|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................
|
Original
Contribution/Clinical Investigation
|
|

|
<-- Turkey -->
Preoperative
management of sickle cell patients with hydroxyurea
[pdf version]
Mehmet Rami Helvaci,
Sedat Hakimoglu, Mehmet Oktay Sariosmanoglu,
Suleyman Kardas, Beray Bahar, Merve Filoglu,
Ibrahim Ugur Deler, Duygu Alime Almali, Ozcan
Gokpinar, Ozlem Celik, Aynur Ozbay, Ozgun Ilke
Karagoz, Seher Aydin
<-- Ethiopia-->
Khat
(Catha edulis) chewing as a risk factor of low
birth weight among full term Newborns: A systematic
review
[pdf version]
Kalkidan Hassen
<-- Australia -->
Chronic
pain review following Lichtenstein hernia repair:
A Personal Series
[pdf
version]
Maurice Brygel,
Luke Bonato, Sam Farah
<-- Saudi Arabia -->
Assessment
of Health Status of Male Teachers in Abha City,
Saudi Arabia
[pdf
version]
Ali Mofareh Assiri,
Hassan M. A. Al-Musa
|
|
........................................................ |
Evidence
Based Medicine
........................................................
Medicine and Society
........................................................
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| October 2015 -
Volume 13 Issue 7 |
|
|
Chronic pain review following
Lichtenstein hernia repair:
A Personal Series
Maurice
Brygel (1)
Luke Bonato (2)
Sam Farah (3)
(1) Mr Maurice Brygel MBBS FRACS General Surgeon,
Director Melbourne Hernia Clinic, Masada hospital,
Melbourne Victoria,
Australia
(2) Dr Luke J Bonato MBBS
Surgical HMO,
Melbourne Victoria,
Australia
(3) Dr Sam S Farah, MBBS(Hons)
Master of Medicine (Clinical Epidemiology)
Student Intern, Southern Health, Melbourne
Victoria,
Australia
Correspondence:
Mr Maurice Brygel 26 Balaclava Road East St
Kilda Vic 3183
Australia
Ph: +61 3 9525 9077
Fax: +61 3 9527 1519
Email: mbrygel@netspace.net.au
|
Abstract
Introduction:
Chronic groin pain is both a topical subject
and important outcome measurement following
inguinal hernia repair. It has been suggested
its incidence is related to the management
of the nerves of the inguinal canal as
well as the type of mesh used and methods
of fixation for both open and laparoscopic
surgery.
The level of pre-operative
and post operative pain, its duration
as well as complications may all be factors
in predicting whether chronic pain may
develop. The method of measurement of
chronic pain is itself a contentious issue.
It is now apparent that the measurement
of activity and functional status as well
as qualitative measures is important.
Uniform methods
of assessing chronic post-operative pain
have been proposed.
Methods:
A retrospective study reviewing a consecutive
series of Lichtenstein repairs performed
by a single experienced hernia surgeon
was carried out. 248 inguinal hernia patients
operated on in 2005 were reviewed. Patients
were contacted via telephone at a median
of 50 months. A recently validated inguinal
pain questionnaire was used to assess
the incidence of chronic pain.
Results: 185
(75%) patients were able to be contacted
for follow-up, making a total of 213 inguinal
hernia repairs (including bilateral hernias).
At the time of review 3% of patients reported
having pain. No patients reported that
pain or discomfort was limiting their
work, exercise or activities of daily
living. No patients had disabling pain.
Conclusion:
Chronic pain did not appear to be a major
problem within this cohort of patients.
The Lichtenstein technique can produce
favourable results in terms of chronic
pain for unilateral, bilateral and recurrent
inguinal hernias in an unselected group
of patients with the usual mix of risk
factors and complications.
Key words:
Inguinal hernia, Lichtenstein, Local anaesthesia,
Chronic pain, Bilateral inguinal hernia,
Recurrent inguinal hernia
Abstract presentation
delivered to:
The Royal Australasian College Of Surgeons
Annual Scientific Congress, Perth, May
2010.
The American Hernia Society, Hernia Repair
Conference 2010, Orlando, Florida, March
2010.
|
Inguinal hernia repairs are one of the most
common surgical procedures(1). The pre-eminent
status of the original Lichtenstein technique
has been challenged with the introduction of
other open and laparoscopic techniques, lightweight
meshes and new methods of fixation with absorbable
tackers and tissue glues. While there has been
significant improvement in recurrence rates
with most types of mesh repair(2), a variable
and worrying incidence of chronic pain following
open and laparoscopic repair of inguinal hernias
has been documented(3).
There is still controversy regarding the true
incidence of chronic pain. The lack of uniform
definitions and interpretation as well as different
methods of assessment has lead to this(4-6).
Mild, moderate and severe pain has been reported
to have a prevalence of 0.7% to 43.3%(3), with
some treating the presence of pain as a dichotomous
(yes/no) entity.(7) An overall prevalence of
0.5 - 6% of severe debilitating pain affecting
normal daily activities and work has been reported(3).
It has also been suggested that the rates of
severe chronic pain are lower with laparoscopic
repair, compared with Lichtenstein repair or
other open techniques, as well as being associated
with earlier return to work and normal activities(8).
This however is associated with more adverse
events during surgery(9) as well as higher rates
of visceral injury(10).
Other factors such as patient profile, the
level of pre-operative pain, type of hernia,
post-operative pain and complications are also
being assessed as to their significance in assessing
the risk of the development of chronic pain(8).
Many methods including numerical and behavioural
rating scales have been used to assess the levels
of chronic pain(11), attesting to the difficulty
in assessment and interpretation. Standardization
of methods of measuring results is required(7).
Franneby's(11) validated chronic inguinal pain
questionnaire (IPQ) was used in this study.
This was chosen because of the comprehensive
but simple nature of the questionnaire. This
also incorporated pain behavior rather than
numbers. The IPQ also addressed many of the
issues surrounding this difficult concept, and
went a great way towards providing accurate
assessment.
Many of the multicentre trials used in larger
systematic reviews(10) that govern current guidelines(12)
incorporate many different surgeons of varying
levels of experience(9). To gain further insight
a consecutive series of patients operated on
using the Tension Free Lichtenstein Technique
(TFLT) with local anaesthesia and standard mesh
in 2005 by a single experienced hernia surgeon
were reviewed.
The primary objective of this study was to
assess the incidence of chronic pain, using
a validated inguinal pain questionnaire(11).
This series aims to address the issues previously
raised when investigating the incidence of chronic
pain(13), in particuar inadequate analysis.
The Lichtenstein technique(14) was used in a
consecutive series of patients with unilateral,
bilateral and recurrent inguinal hernias.
Approval
was
obtained
from
The
Avenue
Hospital
Human
Research
Ethics
Committee,
Ramsay
Health,
Melbourne,
Australia.
Patients
Selection
&
Baseline
Data
All
patients
who
underwent
a
primary
inguinal
hernia,
bilateral
inguinal
hernia,
or
recurrent
inguinal
hernia
repair
in
2005
were
included.
Patients
were
then
contacted
in
2009,
at
a
median
of
50
months
post-operatively
by
one
of
the
research
team.
The
follow-up
rate
was
75
%.
An
extensive
interview
based
on
Franneby's
IPQ(11)
was
conducted.
A
review
of
the
patient's
medical
records,
together
with
audit
forms
completed
at
the
time
of
operation
was
undertaken.
The
level
of
pre-operative
pain,
co-morbidities
and
type
and
size
of
the
hernia
had
been
recorded
pre-operatively.
The
method
of
repair,
mesh
and
fixation
used,
together
with
the
management
of
the
nerves
was
documented.
The
post-operative
complications,
post-operative
pain,
analgesic
requirements,
patient's
interpretation
of
the
pain,
and
return
to
normal
activities
and
work
had
been
documented
during
the
routine
post-operative
visits.
The
level
of
analgesics
required
post-operatively
and
return
to
normal
activities
was
reviewed.
Inguinal
Pain
Questionnaire
(IPQ)
The
IPQ
uniquely
explored
pain
intensity
rather
than
its
presence
or
absence.
This
allowed
for
a
more
meaningful
examination
of
pain,
and
pain
behavior.
The
IPQ
measured
•
Pain
and
its
impact
on
daily
activities
was
examined
across
four
different
periods:
preoperatively,
post-operatively,
time
of
interview,
and
the
week
preceding
the
interview,
using
the
following
scale;
i.
No
Pain
ii.
Pain
present
but
can
easily
be
ignored
iii.
Pain
present,
cannot
be
ignored,
but
does
not
interfere
with
everyday
activities
iv.
Pain
present,
cannot
be
ignored,
interferes
with
concentration
on
chores
and
daily
activities
v.
Pain
present,
cannot
be
ignored,
interferes
with
most
activities
vi.
Pain
present,
cannot
be
ignored,
necessitates
bed
rest
vii.
Pain
present,
cannot
be
ignored,
prompt
medical
advice
sought
•
When
pain
ceased.
•
How
often
had
the
participant
felt
pain
in
the
operate
groin
during
the
past
week,
and
how
long
they
may
have
lasted.
•
Current
analgesia
requirements.
•
Activities
of
daily
life
associated
questions.
•
Any
work
limitations.
The
Lichtenstein
Technique(14)
Anaesthesia
All
repairs
were
carried
out
using
Local
Anaesthetic
(LA)
infiltration
and
light
intravenous
sedation,
including
Fentanyl,
Propofol
or
Midazolam
and
anti-inflammatory
agents.
The
combination
used
depended
largely
on
the
anaesthetist's
preference.
A
mixture
of
Lignocaine
2%
with
Adrenaline
1:
200,000
and
plain
Bupivacaine
0.5%
were
used.
LA
was
directly
infiltrated
into
the
skin
and
subcutaneous
tissues
after
an
initial
dose
of
sedation.
The
sedation
avoided
the
possible
discomfort
of
the
injections.
The
ilioinguinal
nerve(IIN)
and
the
iliohypogatric
nerves
(IHN)
were
blocked
by
introducing
the
LA
deep
to
the
external
oblique
aponeurosis
under
direct
vision.
This
gave
rapid
anaesthesia
and
displaced
the
IIN
and
IHN
from
the
external
oblique
making
direct
injury
to
the
nerves
and
their
perineurium
less
likely.
The
LA
helped
identify
and
dissect
the
tissue
planes
as
it
was
injected
around
the
hernial
sac
and
cord
and
into
the
region
of
the
genital
division
of
the
GFN.
A
formal
ilio-inguinal
nerve
(IIN)
block
at
the
anterior
superior
iliac
spine
was
not
performed,
as
in
the
surgeon's
experience
patients
frequently
complained
of
post-operative
pain
at
the
site
of
injection.
Moreover,
this
technique
takes
longer
to
become
effective
and
adds
to
the
overall
volume
of
LA
required.
The
Nerves
The
identification
and
management
of
the
nerves
was
recorded.
An
attempt
was
made
to
identify
all
3
nerves.
However
an
extensive
search
was
not
carried
out
as
this
could
increase
tissue
trauma
and
possibly
damage
the
nerves.
In
the
majority
of
cases,
all
nerves
were
identified
and
spared.
If
the
nerve
had
been
traumatised
or
was
compromised
by
the
mesh
or
suturing,
it
was
dissected
back
to
the
muscle,
divided
and
removed
totally,
(neurectomy).
Diathermy
or
ligation
of
the
stump
was
not
employed.
The
IIN
was
usually
not
separated
from
the
cord.
Care
was
taken
in
closing
the
external
oblique
to
avoid
entrapping
the
IIN.
Surgical
technique:
The
Lichtenstein
technique
has
been
well
described(14).
Some
important
aspects
of
the
technique
and
possible
differences
include:
•
No
diathermy
was
used;
it
is
believed
this
could
cause
tissue
and
nerve
damage
setting
up
a
neuropathic
and
nocioceptive
inflammatory
response.
•
Adrenaline
kept
the
blood
loss
to
a
minimum.
•
Sharp
dissection
was
used
to
reduce
trauma.
•
The
Local
Anaesthetic
technique
requires
a
gentler
dissection.
•
For
indirect
hernias
the
sac
was
either
excised
or
reduced
(especially
for
sliding
hernias).
•
For
direct
hernias
the
sac
was
reduced.
•
Any
additional
lipoma
of
the
cord
was
always
excised.
•
A
standard
Polypropylene
mesh
was
used
Prolene
(trademark)
mesh,
Polypropylene,
non-absorbable
synthetic
surgical
mesh,
Johnson
&
Johnson.
•
A
standard
skin
stapler
(Appose
35w
auto
suture)
was
used
to
fix
the
mesh
to
the
inguinal
ligament
as
per
the
Lichtenstein
technique.
The
mesh
was
placed
well
medial
to
pubic
tubercle,
but
the
staples
were
placed
well
away
from
the
pubic
tubercle.
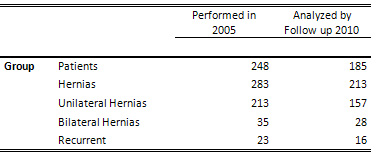
A
total
of
248
patients
were
operated
on
in
2005.
This
equated
to
283
hernias
including
35
bilateral,
and
23
recurrences.
185
patients
were
contacted
in
2010.
This
equated
to
213
hernia
repairs
with
28
bilateral
and
16
recurrences
equating
to
a
follow-up
rate
of
75%
(Table
1).
Table
1:
Number
of
Patients,
and
distribution
of
hernia
subtypes
Patient
demographics
(of
original
cohort)
Age
distribution
was
between
18
-
90
years.
The
majority
between
50
-
60
years
of
age
n
=
73
(28.85%).
241
(97%)
of
the
patients
were
male,
and
7
(3%)
were
female.
Inguinal
Pain
Questionnaire
(IPQ)
67%
(n
=
124)
of
patients
reported
pre
operative
pain.
This
ranged
in
severity
between
pain
that
could
be
easily
ignored
(27%)
to
pain
which
required
hospitalization
(3%).
33%
(n
=
61)
of
patients
reported
no
pain
at
all.
Table
2:
Comparison
of
pain
ratings
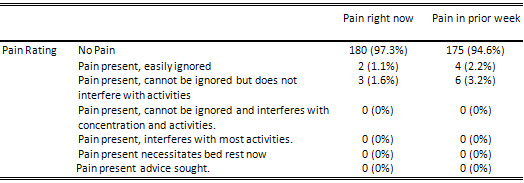
The
proportion
of
patients
with
pain
at
time
of
interview
was
3%
(95%
CI:
1%
to
5%,
P<0.001)
(Table
2).
Of
those
who
reported
pain:
•
1.1%
(n
=
2)
reported
that
their
pain
did
not
interfere
with
their
normal
activities
and
could
be
easily
ignored.
•
1.6%
(n=
4)
reported
having
pain,
which
did
not
interfere
with
their
activities
but
could
not
be
easily
ignored
(but
still
not
sufficient
to
require
analgesia).
"
No
patients
reported
pain
that
interfered
with
their
daily
activities
or
chores,
required
analgesia
or
required
medical
attention.
The
proportion
of
patients
with
pain
in
the
week
prior
to
interview
was
5%
(95%
CI:
2%
to
7%
P<0.001)
(Table
2).
Of
those
who
reported
pain:
•
2.2%
(n
=
4)
reported
that
their
pain
did
not
interfere
with
their
normal
activities
and
could
be
easily
ignored.
•
3.2%
(n=
6)
reported
having
pain,
which
did
not
interfere
with
their
activities
but
could
not
be
easily
ignored
(but
still
not
sufficient
to
require
analgesia).
•
No
patients
reported
pain
that
interfered
with
their
daily
activities
or
chores,
required
analgesia
or
required
medical
attention.
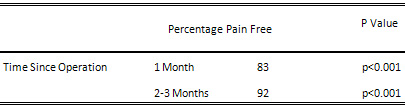
Resolution
of
pain
post-operatively
83%
(n
=154)
of
patients
were
pain
free
at
1
month
post
operatively,
and
92%
(n
=
170)
at
2-3
months
post-operatively
(Table
3).
Of
the
other
8%:
3%
had
intermittent
pain
that
lasted
for
6
months
(not
interfering
with
activities),
4%
of
patients
experienced
pain
for
up
to
12
months
(not
interfering
with
activities),
1%
had
pain
for
up
to
24
months
post-operatively.
Table
3:
Resolution
of
pain
post
operatively.
P
Values
calculated
when
cross-tabulated
against
preoperative
pain.
Post
Operative
Analgesia
Requirements
Patients
were
prescribed
paracetamol
and
codeine
tablets
(500mg
&
30mg
combination)
postoperatively,
and
were
advised
to
down
grade
to
the
500mg/8mg
combination
or
the
paracetamol
500mg
only
preparation
as
soon
as
pain
allowed
or
if
they
were
having
side
effects
from
the
analgesia.
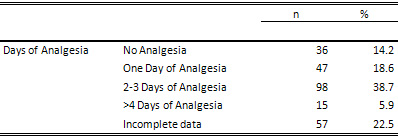
Table
4:
Post
Operative
Analgesia
Requirements
Functional
status
questions
(at
time
of
interview
and
previous
week)
•
100%
(n=185)
of
patients
had
no
pain
when
getting
up
from
a
low
chair.
•
97.8%
(n=180)
of
patients
reported
no
pain
when
sitting
for
more
than
half
an
hour.
•
98.4%
(n=182)
182
of
patients
did
not
experience
any
pain
or
discomfort
when
standing
for
more
than
half
an
hour.
•
98.9%
(n=183)
of
patients
were
able
to
go
up
and
down
stairs
without
experiencing
any
pain
in
the
groin.
•
98.4%
(n=182)
had
no
pain
when
driving.
Complications:
•
None
of
the
patients
with
significant
complications
developed
significant
chronic
pain
or
disability.
•
One
patient
re-operated
on
for
bleeding,
due
to
anti-coagulation
following
embolus,
had
occasional
discomfort.
•
One
patient
who
needed
removal
of
a
staple
from
the
mesh
had
no
further
pain
•
One
patient
who
required
prostatectomy
had
no
further
pain
•
Continuing
audit
over
many
years
showed
these
to
be
one
off
events
•
The
patients
with
seromas
and
superficial
infections
had
no
further
problems,
as
did
the
patients
who
developed
recurrences,
which
were
repaired.
Treatment
of
Nerves
The
IIN
was
identified
in
approximately
80%
of
cases.
In
approximately
10%
of
these
cases
when
the
nerve
was
identified
a
neurectomy
was
performed,
either
as
a
result
of
accidental
damage,
excessive
dissection
or
the
fear
of
entrapment
in
the
mesh.
The
IHN
was
identified
less
frequently
in
approximately
70%
of
cases.
It
was
divided
accidently
or
intentionally
in
approximately
10%
of
these
cases
mainly
to
avoid
entrapment
in
fixation
of
the
mesh
as
it
emerged
medially
from
the
internal
oblique
aponeurosis.
The
GFN
was
always
identified
with
the
cremasteric
vessels
and
only
divided
and
ligated
in
a
few
cases
when
these
vessels
were
ligated
for
technical
reasons.
The
vast
majority
of
unilateral,
bilateral
or
recurrent
hernia
patients
at
50
months
had
no
significant
pain
or
disability.
None
reported
that
their
exercise,
activities
or
work
were
limited
by
pain.
Few
reported
the
need
for
analgesia
on
any
consistent
basis.
The
incidence
of
moderate
or
significant
chronic
pain
was
less
than
1%,
which
the
authors
felt
would
be
pain
that
interfered
with
activities
or
required
regular
analgesia.
In
view
of
the
high
incidence
of
chronic
pain
and
disability
in
some
series(9)
there
have
been
many
attempts
to
identify
possible
risk
factors
and
surgical
materials
and
techniques
that
might
predict
its
development.
This
study,
because
of
the
low
incidence
of
chronic
pain
was
unable
to
identify
any
previously
reported
risk
factors,
despite
the
cohort
being
a
consecutive
series
of
patients.
The
authors
have
sought
to
analyze
and
explain
why
these
results
may
be
different
to
others.
The
wide
discrepancy
in
the
reported
incidence
of
chronic
pain
after
inguinal
hernia
repair
results
needs
to
be
explained
particularly
as
recommendations
may
be
based
on
these
results(12).
It
has
been
pointed
out
that
aggressive
early
therapy
for
post-operative
pain
is
indicated,
since
the
intensity
of
post-operative
pain
correlates
with
the
risk
of
developing
chronic
pain(15).
Pre-operative
LA
was
used
routinely
as
part
of
this
regime
ensuring
the
patient
is
pain
free
for
at
least
4-10
hours
and
is
able
to
travel
home
in
comfort
without
the
need
for
analgesics.
It
was
noted
in
this
series
that
the
vast
majority
of
the
patients
did
not
consider
early
post-operative
pain
to
be
a
major
factor.
The
use
of
post-operative
analgesics
was:
14%
needed
no
painkillers,
18%
used
pain
killers
for
1
day,
and
the
majority
for
just
a
few
days
to
a
week.
Even
those
who
felt
post-operative
pain
to
be
an
issue
did
not
develop
significant
chronic
pain.
Those
patients
who
did
complain
of
post-operative
pain
at
one
week
were
kept
under
review
until
the
pain
resolved.
The
low
incidence
of
significant
early
post-operative
pain
or
perceived
pain
and
the
minimal
need
for
analgesia
in
many
patients,
may
be
of
significance.
The
LA
may
contribute
to
this
early
low
level
of
pain
and
may
be
a
significant
factor,
particularly
as
pre-emptive,
peri-operative
and
post-operative
analgesia
considered
under
the
title
"multimodal
analgesia"
are
being
assessed
as
factors
in
preventing
chronic
pain(16).
Furthermore
with
LA
many
of
the
early
side
effects
of
general
anaesthesia
such
as
nausea,
vomiting,
and
acute
retention
of
urine
are
reduced.
Less
intensive
post-operative
nursing,
including
airway
care
is
required.
The
majority
of
patients
go
home
within
3
hours
of
surgery.
The
long
acting
LA
lasts
from
4-10
hours
and
many
patients
do
not
need
further
analgesia.
Many
patients
preferred
the
LA
because
of
previous
problems
with
general
anaesthesia.
Many
of
the
studies
of
the
Lichtenstein
method
have
not
used
local
anaesthesia
as
described
by
Lichtenstein.
This
may
diminish
the
benefits
of
the
original
repair
and
also
account
for
a
higher
incidence
of
chronic
pain
found
in
some
series.
The
nerves
The
management
of
the
3
major
nerves
of
the
inguinal
canal
has
been
considered
to
be
a
factor
in
chronic
pain(17).
This
study
showed
a
low
incidence
of
chronic
pain
despite
the
IIN
and
IHN
not
being
formally
identified
or
damaged
and
removed
in
up
to
20%
of
cases.
Extensive
studies
concluded
that
identification
and
preservation
of
all
3
nerves
of
the
inguinal
canal
reduces
chronic
incapacitating
groin
pain.
Mesh,
staples
Mesh
and
staples
have
also
been
widely
implicated
as
significant
factors
in
the
development
of
chronic
pain
leading
to
a
variety
of
new
lighter
weight
meshes,
staples
and
glues(16).
This
series
with
its
low
incidence
of
significant
chronic
pain
using
a
standard
Polypropylene
mesh
and
non-absorbable
staples
raises
the
question
as
to
the
role
of
the
mesh
in
the
development
of
chronic
pain.
Positive
Results
The
positive
results
identified
in
this
series
may
be
due
to
the
following
factors;
LA
infiltration
allowing
simpler
dissection
of
the
tissues
with
less
trauma.
Diathermy
is
not
used,
possibly
reducing
the
inflammatory
response
around
the
nerve
endings,
a
possible
cause
of
nocioceptive
pain.
Identification
and
management
of
the
nerves(12).
The
use
of
the
open
skin
stapler
to
fix
the
mesh
(appose
ulc
35w
auto
suture).
The
early
supervised
management
of
post-operative
pain,
including
contact
by
telephone
by
the
surgeon
with
all
patients
the
day
following
surgery
to
adjust
analgesia
and
give
support
as
necessary.
If
the
results
vary
so
much,
is
it
possible
to
attribute
chronic
pain
to
the
mesh/fixation
alone?
The
results
in
this
study,
suggest
that
mesh
and
staples
may
not
be
the
main
factors
in
determining
the
incidence
of
chronic
pain,
and
could
it
just
be
the
way
the
materials
are
used?
Does
it
depend
on
the
technique
and
the
surgeon?
There
is
strong
evidence
from
this
series,
using
a
validated
inguinal
pain
questionnaire,
that
a
Lichtenstein
repair
using
local
anaesthesia
can
achieve
a
low
incidence
of
chronic
post-operative
pain.
Those
few
patients
who
did
report
pain,
did
not
have
any
associated
significant
morbidity
or
impairment
of
activities
of
daily
living.
No
obvious
risk
factors
were
identified
as
predicting
or
associated
with
chronic
pain.
There
appeared
to
be
no
reason
to
alter
the
approach
used
to
manage
the
nerves,
the
type
of
mesh
or
its
method
of
fixation,
in
terms
of
chronic
pain.
The
validated
IPQ
provides
a
more
detailed
appreciation
of
pain
behaviour.
These
types
of
pain
measures
will
be
useful
in
the
future
to
help
in
assessing
the
role
of
surgical
risk
factors
and
techniques
as
a
cause
for
chronic
pain.
More
detailed
investigation
using
these
validated
tools
is
required
in
larger
prospective
studies,
to
provide
more
accurate
and
meaningful
comparisons
between
other
techniques
in
conjunction
with
greater
operator
experience.
1.
Kingsnorth
A,
LeBlanc
K.
Hernias:
inguinal
and
incisional.
Lancet.
Nov
8
2003;362(9395):1561-1571.
2.
Bisgaard
T,
Bay-Nielsen
M,
Christensen
IJ,
Kehlet
H.
Risk
of
recurrence
5
years
or
more
after
primary
Lichtenstein
mesh
and
sutured
inguinal
hernia
repair.
British
Journal
of
Surgery.
Aug
2007;94(8):1038-1040.
3.
Kehlet
H.
Chronic
pain
after
groin
hernia
repair.
British
Journal
of
Surgery.
Feb
2008;95(2):135-136.
4.
Poobalan
AS,
Bruce
J,
King
PM,
Chambers
WA,
Krukowski
ZH,
Smith
WC.
Chronic
pain
and
quality
of
life
following
open
inguinal
hernia
repair.
British
Journal
of
Surgery.
Aug
2001;88(8):1122-1126.
5.
Bay-Nielsen
M,
Nilsson
E,
Nordin
P,
Kehlet
H,
Swedish
Hernia
Data
Base
the
Danish
Hernia
Data
B.
Chronic
pain
after
open
mesh
and
sutured
repair
of
indirect
inguinal
hernia
in
young
males.
British
Journal
of
Surgery.
Oct
2004;91(10):1372-1376.
6.
Condon
RE.
Groin
pain
after
hernia
repair.
Annals
of
Surgery.
Jan
2001;233(1):8.
7.
Kehlet
H,
Bay-Nielsen
M,
Kingsnorth
A.
Chronic
postherniorrhaphy
pain--a
call
for
uniform
assessment.
Hernia.
Dec
2002;6(4):178-181.
8.
Dickinson
KJ,
Thomas
M,
Fawole
AS,
Lyndon
PJ,
White
CM.
Predicting
chronic
post-operative
pain
following
laparoscopic
inguinal
hernia
repair.
Hernia.
Dec
2008;12(6):597-601.
9.
Langeveld
HR,
van't
Riet
M,
Weidema
WF,
et
al.
Total
extraperitoneal
inguinal
hernia
repair
compared
with
Lichtenstein
(the
LEVEL-Trial):
a
randomized
controlled
trial.
Annals
of
Surgery.
May
2010;251(5):819-824.
10.
McCormack
K,
Scott
NW,
Go
PM,
Ross
S,
Grant
AM,
Collaboration
EUHT.
Laparoscopic
techniques
versus
open
techniques
for
inguinal
hernia
repair.
Cochrane
Database
of
Systematic
Reviews.
2003(1):CD001785.
11.
Franneby
U,
Gunnarsson
U,
Andersson
M,
et
al.
Validation
of
an
Inguinal
Pain
Questionnaire
for
assessment
of
chronic
pain
after
groin
hernia
repair.
British
Journal
of
Surgery.
Apr
2008;95(4):488-493.
12.
Simons
MP,
Aufenacker
T,
Bay-Nielsen
M,
et
al.
European
Hernia
Society
guidelines
on
the
treatment
of
inguinal
hernia
in
adult
patients.
Hernia.
Aug
2009;13(4):343-403.
13.
Franneby
U,
Sandblom
G,
Nordin
P,
Nyren
O,
Gunnarsson
U.
Risk
factors
for
long-term
pain
after
hernia
surgery.
Annals
of
Surgery.
Aug
2006;244(2):212-219.
14.
Lichtenstein
S,
Amid,
Montlor.
The
tension
free
hernioplasty
(1989)
American
Journal
Of
Surgery
157:188-193.
.
American
Journal
of
Surgery.
1989(157):188-193.
15.
Kehlet
H,
Jensen
TS,
Woolf
CJ.
Persistent
postsurgical
pain:
risk
factors
and
prevention.
Lancet.
May
13
2006;367(9522):1618-1625.
16.
Aasvang
EK,
Gmaehle
E,
Hansen
JB,
et
al.
Predictive
risk
factors
for
persistent
postherniotomy
pain.
Anesthesiology.
Apr
2010;112(4):957-969.
17.
Caliskan
K,
Nursal
TZ,
Caliskan
E,
Parlakgumus
A,
Yildirim
S,
Noyan
T.
A
method
for
the
reduction
of
chronic
pain
after
tension-free
repair
of
inguinal
hernia:
iliohypogastric
neurectomy
and
subcutaneous
transposition
of
the
spermatic
cord.
Hernia.
Feb
2010;14(1):51-55.
|
|
.................................................................................................................

|
| |
|

