
detected
in
each
group,
and
results
were
compared
in
between.
Mann-Whitney
U
test,
Independent-Samples
T
test,
and
comparison
of
proportions
were
used
as
the
methods
of
statistical
analyses.
The
study
included
417
cases
(217
females),
totally.
The
first
and
second
phases
took
periods
of
eight
and
four
months,
respectively.
During
the
first
phase,
we
were
able
to
detect
50
cases
(31
females)
with
underweight.
On
the
other
hand,
we
were
able
to
detect
just
nine
cases
(six
females)
in
the
obesity
group
during
the
second
phase
therefore
the
obesity
group
was
not
taken
for
comparison.
Despite
the
nonsignificant
differences
according
to
age
in
between,
female
ratios
were
detected
as
62.0%
(31
cases),
53.9%
(149
cases),
and
40.6%
(37
cases)
in
the
underweight,
normal
weight,
and
overweight
groups,
respectively
(Table
1).
So
there
was
a
statistically
significant
(p<0.05)
male
predominance
in
the
overweight
group.
Beside
that
there
were
nonsignificant
differences
according
to
the
prevalence
of
smoking
between
the
three
groups.
There
were
gradual
and
statistically
significant
increases
in
the
prevalence
of
WCH
beside
the
gradual
and
significant
decreases
in
the
sustained
NT
from
the
underweight
towards
the
normal
weight
and
overweight
groups.
Eventually,
the
prevalence
of
WCH
reached
68.1%
(62
cases)
in
the
overweight
group.
In
other
words,
only
31.8%
(29
cases)
of
the
overweight
group
had
sustained
NT
despite
the
very
young
mean
age
of
the
patients.
Probably
due
to
the
very
young
mean
age,
there
was
only
one
case
of
HT
among
the
study
cases.
Table
1:
Blood
pressure
variability
of
the
study
cases
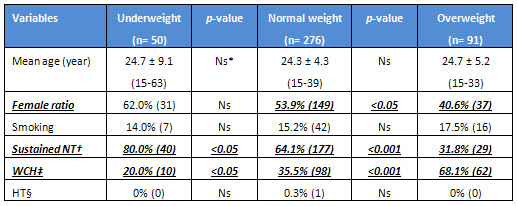
*Nonsignificant
(p>0.05)
†Normotension
‡White
coat
hypertension
§Hypertension
Click
here
for
Table
2:
Comparison
of
the
previous
study
cases
| | |

