|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................ |
Original
Contribution / Clinical Investigation
|





|
<-- Kuwait -->
Hyperglycemia
In Pregnancy in Arab Population, Kuwait Oil
Company Hospital, Kuwait
[pdf
version]
Hany M. Aiash, Sameh F. Ahmed,
Amro Abo Elezz
<-- Jordan -->
Ischiofemoral
impingement syndrome , incidence and clinical
importance
[pdf
version]
Jamil S. Shawaqfeh, Maysoon Banihani, Hend Harahsheh,
Ashraf Tamimi,
Abdulaziz Bawazir
<-- Abu Dhabi -->
Assessment
of behaviors, risk factors of Diabetic foot
ulcer and footwear safety among diabetic patients
in primary care setting, Abu Dhabi, UAE
[pdf version]
Osama Moheb Ibrahim Mohamed, Nwanneka E. O.
Ofiaeli, Adnan Syeed, Amira Elhassan,
Mona Al Tunaiji, Khuloud Al Hammadi, Maryam
Al Ali
<-- Nepal -->
Determinants
and Prevalence of Stunting Among Rural Kavreli
Pre-school Children
[pdf
version]
Kharel Sushil, Mainalee Mandira, Pandey Niraj
DOI:
<-- Qatar -->
Medical
and Psychological Associations with Nocturnal
Enuresis in Children in Qatar
[pdf version]
Ahmed Mohamed Kahlout, Hayam Ali AlSada
|
........................................................
International Health
Affairs
|

|
<-- Turkey -->
Aging
Syndrome
[pdf
version]
Mehmet Rami Helvaci, Orhan Ayyildiz, Orhan Ekrem
Muftuoglu, Mustafa Yaprak
Abdulrazak Abyad, Lesley Pocock
|
........................................................
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| April/May 2017
- Volume 15, Issue 3 |
|
|
Hyperglycemia In Pregnancy
in Arab Population, Kuwait Oil Company Hospital,
Kuwait
Hany M. Aiash
(1)
Sameh F. Ahmed (2)
Amro Abo Elezz (3)
(1) Hani M. Aiash, MD, Family
Medicine Department, Faculty of Medicine,
Suez Canal University, Egypt
(2) Sameh F. Ahmed, MD, Family Medicine Department,
Faculty of Medicine,
Suez Canal University, Egypt
(3) Amro Abo Elezz, MD, Gynaecology & Obstetrics
Department, Faculty of Medicine,
Azhar University, Egypt
Correspondence:
Sameh
F. Ahmed, MD,
Family Medicine Department,
Faculty of Medicine,
Suez Canal University,
Ismailia, 41111
Egypt
Phone: 00201118718112;
00966581803197(KSA)
Email: samehfawzi3691@gmail.com
|
Abstract
Background: The hyperglycemic population
in pregnancy consists of two main cohorts-
subjects with onset or first recognition
during pregnancy (Gestational diabetes
mellitus -GDM) and subjects with preexisting
history of diabetes mellitus. The prevalence
of GDM has been steadily increasing with
the rise of obesity and unhealthy life
style reaching up to 14 % annually in
many countries including the United States.
Hyperglycemia from any cause can seriously
affect both mother and baby and increases
the risk of complications during pregnancy,
labor and after delivery.
Aim: We aimed to study any baseline
obstetric history differences as well
as labor outcomes and neonatal characteristics
between the two groups, Group A- impaired
glucose tolerance and recent diagnosis
of pregnancy induced diabetes mellitus
( n=240), and, Group B- known history
of Type 2 Diabetes mellitus and already
on medication (n=240).
Methods: This is a prospective,
open label, double arm, observational,
longitudinal registry study. The registry
was launched with immediate effect in
December 2012 and recruitment of subjects
continued until January 2014. After fulfilling
the inclusion criteria, a total of 480
subjects comprising two equal groups (Group
A with a known history of type 2 diabetes
mellitus and Group B with GDM) were recruited;
their obstetric history captured and they
were followed up on a regular basis till
delivery. Mode of delivery and neonatal
status especially APGAR status at birth,
5 minutes and 10 minutes were closely
monitored and captured using an eCRF by
the study physicians.
Results: Statistical analysis revealed
a significant difference in the obstetric
history-parity (p=0.000), previous abortion
history (p=0.007), previous caesarean
sections (p= 0.000) and type of delivery
(vaginal, caesarean, vacuum (p value=
0.000, 0.000 and 0.006 respectively) while
there were no statistically significant
variations amongst the neonatal statuses
except for higher birth weight (p=0.02)
and neonatal complications (p=0.033).
Conclusion: Hyperglycemia with
pregnancy is a steadily increasing problem
that can seriously affect both mother
and baby as shown in the present study
, however, the present study did not show
any significant differences in the weeks
of delivery (preterm vs term). Also, the
present study revealed more congenital
heart problems, especially septal defects,
among offspring of mothers with overt
type 2 DM due to the chronicity of hyperglycemia
compared with offspring of mothers with
gestational diabetes.
Key words: Gestational Diabetes
Mellitus, Impaired Glucose Tolerance,
Type 2 Diabetes Mellitus, APGAR
|
Kuwait has acquired a notorious place in the
world ranking of metabolic disorders in the
last decade, especially Diabetes Mellitus, mainly
owing to the extreme climate (which makes outdoor
activities less feasible) and unhealthy dietary
habits. The hyperglycemic population in pregnancy
consists of two main cohorts- subjects with
onset or first recognition during pregnancy
(Gestational diabetes mellitus -GDM) and subjects
with preexisting history of diabetes mellitus.(1)
Innumerous trials around the globe have dealt
with the concept of impaired glucose tolerance
and its effect on pregnancy and adverse outcomes.
The prevalence of GDM has been steadily increasing
with the rise of obesity and unhealthy life
style, reaching up to 14 % annually in the United
States, says Center for Disease Control (CDC).(2)
Pregnant women with gestational diabetes and
impaired glucose tolerance are at high risk
for pregnancy and delivery complications including
infant macrosomia, neonatal hypoglycemia and
caesarean delivery. (3,4) Hence, the impending
necessity for a registry which compares the
two hyperglycemic manifestations as GDM and
known T2DM, so as to determine the effect of
chronicity of hyperglycemia in pregnancy and
neonatal statuses piqued our efforts. An intensive
lifestyle intervention could significantly reduce
incidence of diabetes. Weight loss and 150 min
of physical activity per week similar in intensity
to brisk walking are the most effective lifestyle
intervention.(5)
This
prospective,
open
label,
double
arm,
observational,
longitudinal
registry
sought
the
approval
of
its
sole
site
(KOC
hospital,
Kuwait)
ethics
committee
and
gained
the
approval
by
November
2012.
The
registry
was
launched
with
immediate
effect
in
December
2012
and
recruitment
of
subjects
(who
complied
with
proper
informed
consent
procedure)
continued
until
January
2014.
The
inclusion
criteria
were
broad,
comprising
3
main
points:
(a)
Willingness
to
perform
GTT
(Glucose
tolerance
test)
during
24-28
gestational
weeks
and
follow
study
procedure,
(b)
Women
with
risk
factors
for
hyperglycemia
and
(c)
Signed
informed
consent.
Exclusion
criteria
included
any
subject
<
18
years
of
age,
any
underlying
history
of
co-morbidities
such
as
hypertension,
coronary
artery
disease,
chronic
kidney
disease
and/
or
inability
to
provide
informed
consent.
All
subjects
in
the
first
trimester
presenting
to
KOC
hospital
Obstetrics
department
were
screened
for
a
known
history
of
T2DM
and/or
minimal
two
consecutive
incidences
of
elevated
Blood
Glucose
levels
sufficient
to
meet
the
WHO
-
GDM
definition.(6,7)
All
subjects
with
confirmed
fasting
glucose
levels
of
>
7.0
mmol/L
or
random
glucose
levels
of
>
11.1
mmol/L
in
the
first
trimester
were
classified
as
overt
/
T2DM
and
grouped
together
(
Group
B)
while
those
who
presented
with
impaired
glucose
tolerance
confirmed
by
a
positive
Oral
Glucose
Tolerance
Test
(OGTT)
between
24-
28
gestational
weeks
were
classified
as
GDM
(
Group
A).(3)
Both
groups
had
their
OGTT
performed
and
analyzed
at
KOC
hospital
laboratory.
The
OGTT
consisted
of
75
g
2-hours
glucose
test
and
was
carried
out
after
overnight
fasting
(10-16
hours)
and
at
least
3
days
of
unrestricted
diet
and
normal
physical
activity.
A
total
of
480
subjects
(Group
A,
n=240
and
Group
B,
n=240)
were
recruited,
their
obstetric
history
captured
and
followed
up
on
a
regular
basis
till
delivery.
Mode
of
delivery
and
neonatal
status
especially
APGAR
status
at
birth,
5
minutes
and
10
minutes,
were
closely
monitored
and
captured
using
an
eCRF
by
the
study
physicians.
Statistical
analysis:
Data
were
analyzed
using
SPSS
version
12.0.
A
confidence
interval
of
5%
and
p-
value
of
0.05
were
set.
MANOVA
and
ANOVA
were
performed.
To
find
significant
correlations,
Chi-square
tests
were
adopted
for
continuous
variables
while
Mann
Whitney's
U
test
was
used
for
categorical
variables.
Click
here
for
Table
1:
Obstetric
history
and
baseline
characteristics
of
the
two
study
groups
Table
1
shows
a
significant
statistical
difference
between
Group
A
and
B
regarding
obstetric
history.
In
case
of
parity,
Group
A
was
comprised
of
comparatively
higher
percentages
of
nulliparous
and
primiparous
subjects
while
multiparity
was
on
the
higher
side
in
Group
B
(
p=
0.000).
Likewise,
Group
B
subjects
had
significantly
higher
number
of
abortions
(especially
multiple
abortions)
than
Group
A
(p=
0.007)
as
well
as
multiple
caesarean
sections
(p=0.000).
53.3
%
(n=128)
in
Group
B
were
on
Insulin
supplementation
while
the
rest
were
on
oral
hypoglycemic
agents.
All
subjects
in
Group
A
were
on
oral
hypoglycemic
agents.
OGTT
was
positive
for
all
subjects
in
Group
A
while
negative
for
those
in
Group
B
(probably
owing
to
their
medications).
Click
here
for
Table
2:
Neonatal
status
Table
2
shows
the
neonatal
statuses
in
both
groups.
There
was
statistically
higher
complications
in
Group
B
(p=0.033)
and
slightly
higher
birth
weight
(p=0.02)
as
compared
to
Group
A,
however
there
were
no
statistically
significant
differences
in
the
APGAR
scales.
Figure
1:
Types
of
delivery
(percentages)
in
both
groups
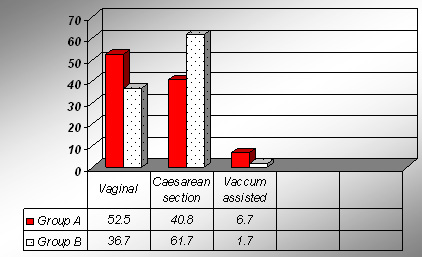
Figure
1
depicts
the
variations
in
the
modes
of
delivery
for
both
groups.
While
group
A
had
significantly
higher
percentage
of
vaginal
deliveries
and
vacuum
deliveries,
group
B
could
afford
more
caesarean
sections
(p=0.000,
0.006
and
0.000
respectively).
However
there
were
no
significant
differences
in
the
weeks
of
delivery
(preterm
vs
term)
amongst
both
groups.
The
aim
of
our
registry
was
to
identify
any
key
differences
between
T2DM
and
GDM
cases,
and
the
related
delivery
complications
and
neonatal
statuses.
As
opposed
to
the
meta-
analysis
reports
of
14
studies
done
by
Hai-Qing
Wang,
Han-Lin
Lai,
Yi
Li
et
al
in
2015(8),
our
study
did
not
show
any
significant
risk
effect
for
impaired
Glucose
tolerance
as
a
predictor
for
Large
for
Gestational
Age
(LGA).
Fetal
growth
is
mainly
dependent
on
interactions
of
maternal
and
fetal
endocrine
statuses
and
genetic
predispositions.
Higher
amount
of
maternal
blood
sugar
levels
in
turn
exposes
the
fetus
to
higher
levels
of
glucose
leading
to
fetal
lipogenesis
and
excessive
growth.(9)
In
our
study,
it
was
shown
that
the
average
birth
weight
was
statistically
higher
in
known
diabetics
than
gestational
diabetics.
Earlier
studies
have
proved
that
achievement
of
glucose
control
in
women
with
at
least
one
OGTT
value
decreased
adverse
neonatal
outcomes
to
near
baseline
level.(10,11,12)
However
our
study
has
shown
that
chronicity
of
hyperglycemic
status
significantly
increases
adverse
neonatal
outcomes
(p=0.033).
Recent
studies
have
confirmed
in
mouse
models
that
maternal
type
2
diabetes
mellitus
causes
heart
defects
in
the
developing
embryo
manifested
with
oxidative
stress,
endoplasmic
reticulum
stress,
and
excessive
apoptosis
in
heart
cells.(13)
Our
trial
has
shown
that
though
congenital
heart
defects
(especially
septal
defects)
were
common
in
both
groups,
offspring
of
females
with
either
overt
diabetes
or
gestational
diabetes,
but
more
frequent
among
the
offspring
of
mothers
with
overt
T2DM
(8%
vs
2%,
in
Group
B
and
Group
A
respectively).
Even
though
the
differences
between
APGAR
scores
at
birth,
5
minutes
and
10
minutes
weren't
statistically
significant,
it
was
noted
that
while
those
in
Group
A
born
with
low
scores
recovered
rapidly,
the
recovery
was
late
in
group
B.
New
meta-analysis
done
by
Jared
T.
Rockner
et
al
(14)
from
25
studies
has
shown
that
women
with
1
abnormal
value
on
3-
h,
100
g
OGTT
have
a
significantly
increased
risk
for
poor
outcomes
comparable
with
women
who
have
gestational
diabetes
mellitus.
Even
though
our
study
hasn't
included
any
similar
subjects
we
have
been
able
to
conclude
that
though
both
groups
require
good
management,
more
care
needs
to
be
given
to
those
with
previous
history
of
T2DM
even
if
their
OGTT
is
negative.
Along
with
medications,
dietary
control
and
exercise
shall
make
for
better
management.
(15)
Hyperglycemia
with
pregnancy
is
a
steadily
increasing
problem
that
can
seriously
affect
both
mother
and
baby
as
shown
in
the
present
study,
however,
there
were
no
significant
differences
in
the
weeks
of
delivery
(preterm
vs
term)
amongst
this
group
of
people.
However
our
study
has
shown
that
chronicity
of
hyperglycemic
status
significantly
increases
adverse
neonatal
outcomes
especially
in
regards
to
septal
defects.
The
limitation
of
the
study
lies
in
the
fact
that
this
was
a
single
centre
trial
with
no
randomization.
Also,
a
thorough
analysis
of
all
baseline
characteristics
and
clinical
presentations,
as
well
as
adverse
event
log
needs
to
be
maintained.
1.
American
Diabetes
Association.
Diagnosis
and
classification
of
diabetes
mellitus.
Diabetes
Care
2013;36(suppl
1):S67-74.
2.
CDC
3.
Wendland
EM,
Torloni
MR,
Falavigna
M,
Trujillo
J,
Dode
MA,
Campos
MA,
et
al.
Gestational
diabetes
and
pregnancy
outcomes-
a
systematic
review
of
the
World
Health
Organization
(WHO)
and
the
International
Association
of
Diabetes
in
Pregnancy
Study
Groups
(IADPSG)
diagnostic
criteria.
BMC
Pregnancy
Childbirth
2012;12:23
4.
Wong
T,
Ross
GP,
Jalaludin
BB,
Flack
JR.
The
clinical
significance
of
overt
diabetes
in
pregnancy.
Diabet
Med
2013;30(4):468-74
5.
Diabetes
Prevention
Program
(DPP)
Research
Group.
The
Diabetes
Prevention
Program
(DPP):
description
of
lifestyle
intervention.DiabetesCare
2002;25:2165-2171
6.
Alberti
KG,
Zimmet
PZ:
Definition,
diagnosis
and
classification
of
diabetes
mellitus
and
its
complications.
I.
Diagnosis
and
classification
of
diabetes
mellitus
provisional
report
of
a
WHO
consultation.
Diabet
Med
15:539-553,
1998
7.
BMJ
2-
Recommendations
for
diagnosis
of
glucose
intolerance
in
Pregnancy-
May
2016
8.
Hai-Qing
Wang,
Han-Lin
Lai,
Yi
Li,
Qi-Fei
Liu,
Shuang
Hu,
Li
Li:
The
Relationship
between
Maternal
Gestational
Impaired
Glucose
Tolerance
and
Risk
of
Large-for-Gestational-Age
Infant:
A
Meta-Analysis
of
14
Studies.
J
Clin
Res
Pediatr
Endocrinol
2016;
8:
264-269
9.
Segregur
J,
Bukovic
D,
Milinovic
D,
Oreskovic
S,
Pavelic
J,
Zupic
T,
Persec
J,
Pavic
M.
Fetal
macrosomia
in
pregnant
women
with
gestational
diabetes.
Coll
Antropol
2009;33:1121-1127.
10.
Vambergue
A,
Nuttens
MC,
Verier-Mine
O,
Dognin
C,
Cappoen
JP,
Fontaine
P.
Is
mild
gestational
hyperglycaemia
associated
with
maternal
and
neonatal
complications?
The
Diagest
Study.
Diabet
Med
2000;17:203-208.
11.
Berkus
MD,
Langer
O.
Glucose
tolerance
test:
degree
of
glucose
abnormality
correlates
with
neonatal
outcome.
Obstet
Gynecol
1993;81:344-348.
12.
Lindsay
MK,
Graves
W,
Klein
L.
The
relationship
of
one
abnormal
glucose
tolerance
test
value
and
pregnancy
complications.
Obstet
Gynecol
1989;73:103-106.
13.
Yanqing
Wu,
E.
Albert
Reece,
Jianxiang
Zhong,
et
al.
Type
2
diabetes
mellitus
induces
congenital
heart
defects
in
murine
embryos
by
increasing
oxidative
stress,
endoplasmic
reticulum
stress,
and
apoptosis.
American
Journal
of
Obstet
and
Gynecol
2016;215:
366
e1-
366e10.
14.
Jared
T.
Roeckner
,
Luis
Sanchez-Ramos,
Rubymel
Jijon-Knupp,
et
al
.Single
abnormal
value
on
3-hour
oral
glucose
tolerance
test
during
pregnancy
is
associated
with
adverse
maternal
and
neonatal
outcomes:
a
systematic
review
and
metaanalysis.
American
Journal
of
Obstet
and
Gynecol
2016;
215:287-297
15.
National
Institute
for
Health
and
Care
Excellence
(UK);
Diabetes
in
Pregnancy:
Management
of
Diabetes
and
Its
Complications
from
Preconception
to
the
Postnatal
Period.
NICE
Guideline
No:3,
2015:
Feb.
|
|
.................................................................................................................

|
| |
|

