|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................ |
Original
Contribution / Clinical Investigation
|





|
<-- Kuwait -->
Hyperglycemia
In Pregnancy in Arab Population, Kuwait Oil
Company Hospital, Kuwait
[pdf
version]
Hany M. Aiash, Sameh F. Ahmed,
Amro Abo Elezz
<-- Jordan -->
Ischiofemoral
impingement syndrome , incidence and clinical
importance
[pdf
version]
Jamil S. Shawaqfeh, Maysoon Banihani, Hend Harahsheh,
Ashraf Tamimi,
Abdulaziz Bawazir
<-- Abu Dhabi -->
Assessment
of behaviors, risk factors of Diabetic foot
ulcer and footwear safety among diabetic patients
in primary care setting, Abu Dhabi, UAE
[pdf version]
Osama Moheb Ibrahim Mohamed, Nwanneka E. O.
Ofiaeli, Adnan Syeed, Amira Elhassan,
Mona Al Tunaiji, Khuloud Al Hammadi, Maryam
Al Ali
<-- Nepal -->
Determinants
and Prevalence of Stunting Among Rural Kavreli
Pre-school Children
[pdf
version]
Kharel Sushil, Mainalee Mandira, Pandey Niraj
DOI:
<-- Qatar -->
Medical
and Psychological Associations with Nocturnal
Enuresis in Children in Qatar
[pdf version]
Ahmed Mohamed Kahlout, Hayam Ali AlSada
|
........................................................
International Health
Affairs
|

|
<-- Turkey -->
Aging
Syndrome
[pdf
version]
Mehmet Rami Helvaci, Orhan Ayyildiz, Orhan Ekrem
Muftuoglu, Mustafa Yaprak
Abdulrazak Abyad, Lesley Pocock
|
........................................................
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| April/May 2017
- Volume 15, Issue 3 |
|
|
Medical and Psychological
Associations with Nocturnal Enuresis in Children
in Qatar
Ahmed Mohamed
Kahlout
Hayam Ali AlSada
PHCC, Doha
Qatar
Correspondence:
Dr. Ahmed
Mohamed Kahlout
Doha
Qatar
Email: akahlout@phcc.gov.qa
|
Abstract
Nocturnal Enuresis is a common problem
observed in Qatar. However, no Qatar-based
study has examined enuresis in the primary
health care setting, and thus this study
will have particular relevance to this
population. A prospective study was designed
in primary health care centers in Qatar
to collect information on Nocturnal Enuresis
of children in Qatar.
Aim: The aim of this study is to
determine the prevalence of Enuresis and
its recovery rate among children in the
Western Area of Doha, and evaluate the
different associations between Nocturnal
Enuresis (NE) and medical and psychological
conditions, and to assess the impact of
the condition in children and families.
Methods: Questionnaires about nocturnal
enuresis were distributed to the parents
of 399 children age 5 to 11 frequenting
the Primary Health Care centers clinics
in the Western Area of Doha. All cases
received followed up evaluations at 6,
12, and 18 months.
Results: The results indicated
a 36.3% prevalence of Enuresis in children.
Significant associations of medical and
psychological problems such as snoring,
bronchial asthma and stressful events
were found. Recovery rates of 26, 24,
and 19% were observed after 3 times follow-up
at 6, 12, and 18 months respectively.
Conclusions: This study confirms
the prevalence of Nocturnal Enuresis among
children frequenting the primary health
care centers of the Western area of Doha,
and the Medical and Psychological associations
are similar to those of similar studies
from various countries of the Arab countries
area. Health education will encourage
the parents to be aware, deal with this
problem and find appropriate medical advice.
Key words: nocturnal
enuresis, Medical and psychological associations,
Doha, Qatar
|
Enuresis is a condition characterized by involuntary
discharge of urine overnight, as per the ICCS
definition (1). Commonly seen in young children,
enuresis is considered problematic when it occurs
in children 5 or older. Enuresis may be primary
or secondary, where a child with primary enuresis
has never had a dry period for at least 6 months,
whereas a child with secondary enuresis has
experienced a dry spell of at least this duration
(1, 2, 3).
Various management strategies are available
for nocturnal enuresis: for example, counseling
of parents, medical treatment, or psychotherapy.
Nocturnal Enuresis is a common problem observed
in Qatar. However, no Qatar-based study has
examined enuresis in the primary health care
setting, and thus this study will have particular
relevance to this population.
The aim of this study is to determine the prevalence
of Enuresis and its recovery rate among children
in the Western Area of Doha, and evaluate the
different associations between Nocturnal Enuresis
(NE) and medical and psychological conditions,
and to assess the impact of the condition in
children and families.
Participants
were
children
age
5
to
11
recruited
while
visiting
the
Primary
Health
Care
clinics;
children
with
known
neurological
and
genetic
syndromes
were
excluded.
The
study
was
conducted
by
requesting
that
parents
complete
a
questionnaire
on
their
child's
history
with
urinary
and
other
behaviors.
The
questionnaire
was
purpose-built
for
this
research
by
the
author
and
was
subsequently
validated
by
the
Hamad
Medical
Corporation
(HMC)
Research
Committee.
This
study
was
approved
by
HMC
ethics
committee.
The
questionnaire
consisted
of
three
parts
where
the
first
part
included
socio-demographic
characteristics
and
toilet
training
of
the
sample.
The
second
part
was
designed
to
enquire
about
the
presence
of
nocturnal
enuresis
and
its
relevant
characteristics.
Children
without
NE
were
asked
about
the
age
of
dryness.
The
third
part
of
the
questionnaire
asked
all
participants
about
psychological
and
medical
conditions
such
as
constipation,
snoring,
and
the
experience
of
stressful
events.
Sleep
disturbances
are
defined
by
the
ICD-10
such
as
nightmares,
sleep
terrors,
sleep
walking,
and
sleep
talking.
Constipation
was
defined
as
delay
or
difficulty
in
defecation,
present
for
two
or
more
weeks
and
sufficient
to
cause
distress
to
the
patient.
(4,5)
The
questionnaire
was
not
based
on
the
Screening
Instrument
for
Psychological
Problems
because
ADD
and
ADHD
subjects
were
not
part
of
the
study.
The
questionnaires
were
not
validated
as
the
Vancouver
or
Toronto
voiding
questionnaires.
Statistical
Analysis:
Qualitative
and
quantitative
data
values
were
expressed
as
frequency
along
with
percentage
and
mean±SD.
Descriptive
statistics
were
used
to
summarize
demographic
and
all
other
clinical
characteristics
of
the
participants.
The
prevalence
of
nocturnal
enuresis
was
estimated
and
presented
along
with
95%
CI.
Associations
between
two
or
more
qualitative
variables
were
assessed
using
chi-square
test,
chi-square
test
with
continuity
correction
factor
or
Fisher
exact
test
as
appropriate.
Quantitative
variables
data
between
two
independent
groups
(nocturnal
enuresis
and
nocturnal
continence)
were
analyzed
using
unpaired
't'
test.
The
results
were
presented
with
the
associated
95%
confidence
interval.
Univariate
and
multivariate
logistic
regression
analysis
was
carried
out
to
assess
the
association
of
various
potential
factors
and
predictors
such
as
age
at
diurnal
dryness,
age
at
nocturnal
dryness,
age
when
child
started
toilet
training,
gender,
family
size,
family
history
enuresis,
nocturnal
dryness,
suffer
constipation,
fecal
incontinence,
stressful
events,
snoring
and
other
medical
problems
with
outcome
variable
nocturnal
enuresis.
Logistic
regression
analysis
results
were
presented
in
terms
of
odds
ratio
(OR)
and
associated
95%
CI.
A
two-sided
P
value
<0.05
was
considered
to
be
statistically
significant.
All
Statistical
analyses
were
done
using
statistical
packages
SPSS
22.0
(SPSS
Inc.
Chicago,
IL).
There
were
399
participants
in
the
study;
145
(36.3%)
were
nocturnal
enuresis,
254
(73.7%)
participants
were
nocturnal
continence.
Mean
age
at
diurnal
dryness
in
the
nocturnal
enuresis
group
was
significantly
higher
30.7±7.8
years,
compared
to
nocturnal
continence
group
27.9±7.4
years
(P<0.001).
Similarly,
the
mean
age
at
nocturnal
dryness
(40.6±14.8
vs
34.4±10.1;
P=0.004),
age
when
child
started
toilet
training
(25.8±6.9
vs
23.8±6.9;
P=0.006)
in
the
nocturnal
enuresis
group
was
significantly
higher
compared
to
nocturnal
continence
group
respectively.
Surprisingly,
we
found
that
36.3%
of
children
suffered
from
enuresis,
while
the
remaining
subjects
didn't
suffer
from
enuresis.
This
was
based
on
analyzing
data
collected
from
399
patients
at
Al
Rayyan
and
Abu
Baker
primary
health
care
centers,
of
which
84
(59%)
were
male
(Table
2).
Of
all
participants,
the
age
when
the
child
started
toilet
training
was
24.6
months
on
average;
diurnal
dryness
was
achieved
at
age
28.9
months
(±7.6),
and
nocturnal
dryness
was
achieved
at
35.5
months
(±11.4)
(Table
1).
The
prevalence
of
nocturnal
enuresis
and
their
association
with
demographic,
physiological,
and
other
medical
and
clinical
characteristics
are
shown
in
Table
2.
The
overall
prevalence
of
nocturnal
enuresis
was
36.3%
(95%
CI:
31.6
to
41.1).
The
prevalence
of
nocturnal
enuresis
in
the
positive
family
history
of
enuresis
was
significantly
higher
97/172;
56.4%
compared
with
48/227;
21.1%
(P<0.001)
in
the
nocturnal
continence
group.
Significantly
higher
nocturnal
enuresis
prevalence
occurred
among
children
who
presented
with
non-nocturnal
dryness
(87.6%
vs
16.1%;
P<0.001)
compared
to
nocturnal
dryness.
Similarly
children
experiencing
stressful
events
had
significantly
higher
nocturnal
enuresis
compared
with
children
with
stressful
events
(56.3%
vs
17.9%;
P<0.00).
Also,
children
with
other
medical
problems
showed
a
similar
trend
with
significantly
higher
occurrences
of
nocturnal
enuresis,
P<0.001.
Gender,
age
at
diurnal
dryness,
family
history,
did
not
have
any
significant
association
with
nocturnal
enuresis
as
presented
in
Table
2.
The
results
of
logistic
regression
analysis
testing
for
each
predictive
variable
and
factors
and
their
association
with
nocturnal
enuresis
are
presented
in
Table
2.
The
results
were
presented
with
odds
ratio
(OR)
and
associated
95%
confidence
interval
(CIs).
Logistic
regression
analysis
revealed
that
increasing
age
at
nocturnal
dryness,
age
when
child
started
toilet
training,
family
history
enuresis,
nocturnal
dryness,
suffer
constipation,
fecal
incontinence,
stressful
events,
snoring
and
other
medical
problems
were
common
risk
factors
and
predictors
significantly
associated
with
an
increased
risk
for
nocturnal
enuresis.
Risk
of
nocturnal
enuresis
was
2.6
times
likely
to
be
higher
among
children
having
age
at
nocturnal
dryness
more
than
40
months
(unadjusted
OR
2.6,
95%
CI
1.37-4.94;
P=0.003)
compared
to
age
group
less
or
equal
to
forty
months.
Children
who
had
positive
family
history
of
enuresis
were
nearly
4.8
times
as
likely
to
have
more
risk
for
nocturnal
enuresis
(unadjusted
OR
4.82,
95%
CI
3.11-7.48;
P<0.001).
Children
who
had
nocturnal
enuresis
were
nearly
1.7
times
as
likely
to
suffer
from
constipation
(unadjusted
OR
1.68,
95%
CI
1.0-2.82;
P=0.05),
3.1
times
as
likely
to
be
positive
for
fecal
incontinence
(unadjusted
OR
3.06,
95%
CI
1.09-8.61;
P=0.034),
5.9
times
as
likely
to
have
stressful
events
(unadjusted
OR
5.91,
95%
CI
3.75-9.32;
P<0.001),
4.2
times
as
likely
to
have
sleep
disturbance
and
3.4
times
more
likely
to
have
other
medical
problems,
than
those
who
had
nocturnal
continence.
Children
with
enuresis
were
twice
as
likely
to
snore
than
children
without
enuresis
(unadjusted
OR
2.1,
95%
CI
1.29-3.78;
P=0.003).
Children
with
enuresis
were
almost
8
times
more
likely
to
have
worms
than
children
without
enuresis
(unadjusted
OR
7.9,
95%
CI
4.19-15.14;
P<0.001).
Using
multivariable
logistic
regression
analysis
controlling
for
all
other
potential
predictors
and
factors
such
as
age
at
diurnal
dryness,
age
at
nocturnal
dryness,
age
when
child
started
toilet
training,
gender,
family
size,
family
history
enuresis,
suffer
constipation,
fecal
incontinence,
stressful
events,
snoring
and
other
medical
problems
we
found
that
the
factors
with
the
strongest
and
significant
association
with
nocturnal
enuresis
are
children
having
positive
family
history
of
enuresis,
nocturnal
dryness,
stressful
events
and
sleeping
disturbance
or
snoring.
No
significant
interactions
were
found
between
different
potential
factors
and
predictors
considered
above
and
including
an
interaction
terms
in
the
model,
had
no
effect
on
the
adjusted
odds
ratio
as
shown
in
Table
3.
Most
parents
were
assisting
their
children
when
they
bed
wet
(64);
43
blamed
the
child
and
6
spanked
the
child
(Table
1).
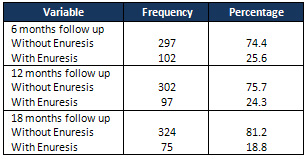
At
the
follow
up
evaluations
at
6,
12,
and
18
months
where
the
number
of
children
with
enuresis
reduced
from
102
children
to
97
and
75
respectively
(Table
4).
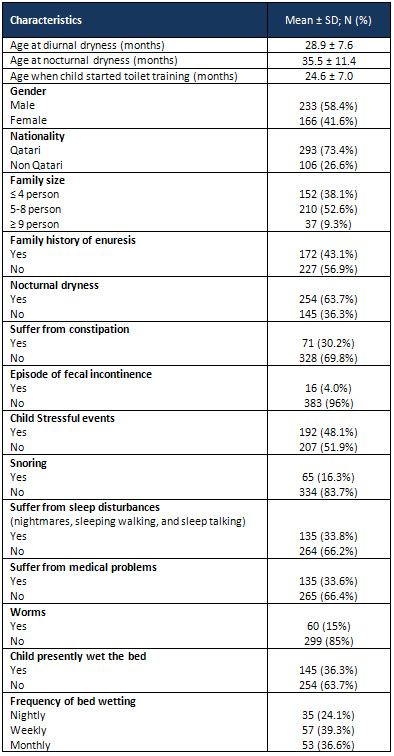
Table
1:
Baseline
Demographic,
Physiological
and
other
Clinical
Characteristics
Table
2:
Association
of
various
predictors
with
nocturnal
enuresis:
Univariate
Logistic
regression
analysis
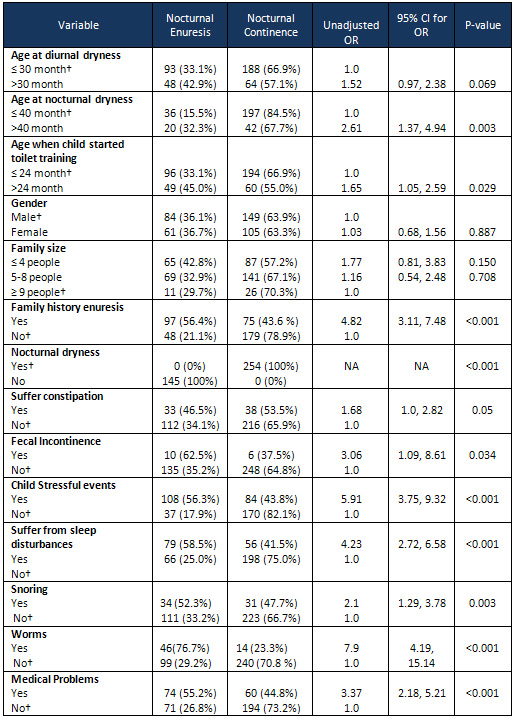 CI:
Confidence
interval;
OR:
odds
ratio;
†Subjects
in
this
category
served
as
the
reference
group.
CI:
Confidence
interval;
OR:
odds
ratio;
†Subjects
in
this
category
served
as
the
reference
group.
The
sum
may
not
equal
to
n=399
for
some
variables
due
to
some
missing
data.
Table
3.
Association
of
various
predictors
with
nocturnal
enuresis:
Multivariate
Logistic
regression
analysis
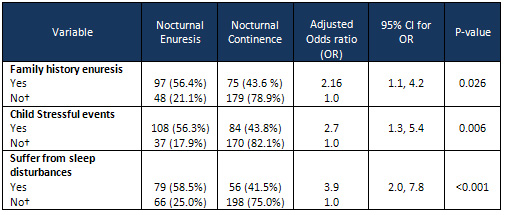
CI:
Confidence
interval;
†Subjects
in
this
category
served
as
the
reference
group.
The
sum
may
not
equal
to
n=399
for
some
variables
due
to
some
missing
data.
Table
4:
Follow-up
outcome
measures
| DISCUSSION
AND
CONCLUSIONS
|
In
our
study,
we
found
a
high
prevalence
and
an
unexpectedly
high
percentage
of
nocturnal
enuresis
(36.3%)
with
equal
distribution
in
both
sexes.
In
similar
studies
carried
out
in
Jordan
and
Yemen,
the
prevalence
of
Nocturnal
Enuresis
among
5
to
15
years
old
children
was
reported
as
8.8%
to
28.6%
respectively
(6,
7).
The
prevalence
found
in
this
study
was
higher
than
reported
worldwide,
at
8.3
-
12.3%
(9).
This
difference
could
be
explained
due
to
the
high
number
of
5
and
6-year
old
participants
in
our
study
which
also
explains
the
reduction
in
the
numbers
found
also
at
the
follow
up
evaluations
at
6,
12,
and
18
months
where
the
number
of
children
with
enuresis
reduced
from
102
(25%)
children
to
97
(24%)
and
75
(19%)
respectively.
At
this
age,
the
rate
of
resolution
worldwide
is
usually
reported
at
15%
per
year
(9).
Stressful
events
and
sleep
disturbances
were
significantly
higher
in
the
children
with
enuresis
compared
with
those
without
enuresis
-
74.5%
vs.
33.1%
,
p
<
.0001,
and
54.5
%
vs22
%
p
<0001
respectively.
Worldwide
the
overall
rate
of
comorbidity
in
epidemiological
and
in
clinical
studies
are
approximately:
13.5%-40.1%
of
all
wetting
children
have
clinically
relevant
behavioral
problems
(9),
emphasizing
the
importance
of
taking
a
thorough
history
of
sleep
disturbances
such
as
nightmares,
sleepwalking,
sleep
talking,
and
stressful
events
like
mother
deprivation,
school
failure,
and
siblings'
rivalry.
It
is
helpful
to
support
the
family
and
children
in
these
cases
with
follow
up
even
without
excellent
outcome
of
the
treatment,;
(10)
when
necessary,
patients
should
be
referred
to
the
appropriate
professionals
for
related
conditions.
Medical
problems
(e.g.,
UTI,
bronchial
asthma)
were
found
to
be
higher
in
the
children
with
enuresis
compared
to
the
control
group
(unadjusted
OR
3.37,
95%
CI
2.18-5.21;
P<0.001)
while
intestinal
worms
in
children
in
enuresis
were
also
found
to
be
higher
(unadjusted
OR
7.9,
95%
CI
4.19-15.14;
P<0.001)
These
children
may
benefit
from
medical
treatment.
Of
course,
treatment
of
intestinal
worms
will
reduce
one
of
the
child's
sufferings
but
it
is
not
known
whether
this
contributes
to
the
resolution
of
enuresis
or
not.
It
was
found
that
34
children
with
enuresis
also
were
snoring
(unadjusted
OR
2.1,
95%
CI
1.29-3.78;
P=0.003).
On
the
other
hand
31
children
without
enuresis
were
also
snoring.
We
don't
know
whether
future
treatment
of
snoring
will
improve
bedwetting
as
was
found
in
another
study
where
half
of
the
children
tonsillectomised
had
improvement
of
their
enuresis
(8).
During
the
3
follow
ups
(6,
12,
and
18
months),
spontaneous
recovery
was
observed.
Recovery
rates
of
26,
24,
and
19%
were
observed
after
3
times
follow-up
at
6,
12,
and
18
months
respectively.
Interestingly,
there
were
several
new
cases
of
children
without
enuresis
starting
to
bed
wet
(likely
from
secondary
enuresis),
which
should
prompt
a
clinician
to
investigate
and
treat
possible
causes.
We
recommend
that
clinicians
obtain
a
thorough
family,
genetic,
trauma,
stressful
events,
and
toilet-training
history;
conduct
a
physical
examination;
and
perform
urine
and
stool
analysis
and
cultures,
urine
24-hour
osmolarity,
and
blood
sugar
tests.
Abdominal
and
pelvic
ultrasounds
would
be
useful
for
suspected
congenital
malformation.
Nocturnal
enuresis
is
a
benign
condition,
and
its
complications
can
often
be
resolved
with
special
care
and
treatment.
1.
The
Standardization
of
Terminology
of
Lower
Urinary
Tract
Function
in
Children
and
Adolescents:
Update
Report
from
the
Standardization
Committee
of
the
International
Children's
Continence
Society.
Austin,
Paul
F.
et
al.
The
Journal
of
Urology,
Volume
191,
Issue
6,
1863
-
1865.e13
2.
Jacobson:
Psychiatric
Secrets,
2nd
ed.;
Chapter
59
-
Encopresis
and
Enuresis
3.
DSM-IV
casebook:
A
learning
companion
to
the
Diagnostic
and
Statistical
Manual
of
Mental
Disorders-4th
ed.
Spitzer,
Robert
L.
(Ed);
Gibbon,
Miriam
(Ed);
Skodol,
Andrew
E.
(Ed);
Williams,
Janet
B.
W.
(Ed);
First,
Michael
B.
(Ed).
Arlington,
VA,
US:
American
Psychiatric
Association.
(1994)
4.
Susan
S.
Baker,
Gregory
S.
Liptak,
Richard
B.
Colletti,
Joseph
M.
Croffie,
Carlo
Di
Lorenzo,
Walton
Ector,
and
Samuel
Nurko.
Constipation
in
Infants
and
Children:
Evaluation
and
Treatment.
Journal
of
Pediatric
Gastroenterology
&
Nutrition,
Vol
30,
Issue
1,
p
109.
(2000)
5.
Camilleri
M.
Disorders
of
gastrointestinal
motility.
In:
Goldman
L,
Schafer
AI,
eds.
Camilleri
M.
Disorders
of
gastrointestinal
motility.
In:
Goldman
L,
Schafer
AI,
eds.
Goldman's
Cecil
Medicine.
24th
ed.
Philadelphia,
PA:
Elsevier
Saunders;
2011:chap
138.
6.
Lembo
AJ,
Ullman
SP.
Constipation.
In:
Feldman
M,
Friedman
LS,
Sleisenger
MH,
eds.
Sleisenger
&
Fordtran's
Gastrointestinal
and
Liver
Disease.
9th
ed.
Philadelphia,
PA:
Elsevier
Saunders;
2010:chap
18
7.
Al-Rashed
KH,
Bataineh
HA.
Frequency
of
enuresis
in
(5-10)
year
old
children
in
Taifila,
Jordan.
Shiraz
E-Med
J.
2007;
8(1):
1-9.
8.
Aljefri
HM,
Basurreh
OA,
Yunus
F,
et
al.
Nocturnal
enuresis
among
primary
school
children.
Saudi
J
Kidney
Dis
Transplant.
2013;
24(6):
1233-41.
9.
Larisa
Kovacevic,*
Cortney
Wolfe-Christensen,
Hong
Lu,
Monika
Toton,
Jelena
Mirkovic,
Prasad
J.
Thottam,
Ibrahim
Abdulhamid,
David
Madgy
and
Yegappan
Lakshmanan.
Why
does
Adenotonsillectomy
Not
Correct
Enuresis
in
All
Children
with
Sleep
Disordered
Breathing?
THE
JOURNAL
OF
UROLOGY,
MAY
2014
10.
The
Journal
of
Urology
Vol.
171,
2545-2561,
June
2004.
Nocturnal
Enuresis:
An
International
Evidence
Based
Management
Strategy.
K.
Hjalmas,*,†
Sweden;
T.
Arnold,
New
Zealand;
W.
Bower,
Australia/Hong
Kong;
P.
Caione,
Italy;
L.
M.
Chiozza,
Italy;
A.
Von
Gontard,
Germany;
S.
W.
Han,
S.
Korea;
D.
A.
Husman,
Usa;
A.
Kawauchi,
Japan;
G.
La¨
Ckgren,
Sweden;
H.
Lottmann,
France;
S.
Mark,
New
Zealand;
S.
Rittig,
Denmark;
L.
Robson,
Usa;
J.
Vande
Walle,
Belgium
And
C.
K.
Yeung,
Hong
Kong
On
Behalf
Of
The
International
Children's
Continence
Society
(Iccs)
11.
Longstaffe,
S.,
Moffat,
M.
and
Whalen,
J.:
Behavioral
and
self-concept
changes
after
six
months
of
enuresis
treatment:
a
randomized,
controlled
trial.
Pediatrics,
105:
935,
2000
|
|
.................................................................................................................

|
| |
|

