DASH
Diet: How Much Time Does It Take to Reduce Blood
Pressure in Pre-hypertensive and Hypertensive
Group 1 Egyptian patients?
Rehab Abdelhai (1)
Ghada Khafagy (2)
Heba Helmy (3)
(1) Dr. Rehab Abdelhai (MD) is Associate Professor
of Public Health at Faculty of Medicine, Cairo
University
(2) Dr. Ghada Khafagy (MD) is lecturer of Family
Medicine, at Faculty of Medicine, Cairo University
(3) Dr. Heba Helmy (MSc) is a Family Physician
at Family Health Unit, Ministry of Health, Egypt.
Correspondence:
Dr. Ghada Khafagy, M.D.
Department of Family Medicine,
Faculty of Medicine,
Cairo University
71st, Moez El-Dwla, Makram Ebeed,
Nasr city, Cairo
Egypt
Phone: +20 - (0)100 - 6393140
Email: ghada.khafagy@kasralainy.edu.eg;
ghadakhafajy@yahoo.com
|
Abstract
Background: Dietary
changes that lower blood pressure (BP)
have the potential to prevent hypertension
and more broadly to reduce BP, thus lowering
risks of BP-related complications. Evidence
shows that even a small reduction in BP
could have enormous benefits.
Objectives:
Evaluate the effect of Dietary Approaches
to Stop Hypertension (DASH) diet on normotensive
individuals; pre-hypertension and hypertensive
grade 1 patients as well as to identify
time needed for DASH to reduce BP in pre-hypertension
and hypertensive grade 1 patients.
Methods: This
study was a prospective interventional
study carried out on 120 participants
attending the out-patient clinic of a
family medicine unit, of Dakahlia governorate,
Egypt. Participants were equally distributed
into three groups; normotensive, pre-hypertensive
hypertensive grade 1 participants (40
in each group). Blood pressure and weight
and waist circumference (WC) were measured
at the beginning of the study then every
2 weeks for 16 weeks.
Results: Significant
reductions in systolic and diastolic BP
among pre-hypertension by (8.1, and 16.4
mmHg respectively with P < 0.001) and
hypertensive participants by (5.8, and
7.4 mmHg respectively with P < 0.001)
were observed. Reduction was greater in
the first 8 weeks and reached a plateau
after 12 weeks. BP decrease in normotensive
group was insignificant. Additionally,
there was insignificant reduction in weight
and WC among the 3 groups.
Conclusion: Adherence
to DASH diet has rapid and statistically
significant improvement in systolic and
diastolic blood pressure in hypertensive
grade 1 and pre-hypertensive participants.
Hence, DASH diet was found effective as
a first line intervention of elevated
blood pressure.
Key Words: DASH,
Diet, Blood Pressure, Hypertension, Egypt
|
The prevalence of prehypertension and hypertension
among Egyptian adults has been reported as 57.2%
and 17.6% respectively. Only 25.2% of the population
had normal blood pressure levels of <120/80
mmHg. The highest prevalence of hypertension
was found in Ismailia, Alexandria, Menya, Menoufia
and Luxor governorates. The prevalence of hypertension
among males and females was similar; however,
females had a lower prevalence of prehypertension,
and a higher prevalence of normal blood pressure,
than males (1).
The STEPwise survey conducted in 2011-2012
recorded that the percentage of adult population
with raised blood pressure, or currently on
medication for hypertension (SBP
> 140 and/or DBP >
90 mmHg), was 39.4%, with females showing higher
percentage (40.8%) than males (38.7%). The percentage
of population with raised blood pressure increased
gradually with age, with the highest percentage
(80.5%) among the age group of 55-65 years.
Overall, the mean blood pressure was found to
be 128/82 mmHg which is considered to be the
state of pre-hypertension (2).
There is a gradual increase in cardiovascular
risk as blood pressure (BP) increases above
even "normal" values of 115/75 mmHg.
For individuals aged 40 to 70 years, each increase
of 20 mmHg of systolic BP or 10 mmHg of diastolic
BP doubles the risk of cardiovascular disease
(CVD). In controlled clinical trials, treatment
of hypertension reduces the risk of congestive
heart failure by 50%, stroke by 35% to 40% and
myocardial infarction by 20% to 25% ( 3).
Dietary factors have an important role in BP
homeostasis. In non-hypertensive and pre-hypertensive
individuals, dietary changes that lower BP have
the potential to prevent hypertension and more
broadly to reduce BP and thereby lower the risk
of BP-related complications. Even an apparently
small reduction in BP, if applied to an entire
population, could have an enormous beneficial
impact. It has been estimated that a 3 mm Hg
reduction in systolic BP could lead to an 8%
reduction in stroke mortality and a 5% reduction
in mortality from coronary heart disease. In
uncomplicated stage I hypertension, dietary
changes can serve as initial treatment before
the start of drug therapy. Among hypertensive
individuals who are already on drug therapy,
dietary changes, particularly a reduced salt
intake, can further lower BP and facilitate
medication step-down. Therefore, the extent
of BP reduction from dietary therapies is greater
in hypertensive than in non-hypertensive individuals
(4).
Although elevated blood pressure can be lowered
pharmacologically, antihypertensive medications
may be costly, must often be used in combination
to achieve adequate blood pressure control,
and can be associated with adverse effects that
impair quality of life and reduce adherence
(5). Although the Dietary Approaches to Stop
Hypertension (DASH) diet and other healthy lifestyle
changes may not be enough to control severe
high blood pressure, yet they often lead to
reduced need for blood pressure-lowering medications
as well as lower doses of those medications
(6).
The DASH diet emphasizes fruits, vegetables,
and low fat dairy products; whole grains, poultry,
legumes, fish, and nuts, and is reduced in fats,
red meat, sweets, and sugar-containing beverages.
It is therefore rich in potassium, magnesium,
calcium, and fiber and reduced in total fat,
saturated fat, and cholesterol. It is also characterized
by slightly increased protein content. It is
likely that several aspects of the DASH diet,
rather than just one nutrient or food, reduces
blood pressure (7).
This study aimed at testing the following
hypothesis: Adherence to DASH diet causes
a significant reduction in systolic and diastolic
BP in both study groups (pre-hypertension and
hypertensive group 1 patients), and a non-significant
reduction among normotensive group. Therefore,
DASH diet can cause even more improvement in
other risk factors of hypertension. Hence this
study aimed at answering the following research
questions: Does DASH diet have an effect on
systolic and diastolic blood pressure in normotensive
individuals, pre-hypertension and hypertensive
group 1 patients, and how much time does the
DASH diet need to decrease BP in pre-hypertensive
and hypertensive patients?
1- Evaluate the effect of DASH diet
on normotensive individuals; pre-hypertension
patients and hypertensive grade 1 patients.
2- Assess time needed for DASH diet to
reduce the blood pressure in pre-hypertension
patients and hypertensive grade 1 patients.
Study
design:
The
study
employed
a
prospective
interventional
design
to
evaluate
the
effect
of
Dietary
Approaches
to
Stop
Hypertension
(DASH)
diet
on
Normotensive,
Pre-hypertension
and
Hypertensive
grade
1
patients.
Study
site
and
subjects:
The
study
was
conducted
in
a
family
medicine
unit
(FMU)
that
provides
primary
health
care
services
in
the
rural
area
of
Sherbeen,
of
Dakahlia
governorate,
Egypt.
The
study
site
was
purposefully
selected
because
it
serves
7
villages,
with
different
socioeconomic
levels.
Additionally,
the
unit
has
a
high
rate
of
outpatient
visitors
(average
30
person/day)
seeking
different
medical
services.
The
health
unit
was
visited
on
three
days
per
week
regularly
from
June,
2012
till
February,
2013.
An
advertisement
was
distributed
throughout
the
FMU,
announcing
to
all
clients
the
subject
of
research
and
its
benefits
to
help
control
blood
pressure.
The
inclusion
criteria
for
study
participants
were
as
follows:
Age
between
30
-
60
years;
systolic
blood
pressure
<160
mmHg,
and
diastolic
blood
pressure
<100
mmHg;
both
sexes;
participants
willing
to
follow
the
advice
related
to
life
style
modifications.
Exclusion
criteria
for
the
study
participants
were:
Any
age
below
30
years,
or
above
60
years,
grade
2
hypertension
(systolic
>
160
mmHg,
diastolic
>
100
mmHg),
patients
with
terminal
organ
failure,
history
of
major
cardiovascular
events
(cerebrovascular
accidents),
patients
with
renal
disease,
pregnant
women,
patients
taking
medications
that
would
alter
blood
pressure
as
oral
contraceptives
pills,
corticosteroids,
hormonal
replacement
therapy,
anti-depressive
medications,
routine
use
of
aspirin
or
non-steroidal
anti-inflammatory
drugs.
.
Study
participants
were
then
classified
into
three
groups,
Group
1:
normotensive
group
with
(systolic
<
120
mmHg,
diastolic
<
80
mmHg);
Group
2:
pre
hypertensive
group
with
(systolic
120
-
139
mmHg,
diastolic
80
-
89
mmHg);
and
Group
3
hypertensive
grade
1
group
with
(systolic
140
-
159
mmHg,
diastolic
90
-99
mmHg).
The
grade
of
the
disease
was
identified
from
the
FMU
patient
records.
Initial
recruitment
of
subjects
started
then
follow-up
continued
for
the
next
16
weeks
(every
2
weeks).
All
participants
underwent
focused
medical
examination
for
initial
screening
before
recruitment.
Sample
Size
and
technique:
The
sample
size
was
calculated
according
to
the
flow
of
FMU
clients
as
obtained
from
the
FMU
records.
The
number
of
clients
ranged
between
20-30
per
day,
with
average
of
400-600
visitors
/month.
For
the
purposes
of
the
study,
every
participant
needed
half
an
hour
to
fill
out
the
questionnaire
and
to
measure
BP,
weight,
height,
and
waist
circumference.
Hence
10
participants
were
recruited
per
day.
Enrolment
stopped
when
the
number
of
subjects
recruited
reached
a
predetermined
sample
size
of
120
equally
distributed
among
the
study
groups.
Using
a
systematic
random
technique
over
the
working
days,
every
5th
patient
was
approached
and
asked
first
verbally
for
consent
to
undergo
initial
screening
and
participate
in
the
study
if
found
to
be
eligible.
All
patients
fulfilling
the
inclusion
criteria
were
asked
to
share
their
telephone
numbers
with
the
research
team
for
ease
of
follow
up.
Participants
were
recruited
for
an
initial
duration
of
5
weeks.
At
the
end
of
the
initial
recruitment
phase
a
total
of
120
individuals
were
recruited
(40
in
each
group).
Study
tools
and
measurements:
a-
Structured
questionnaire:
A
pre-coded
structured
questionnaire
was
used
to
assess
the
socio-demographic
characteristics,
dietary
and
behavioral
information
as
well
as
medical
information.
Demographic
data
included
(age,
gender,
education,
occupation,
marital
status).
Behavioral
and
dietary
information
included
alcohol
intake,
physical
activities,
food
taste
preferences,
cigarette
smoking,
and
frequency
of
intake
of
various
kinds
of
foods.
All
participants
were
asked
about
the
previous
3-day
food
record
prior
to
their
participation
in
the
study.
During
the
first
encounter,
participants
were
interviewed
to
assess
if
their
diet
was
unchangeable,
using
their
3-day
food
record
as
a
basis
for
their
habitual
diet.
For
example,
if
they
felt
unable
to
decrease
their
salt
intake
or
increase
their
fruit
and
vegetable
intake
sufficiently,
then
they
were
excluded
from
the
study.
A
total
of
120
participants
who
were
judged
capable
of
making
the
necessary
dietary
changes
were
recruited
into
the
study.
.
b-
Anthropometric
measurements:
Anthropometric
measurements
were
completed
using
standardized
procedures
and
were
documented
in
a
special
checklist
developed
for
the
purpose
of
the
study.
•
The
waist
circumference
(WC)
was
measured
to
the
nearest
0.1
cm
using
a
non-stretchable
measuring
tape
passing
halfway
between
the
lower
border
of
the
ribs
and
iliac
crest,
with
the
tape
horizontal
through
the
umbilicus.
WC
was
measured
every
month
for
the
subsequent
4
months
of
the
study.
•
Body
weight
(WT)
was
measured
to
the
nearest
50
gram;
subjects
were
in
light
clothing
without
shoes,
and
a
standard
balance
scale
was
used.
Height
(HT)
was
measured
with
subjects
standing
fully
erect
on
a
flat
surface
looking
straight
ahead,
with
heels,
buttocks
and
shoulders
flat
to
the
wall,
without
shoes;
measurements
were
to
the
nearest
0.5
centimeter,
and
a
tape
was
used.
The
body
mass
index
(BMI)
was
calculated
as
the
weight
in
(kilograms)
divided
by
the
height
in
(meters
squared)
(kg/m2).
•
The
Blood
pressure
was
measured
in
the
right
arm,
with
the
participant
in
a
seated
posture
with
feet
on
the
floor
and
arm
supported
at
heart
level,
after
at
least
5
minutes
of
rest
(8).
An
appropriate
size
of
cuff
and
a
standard
mercury
sphygmomanometer
were
used.
A
large
size
cuff
was
used
with
obese
participants.
Two
readings
each
of
systolic
BP
(SBP)
and
diastolic
BP
(DBP)
were
recorded;
Participants
were
advised
to
evacuate
bladder
and
to
stop
consuming
coffee,
tea,
or
smoking
cigarettes,
for
at
least
30
minutes
before
the
BP
readings.
These
measurements
with
the
same
precautions
were
repeated
every
2
weeks
for
the
subsequent
4
months
of
the
study.
All
the
sphygmomanometers
were
checked
and
calibrated
before
use.
Study
Intervention:
The
DASH
diet
tool
as
proposed
by
Hinderliter
et
al,
2011
(7),
was
used.
The
diet
was
explained
on
the
first
day,
and
started
the
following
day
for
16
weeks.
Subjects
were
requested
to
build
up
the
diet
during
the
first
week
of
the
study
period
to
the
required
number
of
portion
sizes
for
a
DASH-style
diet,
which
they
would
then
maintain
for
the
further
study
period.
This
was
done
to
minimize
the
gastrointestinal
side
effects
of
suddenly
increasing
non-starch
polysaccharide.
The
participants
were
asked
to
come
to
the
FMU
every
2
weeks
to
check
their
blood
pressure,
and
for
counseling
and
discussions
regarding
the
diet.
Energy
balance
was
aimed
for,
and
the
importance
of
maintaining
a
constant
body
weight
was
stressed.
The
study
diet
was
based
on
the
DASH
intermediate
sodium
diet
but
altered
to
fit
participant's
food
preferences
and
portion
sizes.
Greatest
emphasis
was
placed
on
consuming
the
fruits,
vegetables
and
low-fat
dairy
foods,
whole
grains,
poultry,
fish,
as
well
as
the
salt
restriction
and
weight
maintenance.
The
importance
of
reducing
saturated
fat,
red
meat
and
refined
carbohydrate
and
increasing
complex
carbohydrate
intakes
was
also
stressed.
Suggestions
on
how
to
increase
fruit
and
vegetable
consumption
were
also
provided.
All
smokers
were
advised
to
quit
smoking,
and
counseling
on
smoking
hazards
was
conducted.
Instructions
were
given
regarding
reducing
sodium
intake.
The
level
of
sodium
intake
that
was
aimed
for
was
2300
mg
or
less
(1
teaspoonful),
which
was
the
intermediate
level
used
in
the
DASH
sodium
trial
(9).
Subjects
were
requested
to
avoid
foods
with
a
high
salt
content
and
not
to
add
salt
during
cooking
or
at
the
table.
They
were
shown
how
to
interpret
food
labels,
particularly
with
regard
to
sodium
content.
Guidance
as
to
how
to
add
flavor
without
using
salt
was
given.
Subjects
were
requested
to
restrict
their
coffee
and
tea
intake
to
not
more
than
six
cups
a
day.
If
their
habitual
intakes
were
higher
than
these
levels,
they
were
asked
to
reduce
to
these
recommended
levels.
Under
participant's
request,
diets
were
organized
in
sheets
according
to
their
needs.
Subjects
were
requested
to
keep
their
exercises
as
usual
without
any
changes.
Data
management
and
statistical
analysis:
The
pre-coded
questionnaires
were
entered
for
analysis
on
SPSS
package
version
11.0.
for
quantitative
data
analysis.
Simple
frequencies
were
used
for
data
checking.
According
to
Joint
National
Committee
on
the
Prevention,
Detection,
Evaluation,
and
Treatment
of
High
Blood
Pressure
(10)
all
of
the
following
cut-off
points
were
used
in
the
study:
•
Age
of
study
participants
was
categorized
into
2
age
groups,
below
35
years
old
and
above
35
years
old.
•
Hypertension
was
identified
according
to
the
following
criteria:
-
Normotensive
group
(systolic
<
120
mmHg,
diastolic
<
80
mmHg),
-
Pre-hypertension
group
(systolic
120
-
139
mmHg,
diastolic
80
-
89
mmHg),
-
Hypertensive
grade
1
(systolic
140
-
159
mmHg,
diastolic
90
-
99
mmHg).
Compliance
with
Ethical
Standards:
The
study
was
approved
by
the
Family
Health
and
Public
Health
Councils.
Selected
members
constituted
the
internal
review
board
to
guarantee
the
ethical
conformity
of
the
study.
Informed
verbal
consent
was
obtained
from
all
the
participants
before
recruitment
in
the
study,
after
explaining
the
objectives
of
the
work
and
procedures.
All
questionnaire
forms
and
clinical
sheets
were
coded
to
preserve
confidentiality
that
was
also
guaranteed
on
handling
the
data
base
according
to
the
revised
Helsinki
declaration
of
biomedical
ethics
(11).
All
participants
were
informed
about
the
results
of
their
medical
examination.
Those
who
were
found
hypertensive
grade
2
were
referred
to
the
unit
health
team
for
drug
prescription,
and
further
follow
up.
The
study
included
120
participants
of
which
56.7%
were
females.
Participants
were
equally
distributed
among
the
study
groups.
The
mean
age
of
participants
in
the
hypertensive
group
was
found
to
be
significantly
older
than
those
in
the
other
two
study
groups
with
a
mean
age
of
45.5
±
7.7
years
compared
to
39.5
±
8.3years
and
40.2
±
7.8
years
for
participants
in
the
normotensive
and
pre-hypertension
groups,
respectively
(P
=
0.001).
The
age
of
most
of
the
study
participants
were
more
than
35
years
old
(72.5%)
of
which
28.7%
were
normotensive,
31.1%
were
pre-hypertension
and
40.2%
were
hypertensive.
Only
46.6%
of
all
participants
had
higher
education,
of
which
32.1%
were
normotensive,
39.3%
were
pre-hypertension
and
28.6%
were
hypertensive.
Moreover
41.7%
of
all
participants
had
basic
education,
of
which
34.0%
were
normotensive,
28.0%
were
pre-hypertension
and
35.7%
were
hypertensive.
There
was
no
significant
difference
between
the
study
groups
regarding
gender,
marital
status,
education
or
occupation
[Table
1].
Table
1:
Socio-demographic
characteristics
of
the
study
participants
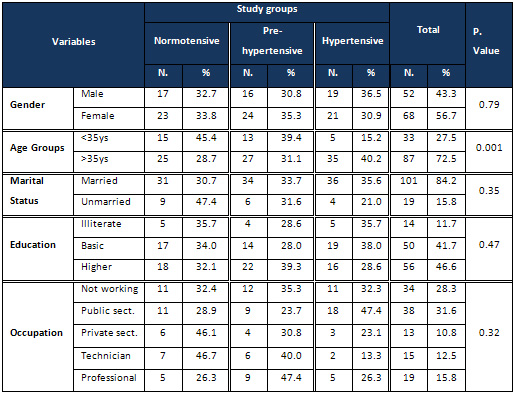
As
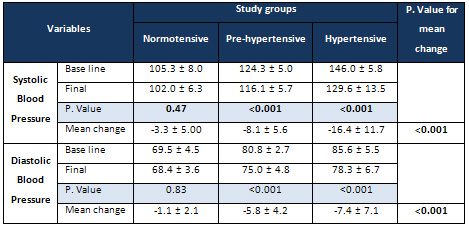
regards
systolic
blood
pressure
(SBP)
readings,
the
base
line
reading
for
normotensive
group
was
105.3
±
8.0
mmHg,
and
then
at
the
end
of
the
study
it
became
102.0
±
6.3
mmHg,
with
mean
change
3.3
±
5.0
mmHg.
For
the
pre-hypertension
group,
it
was
124.3
±
5.0
mmHg.
That
became
116.1
±
5.7
mmHg,
with
mean
change
8.1
±
5.6
mmHg.
As
for
the
hypertensive
group
it
was
146.0
±
5.8
mmHg,
and
became
129.6
±
13.5
mmHg,
with
mean
change
16.4
±
11.7
mmHg.
Although
there
was
no
significant
change
in
the
normotensive
group
readings
(P
=
0.47),
there
were
statistically
significant
changes
in
pre-hypertension
and
hypertensive
readings
(P
<0.001).
When
comparing
the
mean
change
in
systolic
blood
pressure
readings
among
all
study
groups,
a
highly
significant
difference
was
detected
(P
<
0.001)
with
the
hypertensive
group
showing
the
highest
reduction
followed
by
the
other
two
groups.
This
difference
was
found
across
the
three
groups
[Table
2].
Table
2:
Effect
of
DASH
diet
on
mean
systolic
and
diastolic
blood
pressure
readings
among
the
study
groups
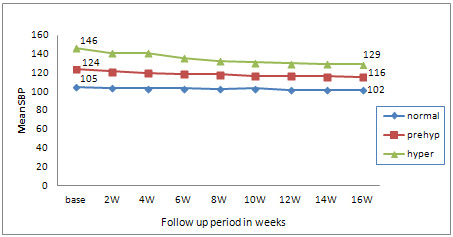
Figure
1
displays
the
mean
SBP
readings
for
the
study
groups,
across
the
follow
up
period
of
the
study.
The
effect
of
DASH
diet
was
most
evident
on
the
hypertensive
group,
where
the
mean
SBP
was
reduced
from
146
mmHg
at
base
line
to
129.6
mmHg
at
the
end
of
16
weeks
and
this
reduction
reached
a
plateau
at
12
weeks.
Figure
1:
Follow
up
of
mean
systolic
blood
pressure,
among
study
groups,
during
the
duration
of
the
study
Regarding
the
diastolic
blood
pressure
(DBP)
readings,
the
base
line
reading
for
the
normotensive
group
was
69.5
±
4.5
mmHg
that
became
at
the
end
of
the
study
68.4
±
3.6
mmHg,
with
mean
change
1.1
±
2.1
mmHg.
Similarly
it
was
80.8
±
2.7
mmHg,
then
75.0
±
4.8
mmHg,
for
pre-hypertension
group
with
mean
change
5.8
±
4.2
mmHg,
and
was
85.6
±
5.5
mmHg
then
78.3
±
6.7
mmHg
with
mean
change
7.4
±
7.1mmHg
for
hypertensive
group.
There
was
no
significant
change
in
normotensive
group
readings
(P
=
0.83),
however,
there
was
a
significant
change
in
pre-hypertension
and
hypertensive
groups
(P
<
0.001).
Comparing
the
mean
change
in
diastolic
blood
pressure,
a
highly
significant
difference
was
detected
(P
<
0.001).
The
hypertensive
group
showed
the
highest
reduction,
followed
by
the
other
two
groups.
The
difference
was
found
between
the
hypertensive
and
pre-hypertension
groups
in
comparison
to
the
normotensive
group
[Table
2].
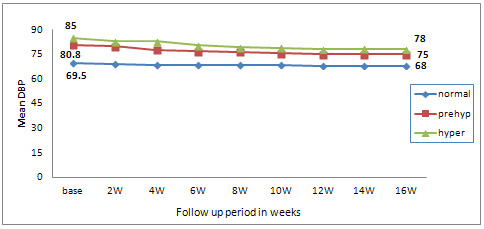
Figure
2
shows
the
mean
DBP
readings
for
the
study
groups
across
the
follow
up
period
of
the
study.
Both
the
hypertensive
and
the
pre-hypertension
groups
started
at
above
80
mmHg
and
reached
78.3
mmHg
and
75.0
mmHg
respectively,
at
the
end
of
the
study
period
with
a
plateau
at
12
weeks.
Figure
2:
Follow
up
of
diastolic
blood
pressure,
among
study
groups
during
the
duration
of
the
study
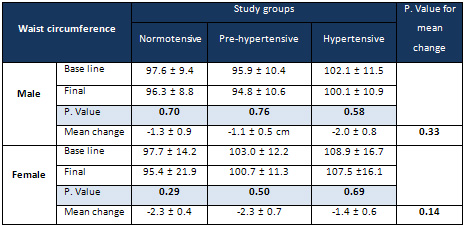
The
mean
waist
circumference
(WC)
among
males
in
the
normotensive
group
at
base
line
was
97.6
±
9.4
cm,
and
then
became
96.3
±
8.8
cm
at
the
end
of
the
study.
Similarly
WC
was
95.9
±
10.4
cm
for
the
pre-hypertension
group,
that
became
94.8
±
10.6
cm,
and
was
102.1
±
11.5
cm,
then
became
100.1
±
10.9
cm
for
the
hypertensive
group
[Table
3].
Although
there
was
a
slight
mean
decrease
in
the
mean
male
WC
of
the
base
line
reading
by
about
1.3
±
0.9
cm,
1.1
±
0.5
cm,
2.0
±
0.8
cm
in
normotensive,
pre-hypertension,
hypertensive
groups
respectively,
there
was
no
statistically
significant
difference
in
the
male
waist
circumference
response.
The
mean
WC
for
females
at
base
line
was
97.7
±
14.2
cm,
to
end
at
95.4
±
21.9
cm
for
the
normotensive
group.
As
for
the
pre-hypertension
group
it
was
103.0
±
12.2
cm,
that
became
100.7
±
11.3
cm,
and
it
was
108.9
±
16.7
cm,
and
became
107.5
±
16.1
cm
for
the
hypertensive
group
[Table
3].
A
slight
decrease
in
the
mean
female
WC
base
line
readings
by
2.3
±
0.4
cm,
2.3
±
0.7
cm
1.4
±
0.6
cm
in
normotensive,
pre-hypertension,
hypertensive
groups
respectively
was
found,
however
these
findings
were
statistically
insignificant.
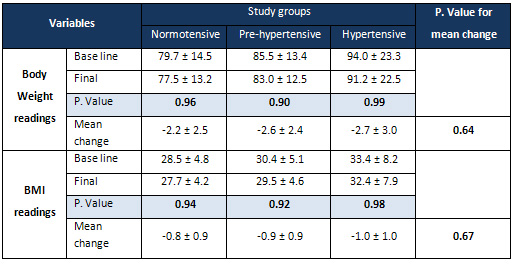
Similar
findings
with
reductions
in
body
weight
and
body
mass
index
were
detected
although
these
were
also
statistically
insignificant
[Table
4].
Table
3:
Effect
of
DASH
diet
on
waist
circumference
of
males
and
females
of
the
study
groups
Table
4:
Effect
of
DASH
diet
on
mean
body
weight
and
body
mass
index
readings
among
the
study
groups
Figure
3:
Follow
up
of
mean
male
waist
circumference,
by
study
groups
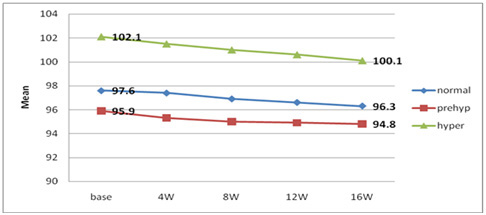
Figure
3
shows
the
mean
male
WC
readings
for
the
study
groups
across
the
follow
up
period
of
the
study.
Both
the
hypertensive
and
the
pre-hypertension
groups
started
at
above
97
cm
and
reached
100.1
and
96.3
cm
respectively,
at
the
end
of
the
study
period.
Although
the
decrease
in
WC
was
insignificant,
it
continued
throughout
the
14
weeks.
Figure
4:
Follow
up
of
female
mean
waist
circumference,
by
study
groups
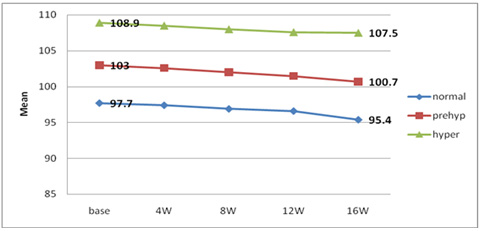
Figure
4
shows
the
mean
female
WC
readings
for
the
study
groups
across
the
follow
up
period
of
the
study.
Both
the
hypertensive
and
the
pre-hypertension
groups
started
at
above
103cm
and
reached
100.7
and
107.5
cm
respectively,
by
the
end
of
the
study
period.
The
decrease
in
WC
was
also
insignificant
but
continued
throughout
the
14
weeks.
The
National
Institutes
of
Health,
in
the
USA,
developed
the
Dietary
Approaches
to
Stop
Hypertension
(DASH)
eating
plan,
which
has
been
shown
to
reduce
blood
pressure
and
body
weight
as
well
as
prevent
chronic
diseases
(12).
This
study
explored
the
effects
of
a
DASH
diet
intervention
among
three
groups
of
Egyptian
patients.
Reductions
in
both
systolic
and
diastolic
blood
pressure
readings
were
found
in
all
groups
of
normotensive,
pre-hypertension
and
hypertensive
grade
1
participants.
However,
reductions
were
significantly
greater
among
the
hypertensive
grade
I
and
pre-hypertensive
group
compared
to
the
normotensive
group.
These
findings
concur
with
results
of
Getchell
et
al,
1999
where
459
adults
who
were
hypertensive
and
non-hypertensive
were
included
and
the
study
applied
three
types
of
diets:
(1)
a
control
diet
with
a
nutrient
composition
typical
of
that
consumed
by
Americans;
(2)
a
DASH
diet
rich
in
fruits,
vegetables,
and
low
fat
dairy
products
with
a
reduced
amount
of
saturated
fat,
total
fat,
and
cholesterol
and
a
modestly
increased
amount
of
protein;
and
(3)
a
diet
rich
in
fruits
and
vegetables
but
otherwise
similar
to
the
control
diet.
It
was
found
that
in
comparison
to
the
control
group,
blood
pressure
reduction
was
greater
in
those
who
were
hypertensive
on
entry
to
the
study.
Additionally,
for
participants
following
the
DASH
diet,
the
amount
of
blood
pressure
reduction
increased
significantly
as
baseline
blood
pressure
increased
(13).
In
addition,
the
study
of
Harnden
et
al,
2010
that
applied
a
DASH
diet
for
30
days
in
the
UK
showed
a
weight
reduction
with
an
associated
significant
reduction
in
the
mean
systolic
and
diastolic
blood
pressure
(14).
As
regards
the
effect
of
DASH
and
time
to
reduction
of
both
systolic
and
diastolic
blood
pressure,
findings
of
our
study
showed
major
significant
reductions
in
the
BP
among
pre-hypertensive
and
hypertensive
group
1
patients
were
greater
in
the
first
8
weeks
reaching
a
plateau
after
12
weeks
till
the
end
of
the
study.
Similar
results
were
reported
by
Craddick
et
al,
2003
who
found
that
DASH
diet
quickly
and
significantly
reduces
blood
pressure,
in
comparison
to
the
control
(ordinary)
diet
among
adults
diagnosed
as
pre-hypertensive
and
hypertensive
grade
1.
These
results
were
obtained
without
requiring
participants
to
lose
weight
or
reduce
their
sodium
intake
(15).
Earlier
Vollmer
et
al,
2001
reported
on
proven
strategies
for
reducing
blood
pressure
as
confirming
the
DASH
diet,
and
reducing
sodium
intake
among
other
strategies.
Adopting
each
alone
or
in
combination
would
reduce
the
risks
of
high
blood
pressure.
However,
this
requires
long-term
commitment
and
significant
lifestyle
change
to
be
effective
(16).
In
2007,
Dauchet
et
al,
found
in
a
cross-sectional
analysis,
that
measured
intake
of
fruits,
vegetables,
and
dairy
products
which
are
the
components
of
DASH
diet,
are
associated
with
a
lowered
systolic
blood
pressure
by
1.5
mmHg
and
diastolic
blood
pressure
by
1.4
mmHg
(17).
In
our
study,
there
was
a
slight
decrease
in
the
mean
WC
in
normotensive,
pre-hypertension,
hypertensive
groups.
Although
this
was
insignificant
yet
it
continued
throughout
the
14
weeks
of
the
study.
Additionally,
slight
reductions
were
also
found
regarding
body
weight
and
BMI
following
compliance
to
the
DASH
diet
that
although
insignificant,
may
have
also
helped
in
reducing
blood
pressure
among
study
participants.
Data
from
the
ENCORE
study
suggest
that
the
DASH
eating
plan
alone
lowers
blood
pressure
in
overweight
individuals
with
high
blood
pressure,
but
significant
improvements
in
insulin
sensitivity
are
observed
only
when
the
DASH
diet
is
implemented
as
part
of
a
more
comprehensive
lifestyle
modification
program
that
includes
exercise
and
weight
loss
(18).
DASH
is
thus
preferred
as
the
initial
approach
to
treating
most
individuals
with
uncomplicated
higher
than
optimal
blood
pressure.
Various
DASH
studies
have
demonstrated
that
the
total
eating
pattern,
including
sodium
and
other
nutrients
and
foods,
affects
blood
pressure
and
is
also
associated
with
a
reduced
risk
of
cardiovascular
disease
and
lowered
mortality
(12,
19).
This
study
provides
evidence
for
the
beneficial
health
outcomes
among
adults
that
have
confirmed
our
intervention.
Results
have
shown
that
DASH
diet
reduces
blood
pressure
among
all
participants
but
with
more
effect
among
those
with
higher
blood
pressure
levels.
DASH
diet
as
a
monotherapy
is
known
to
be
an
effective
and
rapid
initial
treatment
for
patients
with
mild
hypertension.
As
an
intervention,
it
alleviates
the
cost
and
side
effects
associated
with
antihypertensive
medications,
ultimately
improving
a
patient's
quality
of
life.
Therefore,
the
study
recommends
that
family
physicians
begin
with
it
as
a
first
step
for
primary
prevention
or
secondary
prevention
in
mildly
uncomplicated
hypertensive
patients
and
determine
its
efficacy
after
8
-12
weeks.
While
other
lifestyle
modifications
such
as
smoking
cessation
require
greater
time
and
personal
effort,
adherence
to
the
DASH
diet
program
can
be
encouraged
through
health
education,
enhancing
family
support
and
frequent
counseling.
1.
Arafa
NAS,
and
Ez-Elarab
HS
(2011).
Epidemiology
of
Prehypertension
and
Hypertension
among
Egyptian
Adults.
The
Egyptian
Journal
of
Community
Medicine;
29
(1):
1-18
2.
World
health
Organization,
(2012)
Egypt;
Noncommunicable
diseases
risk
factor
survey.
STEPwise
2011
-
2012.
World
Health
Organization
-
Egypt
Country
Office
In
collaboration
with
Ministry
of
Health
and
Population
-
Egypt.
Available
at:
http://www.who.int/chp/steps/2011-2012_Egypt_FactSheet.pdf
3.
Pearce
KA
and
Dassow
P
(2008).
In
Taylor's
manual
of
family
medicine,
3rd
Edition.
9.1
Hypertension.
Lippincott
Williams&
Wilkins.
Pg
284-291.
4.
Appel
LJ
(2010).
DASH
Position
Article:
Dietary
approaches
to
lower
blood
pressure.
On
behalf
of
the
American
Society
of
Hypertension
Writing
Group.
Journal
of
the
American
Society
of
Hypertension;
4
(2):
79-89.
Available
at:
http://dx.doi.org/10.1016/j.jash.2010.03.004
5.
Neal
B,
MacMahon
S,
Chapman
N.
(2000).
Effects
of
ACE
inhibitors,
calcium
antagonists,
and
other
blood-pressure-lowering
drugs:
results
of
prospectively
designed
overviews
of
randomised
trials.
Blood
Pressure
Lowering
Treatment
Trialists'
Collaboration.
Lancet.
;
356:
1955-1964.
6.
Svetkey
L
P.,
Morton
DS.
,
Vollmer
W
M.,
et
al
(1999).
Effects
of
Dietary
Patterns
on
Blood
Pressure
Subgroup
Analysis
of
the
Dietary
Approaches
to
Stop
Hypertension
(DASH)
Randomized
Clinical
Trial,
Arch
Intern
Med.:
159(3):285-293.
7.
Hinderliter
AL,
Babyak
MA,
Sherwood
A
and
Blumenthal
JA
(2011).
The
DASH
Diet
and
Insulin
Sensitivity.
Curr
Hypertension
Rep
13:
67-73.
8.
Ataman
SL,
Cooper
R,
Rotimi
C,
et
al
(1996).
Standardization
of
blood
pressure
measurements
in
an
international
comparative
study.
J
Clin
Epidemiology;
49(8):
869-877.
9.
Sacks
F
M,
Svetkey
L
P,
Vollmer
W
M,
et
al
(2001).
DASH-Sodium
Collaborative
Research
Group.
Effects
on
blood
pressure
of
reduced
dietary
sodium
and
the
Dietary
Approaches
to
Stop
Hypertension
(DASH)
diet.
N
Engl
J
Med.;
344(1):3-10.
10.
Joint
National
Committee
on
the
Prevention,
Detection,
Evaluation,
and
Treatment
of
High
Blood
Pressure
(2003).
The
Seventh
Report
of
the
Joint
National
Committee
on
the
Prevention,
Detection,
Evaluation,
and
Treatment
of
High
Blood
Pressure:
the
JNC
7
report.
JAMA;
289:
2560-72.
11.
World
Medical
Association
(2008):
The
Declaration
of
Helsinki.
Available
at:
http://www.wma.net/en/30publications/10policies/b3/index.html
12.
U.S.
Department
of
Agriculture
and
U.S.
Department
of
Health
and
Human
Services.
Dietary
Guidelines
for
Americans,
2010.
7th
Edition,
Washington,
DC:
U.S.
Government
Printing
Office,
December
2010.
Available
at:
http://www.health.gov/dietaryguidelines/dga2010/dietaryguidelines2010.pdf
13.
Getchell
WS,
Svetkey
LP,
Appel
LJ,
Moore
TJ,
Bray
GA,
Obarzanek
E
(1999).
Summary
of
the
Dietary
Approaches
to
Stop
Hypertension
(DASH)
Randomized
Clinical
Trial
Current
Treatment
Options
in
Cardiovascular
Medicine,
1:
295
-
298.
14.
Harnden
KE,
Frayn
KN
and
Hodson
L
(2010).
Dietary
Approaches
to
Stop
Hypertension
(DASH)
diet:
applicability
and
acceptability
to
a
UK
population
Journal
of
Human
Nutrition
and
Dietetics.
The
British
Dietetic
Association
Ltd.,
23,
pp.
3-10.
15.
Craddick
SR,
Elmer
PJ,
Obarzanek
E,
Vollmer
WM,
Svetkey
LP
and
Swain
MC
(2003).
The
DASH
Diet
and
Blood
Pressure,
Current
Atherosclerosis
Reports,
5:484-491.
16.
Vollmer
WM,
Sacks
FM,
Svetkey
LP
(2001).
New
insights
into
the
effects
on
blood
pressure
of
diets
low
in
salt
and
high
in
fruits
and
vegetables
and
low-fat
dairy
products
Current
Controlled
Trials
in
Cardiovascular
Medicine:
2(2):71-74
17.
Dauchet
L,
Kesse-Guyot
E,
Czernichow
S,
et
al
(2007).
Dietary
patterns
and
blood
pressure
change
over
5-y
follow-up
in
the
SU.VI.MAX
cohort.
Am
J
Clin
Nutr.;
85(6):1650-1656.
18.
Blumenthal
JA,
Babyak
MA,
Sherwood
A,
et
al.
(2010).
Effects
of
the
Dietary
Approaches
to
Stop
Hypertension
diet
alone
and
in
combination
with
exercise
and
caloric
restriction
on
insulin
sensitivity
and
lipids.
Hypertension.;
55:
1199-1205.
19.
Sacks,
FM,
Obarzanek,
E,
Windhauser,
M,
Svetkey,
L,
Vollmer,
W,
McCullough,
M,
Karanja,
N,
Lin,
P-H
et
al.
(1995).
Rationale
and
design
of
the
Dietary
Approaches
to
Stop
Hypertension
trial
(DASH).
Annals
of
Epidemiology;
5
(2):
108-118.
|

