|
Assessment of behaviors,
risk factors of Diabetic foot ulcer and footwear
safety among diabetic patients in primary care
setting, Abu Dhabi, UAE
Osama Moheb
Ibrahim Mohamed (1)
Nwanneka E. O. Ofiaeli (2)
Adnan Syeed (3)
Amira Elhassan (4)
Mona Al Tunaiji (5)
Khuloud Al Hammadi (6)
Maryam Al Ali (7)
(1) MBBCh,
MSc, MD FM, (MSc, UK), Consultant Family Medicine,
Ambulatory Health Services, SEHA corporate,
Abu Dhabi, UAE
(2) MBBS, MRCGP (UK), DFFP(UK), Consultant Family
Medicine, Ambulatory Health Services, SEHA corporate,
Abu Dhabi, UAE
(3) MBBS, MRCS, MRCGP(UK), Consultant Family
Medicine, Ambulatory Health Services, SEHA corporate,
Abu Dhabi, UAE
(4) Consultant Family Medicine, Ambulatory Health
Services, SEHA corporate, Abu Dhabi, UAE
(5) Consultant Family Medicine, Ambulatory Health
Services, SEHA corporate, Abu Dhabi, UAE
(6) Khuloud Al Hammady, Family Medicine residents,
SKMC, SEHA corporate, Abu Dhabi, UAE
(7) Maryam Al Ali , Family medicine resident
SKMC, SEHA corporate, Abu Dhabi, UAE
Correspondence:
Dr. Osama
Moheb Ibrahim Mohamed
Consultant Family Medicine,
Ambulatory Health Services,
SEHA corporate,
Abu Dhabi,
UAE
Email: osamamohebibrahim@gmail.com
|
Abstract
Background: Diabetes
mellitus accounts for 5.2 % of all deaths
world-wide. UAE had a prevalence of 19.3%
in 2015. It is estimated that by 2025
this will rise to more than 21.5%(1).
In patients with Diabetes 60-70% will
develop peripheral neuropathy, (2) and
25% will develop a foot ulcer(3). The
yearly incidence of diabetic foot ulcers
ranges from 2 to 32%. More than half of
all foot ulcers (wounds) will become infected,
requiring hospitalization and 20% of infections
result in amputation.(5) History of diabetic
foot ulcer results in a 40% greater 10-year
mortality in diabetic patients(10). Diabetic
foot ulcers can be prevented and researchers
have established that up to 85% of amputations
can be prevented(15).
Objective: The
Aim of this study was to assess behaviors,
prevalence of diabetic foot risk factors
and safety of footwear among diabetic
patients.
Methods: A
cross-sectional study was conducted in
an ambulatory healthcare clinic. Self-reported
questionnaire was used to assess foot
care behaviors,'. Inlow's 60-second Diabetic
Foot Screen was used to examine foot.
ADA risk classification was used for risk
assessment. Furthermore descriptive statistics
were employed to assess the predicators
of practice of diabetic foot care.
Results: The
total patients were 74; the majority of
respondents were local UAE patients 46
(71.88%) with diabetes duration of 8.8
years. Mean age was 59.1±10.11
years; male to female ratio was nearly
similar. Mean A1c level was 7.45 ±1.81
and only 21 out of 50 (42%) patients had
their HbA1c controlled (<7). 80.28%
of patients completed at least elementary
school. The frequency patients received
foot care education and foot examination
were 60 (81.08%) and 55 (74.32 %) respectively;
42 (55.56%) walked barefoot indoors, 43
(56.97%) wore shoes without socks, 35(47.95%)
tested the water temperature with hand
/ elbow before taking a bath or a shower,
50 (68.49%) self-treated corns or calluses
with a blade, 67 (90.54%) wore sandals,
almost all 73 (98.93) relied on feeling
the fit of the shoes when buying a new
pair; overall shoes assessment was improper
shoes in 64 (86.49 %). There was callus
formation in 30 (42.26%), foot deformity
in 11 (15.28%), loss of sensation by monofilament
in 0 to 9 sites, out of 10 in foot 26
(40.55%), absence of dorsalis pedes pulse
in 10 (13.89%) and 40 % were classified
at risk category 1 to develop foot ulcer.
Conclusion: Foot care practices
are still substandard among diabetic patients.
There was a gap between what patient receive
in foot education by health care provider
and what patients did in real practice.
Potential harmful foot care behaviors
were high and protective foot care practice
was low. Finally there were one or more
risk factors of diabetic foot ulcer in
the majority of patients.
Key words:
Diabetes, Diabetic foot, diabetic
neuropathy, foot deformity, proper shoes
for diabetics, Abu Dhabi
|
Diabetes mellitus (DM) is a major emerging
clinical and public health problem accounting
currently for 5.2 % of all deaths world-wide.
According to International Diabetes Federation
(IDF), prevalence of DM in UAE was 19.3 % in
2015. According to WHO estimates (2007), 190
million people suffer from diabetes world-wide
and about 330 million are expected to be diabetic
by the year 2025. UAE had been estimated to
be the 10th country in the prevalence of Diabetes
with prevalence of 19.6. Recent changes in physical
activity and dietary patterns have promoted
the development of diabetes and if different
preventive and control activities are not adopted,
by the year 2025 more than 21.5% of the population
above 20 years old) will have diabetes(1).
About 60-70% of those with diabetes will develop
peripheral neuropathy, or lose sensation in
their feet(2). Up to 25% of those with diabetes
will develop a foot ulcer(3). The yearly incidence
of diabetic foot ulcers ranges from 2% to 32%,
depending on ADA risk classification(4). More
than half of all foot ulcers (wounds) will become
infected, requiring hospitalization and 20%
of infections result in amputation(5). Diabetes
contributes to approximately 80% of the 120,000
non-traumatic amputations performed yearly in
the United States(6). "Every 20 seconds,
somewhere in the world, a limb is lost as a
consequence of diabetes"(7). After a major
amputation, 50% of people will have their other
limb amputated within 2 years(7).
The relative 5-year mortality rate after limb
amputation is 68%. When compared with cancer,
it is second only to lung cancer (86%) (Colorectal
cancer 39%, Breast cancer 23%, Hodgkin's disease
18%, Prostate cancer 8%). People with a history
of a diabetic foot ulcer have a 40% greater
10-year mortality than people with diabetes
alone(8) Every 30 minutes a limb is lost due
to a landmine. Every 30 seconds, a limb is lost
due to diabetes(9). Having a wound immediately
doubles one's chances of dying at 10 years compared
with someone without diabetes(9). Diabetic foot
ulcers double mortality and heart attack risk
while increasing risk for stroke by 40% (10);
each $1 invested in care by a podiatrist for
people with diabetes results in $27 to $51 of
healthcare savings(11).
Diabetic foot ulcers as a result of neuropathy
or ischemia are common. In developed countries,
up to five per cent of people with diabetes
have foot ulcers, and one in every six people
with diabetes will have an ulcer during their
lifetime. Foot problems are the most common
cause of admission to hospital for people with
diabetes. In developing countries, foot problems
related to diabetes are thought to be even more
common. Without action, global amputations rates
will continue to rise(12).
In most cases, however, diabetic foot ulcers
and amputations can be prevented. Researchers
have established that between 49% and 85% of
all amputations can be prevented. It is imperative,
therefore, that healthcare professionals, policymakers
and diabetes representative organizations undertake
concerted action to ensure that diabetic foot
care is structured as effectively as local resources
will allow. This will facilitate improvements
in foot care for people with diabetes throughout
the world and bring about a reduction in diabetic-foot-related
morbidity and mortality(13).
Diabetic foot is one of the common disabling
diabetes complications leading to amputation
and fortunately 85% of amputation is preventable
by a cost-effective foot care. Diabetic foot
examination is one of the key performance indicators
(KPI) by Health Authority / SEHA Corporation
so more data is needed among the Emirati diabetics
to be used as a database for formulation of
an organized structured foot care intervention
program; this study is aiming to provide a database
for foot care intervention program.
1-To assess the behaviors of patients with
diabetes with respect to their foot care,
2-To assess the prevalence of diabetic foot
risk among diabetic patients, and
3-To examine the safety of footwear for diabetic
patients
A-Study Design: A cross sectional study
was conducted in a primary care clinic, Ambulatory
Health Care.
B-Study Population:
1-Patient population: Patients
who presented to Al Bateen Family Medicine Clinic
with physician-diagnosed Diabetes based on the
A1C above or equal 6.5% and who met the inclusion
and exclusion criteria, were included in the
study
2-Inclusion Criteria were: patients
suffering from diabetes for at least 3 years,
Adult (above 18) diabetic patients
3-Exclusion criteria were: Patient
with current Diabetic foot ulcer, History of
amputation, Charcot's foot, congenital foot
deformities, Visual impairment, Physically independent.
Informed consent was obtained and study proposal
was approved by research committee, ambulatory
health care.
4-Sample size: Based on patients'
inclusion and exclusion criteria and 11% anticipated
frequency of "proper foot care" at
95% confidence interval, sample size was estimated
to be 74 diabetic patients(14)..
C- Statistical Analysis: The data were
entered into Excel spreadsheet and analyzed
using SPSS(17) for Windows. Analysis used simple
frequency distribution of key variables in the
study. Comparison was made with selected base
line demographic variable age gender, educational
status and socioeconomic status. The level of
significance was set at p < 0.05. Data was
collected by the investigators for consistency.
For ethical purposes foot care education was
promoted among unaware diabetic patients who
participated in the study.
D-Methods of Data Collection:
1-Demographic data (age, sex,
education, employment status, duration of diabetes,
A1c level, smoking status).
2-Evaluation of Foot Care behaviour:
Patients were asked to fill Vileikyte and colleagues
(15) questionnaires for assessment of foot-care
behavior, (Figure 1). The content of the tool
was based on international "diabetic foot
care guidelines"(16-17). The seventeen-item
questionnaire is split into two behavioral subscales:
nine items pertaining to preventative behavior
and eight items to potentially damaging behavior.
Responses were rated on two different scales:
a 6-point scale for "during the past week"
questions (twice a day, daily, every other day,
twice a week, once a week, or never) and on
a four-point scale for "in general"
questions (always, most of the time, occasionally,
or never).
3- Foot Examination: Inlow's 60-second
Diabetic Foot Screen was used to examine foot(18),
(Figure 2)
4-Foot risk classification : ADA
foot risk classification was used for risk assessment
(Figure3)(19)
5-Foot-wear assessment checklist (Figure
4). A foot examination check list was also developed
which scored on the presence or absence of proper
footwear and included footwear recommendations
prepared by the International Working Group
on the Diabetic Foot; any abnormal character
of the footwear in the checklist indicated improper
footwear (20).
Click here for Figure
1: The behavior questions
Click here for Figure
2: Risk classification based on the comprehensive
foot examination
Click here for Figure
3
Click here for Figure
4: Footwear Assessment Checklist
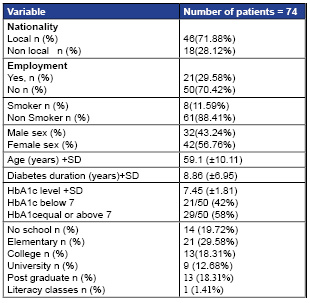
Characteristics of the participants are reported
in Table 1. A higher percentage of the participants
were local and were diagnosed with type 2 diabetes,
and there were a high proportion of participants
who did not complete secondary school.
Table 1: Characteristics of Study populations
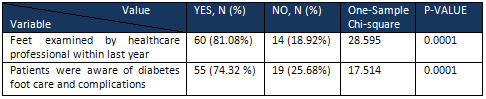
There were a significantly higher proportion
of study population who received foot care health
education and feet were examined by healthcare
personnel as shown in Table 2.
Table 2: Frequency patient received foot
care education and foot examination
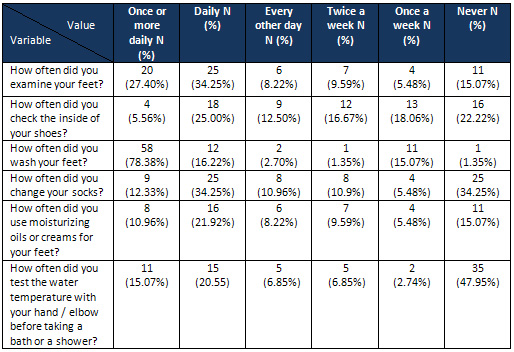
Forty-two patients (55.56%) walked barefoot
indoors, 43 (56.97%) wear shoes without socks,
35 (47.95%) did you test the water temperature
with hand / elbow before taking a bath or a
shower, 50 (68.49%) self-treated corns or calluses
with a blade, 67 (90.54%) wear sandals as shown
in Table 3.
Table 3: Frequency of patients' Diabetic
foot preventative behaviors during the past
week
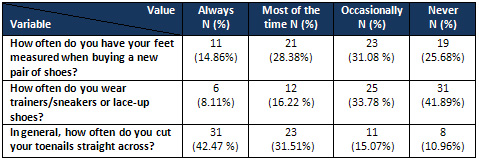
Only 41.89 of patients often wear trainers/sneakers
or lace-up shoes, Table 4.
Table 4: Frequency of patients' Diabetic
foot preventative behaviors during the past
week
Thirty two percent and 31% did not walk bare
foot or wear shoes without socks respectively,
Table 5.
Click here for Table
5: Frequency of patients' Diabetic Foot potentially
damaging behaviors during the past week
Table 6: Frequency of patients' Diabetic
Foot potentially damaging behaviors during the
past week
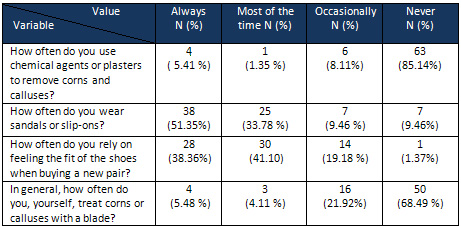
Table 7: Footwear Assessment among participants
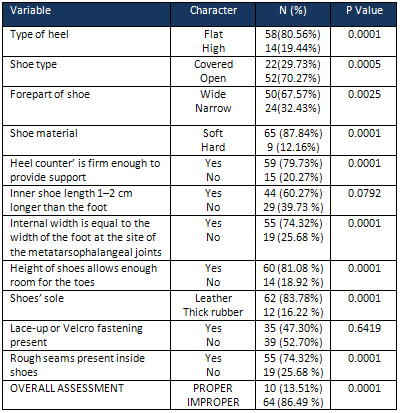
There was callus formation in 30 (42.26%), foot
deformity in11 (15.28%), loss of sensation by
monofilament in 0 to 9 sites out of 10 in foot
26 (40.55%), absence of dorsalis pedes pulse
in 10 (13.89%) and 40 % were classified at risk
category 1 to develop foot ulcer. as shown in
Table 8.
Table 8: 60-second Diabetic Foot Screen
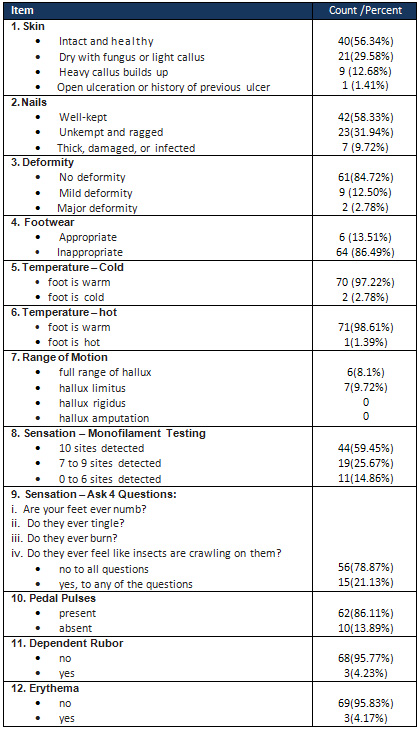
Twenty-one (33.79%) of study population were
classified to have either risk categories 1,
2 or 3 to develop foot ulcer, Table 9.
Table 9: Risk classification based on foot
examination
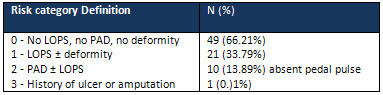
LOPS; loss of peripheral sensation, PAD; peripheral
arterial disease
A total 74 patients were recruited; the majority
of respondents were local UAE patients 46 (71.88%)
with diabetes duration of 8.8 years; mean age
was 59.1±10.11 years; male to female
ratio was nearly similar; mean A1c level was
7.45 ±1.81 and 80.28 of patients completed
at least elementary school. The frequency as
to which patients received foot care education
and foot examination were 60 (81.08%) and 55
(74.32 %) respectively. 42 (55.56%) walked barefoot
indoors; 43(56.97%) wear shoes without socks,
35(47.95%) did test the water temperature with
hand / elbow before taking a bath or a shower;
50 (68.49%) self-treated corns or calluses with
a blade; 67 (90.54%) wear sandals; almost all
73 (98.93) relied on feeling the fit of the
shoes when buying a new pair. Overall shoes
assessment was improper shoes in 64 (86.49%);
there were callus formation in 30 (42.26%),
foot deformity in 11 (15.28%), loss of sensation
by monofilament in 0 to 9 sites out of 10 in
foot 30 (40.54%), absence of dorsalis pedes
pulse in 10 (13.89%) and 40 % were classified
at risk category 1 to develop foot ulcer.
Prevalence of patients who achieved controlled
DM (<7) in this study was 42%. This result
is consistent with a big survey conducted in
9952 subjects which demonstrated that almost
half of the subjects did not meet the recommended
target of glycemic control, and especially the
rate of achieving the HbA1c target markedly
decreased with longer durations despite increases
in the use of any diabetes medication.(21)
In this study although patients who received
foot care education and foot examination were
60 (81.08%) and 55 (74.32 %) respectively, surprisingly,
foot care practices are still poor as shown
in improper footwear 64 (86.49%). Education
and foot examination were not usually associated
with improvement of foot care behaviors. A similar
result was found in a study conducted in the
USA and recommended that understanding the risk
factors, and having the ability to manage complications
outside of the clinical encounter is an important
part of a diabetes foot self-care management
program(22).
In this study, there were 21.13% of patients
who complained of feet pain and numbness which
is not consistent with another study conducted
in 160 patients with diabetes in a hospital
setting which demonstrated 42% had numbness/tingling
and pain in their feet (23). This difference
may be attributed to a population sample in
hospital settings. In another community based
study painful symptoms occurred in 26% of patients
without neuropathy(24) which is similar to the
current study.
In this study, we found that although approximately
80% of patients at Al Bateen Clinic engaged
in some recommended foot care practices and
education, fairly high proportions reported
foot care or footwear practices that should
be avoided; in particular, walking barefooted,
wearing shoes without socks and wearing pointed
(narrow) toe shoes that leads to development
of predisposing conditions of diabetic foot
like corn, calluses, foot injury, foot deformity,
fungal infections, clawing, ingrowing nails,
edema feet. Comparable data on footwear and
foot care practices in Caribbean populations,
from two studies, one from Trinidad25 and the
other from Barbados26 have reported some data.
In Trinidad 49% of patients attending primary
care diabetes clinics reported walking barefooted
inside the house and 23% walked barefooted outside
the house. Comparable data with similar results
in a study reported 44.4 % walking barefooted
inside home (27, 28).
In this study, we found 33.79% of the study
population were classified to have either risk
categories 1, 2 or 3 to develop foot ulcer.
Our data was similar to data demonstrated in
a study conducted in UAE in 2007 which showed
39% (95% CI: 35.1-43.7%) had peripheral neuropathy
and 12% (95% CI: 8.8-14.4%) had peripheral vascular
disease(29).
The findings of this study are limited by
the small sample size which limited our ability
to demonstrate any associations between foot
care practices or footwear and socio-demographic
factors. Despite these limitations, these data
highlight the need for further studies with
larger, representative samples to better understand
the problem at a national level. We also believe
that publication of these findings will serve
as a catalyst for further studies in the subject
area, where clinicians and researchers can evaluate
the extent to which appropriate practices are
being followed in their setting. Additionally,
prospective studies that evaluate the impact
of foot care and footwear practices on outcomes
such as foot ulcers and amputations would further
help to determine the potential for interventions
to improve practice and reduce complications.
Foot care practices are still substandard;
there was a gap between what patients receive
in foot education by health care provider and
what patients did in real practice., Potential
harmful foot care behaviors were high and protective
foot care practice was low. Finally there were
one or more risk factors of diabetic foot ulcer
in the majority of diabetic patients.
Overall, the study highlights the need for
greater emphasis on foot care education and
foot wear practices for patients with diabetes
in Al Bateen Clinic and the need to identify
barriers to foot care practice, both as it relates
to the physician and to the patient. This would
then lead to studies evaluating the efficacy
of various intervention strategies to provide
evidence-based guidelines for practice.
Acknowledgements
The first draft of study protocol was written
by the first author then authors from 1-5 reviewed
and edited the final study protocol; all authors
contributed in data collection. The first author
conducted the statistical analysis, results
and wrote the manuscript ( including the discussion
section) then all authors reviewed and edited
the manuscript and made the decision to submit
the manuscript for publication. The study was
approved by the ethics and research committee
in Ambulatory Healthcare Services/SEHA.
1.
International
Diabetes
Federation.
IDF
Diabetes,
7
ed.
Brussels,
Belgium:
International
Diabetes
Federation,
2015.
http://www.diabetesatlas.org
2.
P
J
Dyck,
J
L
Davies,
D
M
Wilson,
F
J
Service,
L
J
Melton,
3rd
and
P
C
O'Brien.
Risk
factors
for
severity
of
diabetic
polyneuropathy:
intensive
longitudinal
assessment
of
the
Rochester
Diabetic
Neuropathy
Study
cohort.
Diabetes
Care
September
1999
vol.
22
no.
9
1479-1486
3.
Nalini
Singh,
David
G.
Armstrong,
Benjamin
A.
Lipsky.
Preventing
Foot
Ulcers
in
Patients
with
Diabetes.
JAMA,
January
12,
2005-Vol
293,
No.
2
217-221
4.
American
Diabetes
Association.
Preventive
Foot
care
in
Diabetes.
Diabetes
Care
2004;
27
(suppl1):S63-S64
5.
Lawrence
A.
Lavery,
David
G.
Armstrong,
Robert
P.
Wunderlich,
M.
Jane
Mohler,
Christopher
S.
Wendel,
Benjamin
A.
Lipsky.
Risk
Factors
for
Foot
Infections
in
Individuals
with
Diabetes.
Diabetes
Care,
Volume
29,
Number
6,
June
2006
6.
David
G.
Armstrong,
and
Lawrence
A.
Lavery.
Diabetic
Foot
Ulcers:
Prevention,
Diagnosis
and
Classification.
Am
Fam
Physician.
1998
Mar
15;
57(6):1325-1332.
7.
Andrew
JM
Boulton
,
Loretta
Vileikyte
,
Gunnel
Ragnarson-Tennvall,
Jan
Apelqvist.
The
global
burden
of
diabetic
foot
disease
The
Lancet,
Volume
366,
Issue
9498,
Pages
1719
-
1724,
12
November
2005
8.
Marjolein
M.
Iversen,
Grethe
S.
Tell,
Trond
Riise,
Phd
Berit
R.
Hanestad.Truls
Østbye,
Marit
Graue,
Kristian
Midthjell.
History
of
Foot
Ulcer
Increases
Mortality
Among
Individuals
With
Diabetes.
Ten-year
follow-up
of
the
Nord-Trøndelag
Health
Study,
Norway.
Diabetes
Care,
Volume
32,
Number
12,
December
2009
2193
9.
Bharara
M,
Mills
JL,
Suresh
K.,
Rilo
HL.
Armstrong
DG,
Diabetes
and
landmine-related
amputations:
a
call
to
arms
to
save
limbs.
Int
Wound
J,
Feb.:6(1):2-3,
2009
10.
Brownrigg
JR,
Davey
J,
Holt
PJ,
Davis
WA,
Thompson
MM,
Ray
KK,
Hinchliffe
RJ.
The
association
of
ulceration
of
the
foot
with
cardiovascular
and
all-cause
mortality
in
patients
with
diabetes:
a
meta-analysis.
Diabetologia.
2012
Nov;55(11):2906-12.
doi:
10.1007/s00125-012-2673-3.
Epub
2012
Aug
14.
11.
Cara
Westphal,
Ingrid
M.
Neame,
Jessica
C.
Harrison,
Virginia
M.
Bower,
and
Joel
M.
Gurr,
A.
Diabetic
Foot
Ulcer
Pilot
Study,
Journal
of
the
American
Podiatric
Medical
Association
March
2011,
Vol.
101,
No.
2,
pp.
116-123
(doi:
10.7547/1010116)
12.
International
Consensus
on
the
Diabetic
Foot
and
Practical
Guidelines
on
the
Management
and
the
Prevention
of
the
Diabetic
Foot.
International
Working
Group
on
the
Diabetic
Foot,
2003,
Amsterdam,
the
Netherlands,
on
CD-ROM
(www.idf.org/bookshop).
13.
Jeffcoate
WJ,
van
Houtum
WH.
Amputation
as
a
marker
of
the
quality
of
foot
care
in
diabetes.Diabetologia.2004;
47:2051-2058
http://diabeticfootonline.blogspot.com/p/diabetic-foot-facts-and-figures.html
14.
Nadia
Saeed,
Frequency
of
patients
with
diabetes
taking
proper
foot
care
according
to
international
guidelines
and
its
impact
on
their
foot
health,
J
Pak
Med
Assoc,
Vol.
60,
No.
9,
September
2010
p
732-735
15.
Vileikyte
L,
Gonzalez
J,
Leventhal
H,
Peyrot
M,
Rubin
R,
Garrow
A,
Ulbrecht
J,
Cavanagh
P,
Boulton
A:
Patient
interpretation
of
neuropathy
(PIN)
questionnaire:
an
instrument
for
assessment
of
cognitive
and
emotional
factors
associated
with
foot
selfcare.
Diabetes
Care
2006,
29:2617-2624.
16.
Preventative
foot
care
in
diabetes.
Diabetes
Care
2004,
27:S63-S64.
17.
IWGDF:
International
consensus
on
the
diabetic
foot
Amsterdam:
International
Diabetes
Federation;
1999.
18.
http://cawc.net/images/uploads/wcc/7-2-orsted.pdf
19.
Andrew
J.M.
Boulton,
David
G.
Armstrong,
Stephen
F.
Albert,
Robert
G.
Frykberg,
Richard
Hellman,
M.
Sue
Kirkman,
Lawrence
A.
Lavery,
Joseph
W.
Lemaster,
Joseph
L.
Mills,
Michael
J.
Mueller,
Peter
Sheehan,
Dane
K.
Wukich.
Comprehensive
Foot
Examination
and
Risk
Assessment.
A
report
of
the
Task
Force
of
the
Foot
Care
Interest
Group
of
the
American
Diabetes
Association,
with
endorsement
by
the
American
Association
of
Clinical
Endocrinologists
Diabetes
Care,
Volume
31,
Number
8,
August
2008
20.
J.
Apelqvist,
K.
Bakker,
W.
H.
van
Houtum,
N.
C.
Schaper.
Practical
guidelines
on
the
management
and
prevention
of
the
diabetic
foot
based
upon
the
International
Consensus
on
the
Diabetic
Foot
(2007)
.Prepared
by
the
International
Working
Group
on
the
Diabetic
Foot
Diabetes/Metabolism
Research
And
Reviews
Guidelines.
Diabetes
Metab
Res
Rev
2008;
24(Suppl
1):
S181-S187.
21.
Yokoyama,
H.,
Oishi,
M.,
Takamura,
H.,
Yamasaki,
K.,
Shirabe,
S.,
Uchida,
D.,
Sugimoto,
H.,
Kurihara,
Y.,
Araki,
S.
and
Maegawa,
H.
Large-scale
survey
of
rates
of
achieving
targets
for
blood
glucose,
blood
pressure,
and
lipids
and
prevalence
of
complications
in
type
2
diabetes
(JDDM
40).
BMJ
Open
Diabetes
Research
&
Care,
4(1),
(2016).
p.
e
000294.
22.
Bonner,
Timethia;
Foster,
Margaret;
Spears-Lanoix,
Erica.
Type
2
diabetes-related
foot
care
knowledge
and
foot
self-care
practice
interventions
in
the
United
States:
a
systematic
review
of
the
literature.
Diabetic
Foot
&
Ankle,
[S.l.],
v.
7,
feb.
2016.
Available
at:
<http://diabeticfootandankle.net/index.php/dfa/article/view/29758>.
Date
accessed:
18
Nov.
2016.
doi:http://dx.doi.org/10.3402/dfa.v7.29758.
23.
Caroline
A.
Abbott,
Rayaz
A.
Malik,
Ernest
R.E.
van
Ross,
Jai
Kulkarni,
Andrew
J.M.
Boulton
Prevalence
and
Characteristics
of
Painful
Diabetic
Neuropathy
in
a
Large
Community-Based
Diabetic
Population
in
the
U.K
25-Diabetes
Care.
2011
Oct;
34(10):
2220-2224.
Published
online
2011
Sep
15.
doi:
10.2337/dc11-1108
24.-D'Souza,
M.,
Ruppert,
S.,
Parahoo,
K.,
Karkada,
S.,
Amirtharaj,
A.,
Jacob,
D.,
Balachandran,
S.
and
Al
Salmi,
N.
(2016).
Foot
care
behaviors
among
adults
with
type
2
diabetes.
Primary
Care
Diabetes,
10(6),
pp.442-451.
25.
Gulliford
MC,
Mahabir
D.
Diabetic
foot
disease
and
foot
care
in
a
Caribbean
community.
Diabetes
Res
Clin
Pract
2002;
56:35-
40.
26.
Hennis
AJ,
Fraser
HS,
Jonnalagadda
R,
et
al.
Explanations
for
the
high
risk
of
diabetes-
related
amputation
in
a
Caribbean
population
of
black
African
descent
and
potential
for
prevention.
Diabetes
Care
2004;
27:2636-41.
27.
Gayle
KAT,
Tulloch
Reid
MK,
Younger
NO,
et
al.
Foot
care
and
footwear
practices
among
patients
attending
a
specialist
diabetes
clinic
in
Jamaica.
Clinics
and
Practice.
2012;
2(4):e85.
doi:10.4081/cp.2012.e85.
28.
Maniram
Kumhar,
Narendar
Dara,
Tarachand
Saini.
Foot
Wear
and
Footcare
Knowledge.
An
Independent
Risk
Factor
for
Diabetic
Foot
in
Indian
Diabetics.
Indian
Medical
Gazette,
January
2014.
p25-26
29.
Chiwanga
FS,
Njelekela
MA.
Diabetic
foot:
prevalence,
knowledge,
and
foot
self-care
practices
among
diabetic
patients
in
Dar
es
Salaam,
Tanzania
-
a
cross-sectional
study.
Journal
of
Foot
and
Ankle
Research.
2015;8:20.
doi:10.1186/s13047-015-0080-y.
30.
Fatma
Al-Maskari
and
Mohammed
El-Sadig
Prevalence
of
risk
factors
for
diabetic
foot
complications.BMC
Family
Practice20078:
59.DOI:
10.1186/1471-2296-8-59
|

