|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................
|
Original
Contribution/Clinical Investigation
|
|
|
<-- Abu Dhabi -->
Knowledge,
attitude and behaviour of asthmatic patients
regarding asthma in primary care setting in
Abu Dhabi, United Arab Emirates
[pdf version]
Osama Moheb Ibrahim Mohamed, Wael Karameh Karameh
<-- Egypt -->
DASH Diet: How
Much Time Does It Take to Reduce Blood Pressure
in Pre-hypertensive and Hypertensive Group 1
Egyptian patients?
[pdf version]
Rehab Abdelhai, Ghada Khafagy, Heba Helmy
<-- Egypt -->
Assessment of TB
stigma among patients attending chest hospital
in Suez Canal University area, Egypt
[pdf version]
Nahed Amen Eldahshan, Rehab Ali Mohammed, Rasha
Farouk Abdellah, Eman Riad Hamed
<-- Egypt -->
Awareness
of diabetic retinopathy in Egyptian diabetic
patients attending Kasra Al-Ainy outpatient
clinic: A cross-sectional study
[pdf version]
Marwa Mostafa Ahmed, Mayssa Ibrahim Ali, Hala
Mohamed El-Mofty, Yara Magdy Taha
<-- Iraq -->
Estimation of
some biophysical parameters in semen of fertile
and infertile patients
[pdf version]
Dhahir Tahir Ahmad, Suhel Mawlood Alnajar, Tara
Nooradden Abdulla, Zhyan Baker Hasan
|
|
........................................................ |
Medicine and Society
|



|
<-- Iraq -->
Celebrating lives
from the Region
[pdf version]
Lesley Pocock
<-- Regional/International -->
Health
Promotion, Disease Prevention and Periodic Health
Checks: Perceptions and Practice among Family
Physicians in Eastern Mediterranean Region
[pdf version]
Waris Qidwai, Kashmira Nanji, Tawfik A M Khoja,
Salman Rawaf, Nabil Yasin Al Kurashi, Faisal
Alnasir, Mohammed Ali Al Shafaee, Mariam Al
Shetti,Nagwa Eid Sobhy Saad, Sanaa Alkaisi,
Wafa Halasa, Huda Al-Duwaisan, Amal Al-Ali
<--
Australia/Iran -->
Virology
vigilance - an update on MERS and viral mutation
and epidemiology for family doctors
[pdf version]
Lesley Pocock, Mohsen
Rezaeian
|
........................................................
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| July / August
2015 - Volume 13 Issue 5 |
|
Assessment
of TB stigma among patients attending chest hospital
in Suez Canal University area, Egypt
Nahed Amen Eldahshan (1)
Rehab Ali Mohamed (1)
Rasha Farouk Abdellah
(2)
Eman Riad Hamed
(3)
(1) Lecturer ofFamily medicine, Faculty of medicine,
Suez Canal University
(2) Lecturer of occupational Health, Faculty
of medicine, Suez Canal University
(3) Lecturer of chest diseases and tuberculosis,
Faculty of medicine, Suez Canal University
Correspondence:
Dr. Nahed
Amen Eldahshan
Lecturer family medicine
Faculty of medicine, Suez Canal University
Ismailia city, Egypt
Mobile: 01222626824
Email:
nahed.eldahshan@yahoo.com
|
Abstract
Background: TB
stigmatization is a complex process involving
institutions, communities, and inter-
and intra-personal attitudes. While it
has been recognized as an important social
determinant of health and health disparities,
the difficulties in identifying, characterizing,
measuring, and tracking changes in stigmatization
over time have made it challenging to
justify devoting resource intensive interventions
to the problem.
Objectives: To
identify the magnitude and the burden
of TB stigma on patient and effect of
TB stigma on treatment adherence.
Methods: The
data were collected between August and
December 2014, recruiting all patients
who had commenced treatment for up to
a month. All patients were subjected to
personal detailed interview according
to a predesigned questionnaire after taking
informed consent of the patients.
Results: A
total of 53 patients consented to participate.
The mean age ± SD was 43 ±
14.1 years. Out of the total number, 22.6%
were illiterate and 77.4% were literate.
As regards occupation, 69.8% were independent
and 30.2% were dependent. The stigma prevalence
among TB patients was found to be 41.5%.
Stigma is more prevalent among the younger
age group (43.5 %), males (43.9 %) and
among married patients (46.7%). There
was an immense stigma observed among urban
residence (57.7 %), current smokers (60.0
%) and those who had two or less rooms
in their house (66.7 %) and this was found
to have a statistically significant difference
(P<0.05). The majority of patients
(67.9%) take treatment regularly.
Conclusion: TB
stigma has been raised as a potential
barrier to home and work-based direct
observational therapy (DOT). Perceived
TB stigma had no effect on treatment regularity.
Health education programs should be conducted
to reduce TB stigma and improve patients'
compliance.
Key words : TB
stigma, prevalence , treatment adherence
|
Tuberculosis (TB) is believed to be nearly
as old as human history. Traces of it in Egyptian
mummies date back to about 7000 years ago, when
it was described as phthisis by Hippocrates(1).
It was declared a public health emergency in
the African Region in 2005 and has since continued
to be a major cause of disability and death(2).
About 9.4 million new cases of tuberculosis
were diagnosed in 2009 alone and 1.7 million
people reportedly died from the disease in the
same year, translating to about 4700 deaths
per day (2). About one-third of the world's
population (estimated to be about 1.75 billion)
is infected with the tubercle bacillus(3). As
much as 75% of individuals with TB are within
the economically productive age group of 15
to 54 years. This significantly impairs socioeconomic
development, thereby perpetuating the poverty
cycle (4).
The social determinants of health refer to
the institutional, community, and interpersonal
factors that affect health outside of the ease
with which an individual can access medical
services (5). Stigma, which is shaped and promulgated
by institutional and community norms and interpersonal
attitudes, is a social determinant of health(6).
Stigma is a process that begins when a particular
trait or characteristic of an individual or
group is identified as being undesirable or
disvalued(7). The stigmatized individual often
internalizes this sense of disvalue and adopts
a set of self-regarding attitudes about the
marked characteristic including shame, disgust,
and guilt (8). These attitudes produce a set
of behaviors that include hiding the stigmatized
trait, withdrawing from interpersonal relationships,
or increasing risky behavior (9-10).
Stigmatization is conceptually distinct from
discrimination, another social determinant of
health in that the primary goal of discrimination
is exclusion, not necessarily for the target
to feel ashamed or guilty(11-12). Stigmatized
individuals can, however, suffer discrimination
and status loss at the hands of the broader
community, whose norms have caused them to be
perceived as undesirable (7-13). Stigmatization
is a complex process involving institutions,
communities, inter- and intra-personal attitudes.
While it has been recognized as an important
social determinant of health and health disparities,
the difficulties in identifying, characterizing,
measuring, and tracking changes in stigmatization
over time have made it challenging to justify
devoting resource intensive interventions to
the problem(6-14). One exception is human immunodeficiency
virus (HIV)/acquired immunodeficiency syndrome
(AIDS) research, where the interactions among
stigma, HIV risk behaviors, and HIV associated
outcomes have been fairly well characterized(15-16).
Substantially less study has been conducted
on the mechanisms through which stigma impacts
the health of individuals at risk for or infected
with TB. From its introduction in 1994, DOTS
has been the backbone of TB control around the
world. With its focus on passive case detection,
availability of diagnostic techniques, and directly
observed therapy to minimize drug resistant
TB, DOTS has been criticized as a treatment
guideline and biomedical strategy that does
not account for social factors related to TB
control rather than a comprehensive control
plan (17-18).
Delay in presentation to a health facility
is an important concern as it contributes to
delays in initiating TB treatment. This can
result in greater morbidity and mortality for
the patient and increased transmission of Mycobacterium
tuberculosis in the community(19-20). There
is a large body of literature on factors associated
with delay in seeking care for TB symptoms.
These can be broadly grouped into access to
care, personal characteristics, socioeconomic,
clinical, TB knowledge or beliefs, and social
support or psychosocial factors(21). One psychosocial
factor of interest is health-related stigma,
often defined as a social process "characterized
by exclusion, rejection, blame, or devaluation
resulting from experience or reasonable anticipation
of an adverse social judgment" because
of a particular health condition (22). Some
studies have suggested that TB stigma could
lead to delays in patients seeking appropriate
medical care (19-23).
To
highlight
the
importance
of
psychosocial
factor
on
TB
stigma,
aiming
to
improve
the
quality
of
care
for
TB
patients.
To
identify
the
magnitude
and
the
burden
of
TB
stigma
on
patients
received
TB
treatment
and
to
determine
socio
demographics
factors
associated
with
TB
stigma.
This
was
a
cross
sectional
study
conducted
at
two
government
health
institutions
providing
TB
services
in
the
Suez
Canal
area.
The
treatment
regimens
used
throughout
the
country
are
based
on
the
World
Health
Organization's
(WHO)
Directly
Observed
Treatment,
ShortCourse
(DOTS)
strategy.
The
data
were
collected
between
August
and
December
2014,
recruiting
allpatients
who
had
commenced
treatment
for
up
to
a
month.
All
patients
were
subjected
to
personal
detailed
interview
according
to
a
predesigned
questionnaire
after
taking
informed
consent
of
the
patients.
Before
conducting
the
study,
the
questionnaire
was
pre-tested
and
evaluated
for
proper
conduct
of
the
study.
The
information
was
elicited
from
TB
patients
regarding
'problems
faced
in
their
homes,
neighbours'
attitudes
and
friends.
Questionnaire
included
questions
regarding
data
on
socioeconomic
issues
and
awareness
of
TB
and
the
nature
of
their
disclosure
of
their
disease
to
family
members.
The
information
was
also
elicited
regarding
behavioral
changes
such
as
maintaining
appropriate
personal
distance
and
avoiding
close
contact
in
activities
with
family
members,
neighbours,
friends
and
other
fellow
employees.
The
data
were
entered,
cleaned
and
analyzed
using
SPSS
software
version
18.0.
Descriptive
statistics
like
frequency
distribution
and
percentage
calculation
was
made
for
most
of
the
variables.
Chi
square
test
and
proportion
tests
were
used
to
assess
significance.
A
value
of
p<0.05
was
taken
as
significant.
Ethical
Considerations
The
study
subjects
were
explained
the
purpose
of
study
and
assured
privacy.
Confidentiality
and
anonymity
were
maintained
according
to
the
regulations
mandated
by
Research
Ethics
Committee
of
Faculty
of
Medicine
Suez
Canal
University
(no.2357).
Table
1:
Distribution
of
the
study
group
according
to
Socio-demographic
characteristics
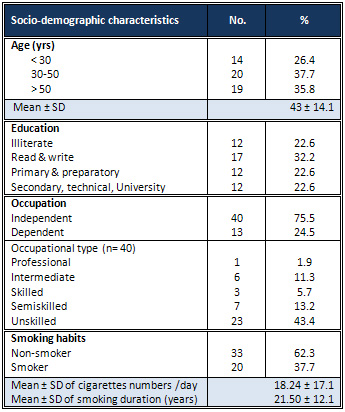
A
total
of
53
patients
consented
to
participate.
The
socio-demographic
profile
of
TB
patients
is
presented
in
Table
1.
The
mean
age
±
SD
was
43
±
14.1
years.
Out
of
the
total
number,
22.6%
were
illiterate
and
77.4%
were
literate.
As
regards
occupation,
69.8%
were
independent
and
30.2%
were
dependent.
There
were
more
male
cases
(77.4
%)
than
female
(22.6%).
Approximately
half
of
the
cases
were
married
(56.6
%)
and
the
majority
had
appropriate
family
income
(64.2%).
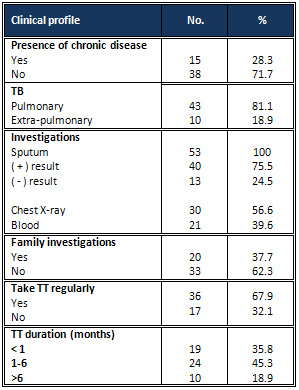
Table
2:
Clinical
profile
of
the
study
population
Table
3:
Prevalence
of
TB
stigma
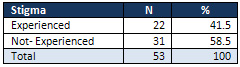
Table
4:
Association
of
risk
factors
and
TB
stigma
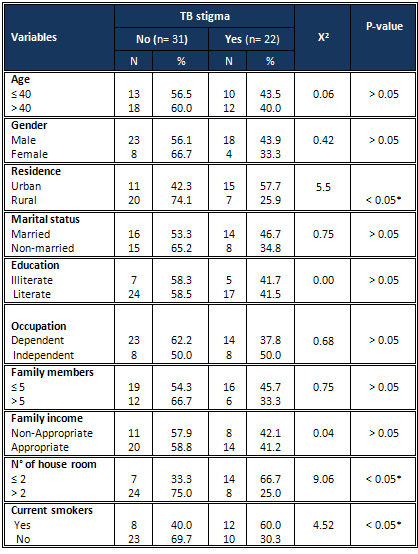
As
regards
clinical
profile
of
the
study
population,
81.1%
had
pulmonary
TB
and
75.5%
had
positive
sputum
smear.
The
majority
of
patients
(67.9
%)
take
treatment
regularly
as
presented
in
Table
2.
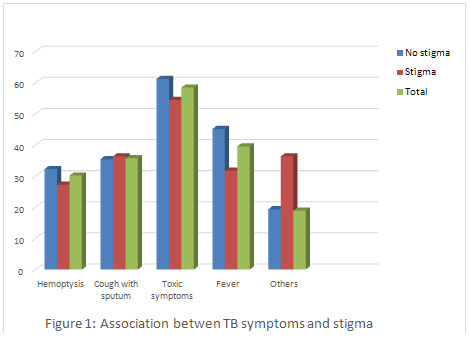
Toxic
symptoms
were
the
most
prevalent
among
TB
patients
(58.5
%)
followed
by
fever
(39.6
%)
and
cough
with
sputum
(35.8
%)
(Figure
1).
The
stigma
prevalence
among
TB
patients
was
found
to
be
41.5%
(Table
3).
Stigma
is
more
prevalent
among
younger
age
groups
(43.5%),
males
43.9%
and
among
married
patients
(46.7%).
There
was
an
immense
stigma
observed
among
urban
residence
(57.7%),
current
smokers
(60.0
%)
and
those
who
had
two
or
less
rooms
in
their
house
(66.7%)
and
this
was
found
to
be
a
statistically
significant
difference
(P<0.05)(
Table
4).
Table
5:
Distribution
of
stigma
score
of
TB
patients
according
to
community
perspectives
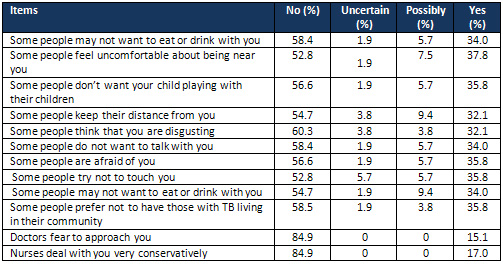
Stigma
faced
in
community
by
TB
patients:
About
one
third
of
TB
patients
reported
that
some
people
prefer
not
to
have
those
with
TB
living
in
their
community
and
35.8%
reported
that
some
people
don't
want
their
children
to
play
with
a
TB
patient's
child
(Table
5).
Table
6:
Distribution
of
stigma
score
of
TB
patients
according
to
patient
perspectives
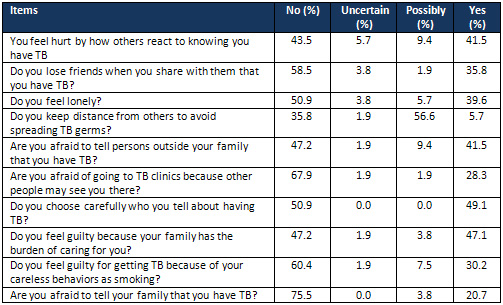
Perceived
Stigma
among
TB
patients:
Out
of
a
total
of
53
patients
41.5%
reported
feeling
hurt
by
how
others
react
to
knowing
that
they
have
TB
and
35.8%
lose
friends
when
they
share
with
them
that
they
have
TB.
Being
afraid
of
going
to
TB
clinics
because
other
people
may
see
them
was
reported
by
28.3%
of
TB
patients.
While
about
half
of
the
patients,
47.1%,
felt
guilty
because
their
family
has
the
burden
of
caring
for
them(Table
6).
Globally,
14.6
million
people
have
active
TB
disease.
Each
year
8.9
million
people
develop
active
TB(24).
Patients
often
isolate
themselves
to
avoid
infecting
others
and
to
avoid
uncomfortable
situations
such
as
being
shunned
or
becoming
the
subject
of
gossip
(25).
Hence,
the
aim
of
this
study
was
to
improve
the
quality
of
life
of
TB
patients
by
identifying
the
magnitude
and
the
burden
of
TB
stigma
on
patients.
Results
of
the
current
study
indicated
that
the
majority
of
the
study
sample
were
men
(77.4
%);
the
same
results
were
supported
by
Aryal(26).
Approximately
half
of
the
cases
were
married
(56.6
%)
and
the
majority
were
literate
and
this
is
in
agreement
with
Abioye
et
al.
(27).
However
this
was
not
supported
in
a
study
in
Bangladesh
where
the
majority
of
patients
had
not
received
any
formal
education
and
this
is
due
to
the
difference
in
culture
and
socioeconomic
characteristics(28).
Our
study
shows
also
that
the
majority
had
appropriate
family
income
(64.2%)
which
matches
the
urban
community
where
the
study
took
place.
Results
showed
that
41.5%
of
the
TB
patients
had
experienced
stigma;
similar
results
were
found
in
Nepal
(63.3%)(26).
The
same
prevalence
was
found
in
a
study
conducted
in
southern
Thailand
by
Rie
AV,
which
shows
that
stigma
is
present
in
patients'
perspective
towards
TB
(29).
Several
studies
suggest
that
health-care
providers
and
at-risk
community
members
perceive
TB
stigma
to
have
a
more
substantial
impact
on
women's
health-care-seeking
behavior
than
on
men's(30).
However
this
disagrees
with
the
study
results
in
which
stigma
was
slightly
more
prevalent
among
men.
This
is
because
most
women
in
our
community
do
not
work
and
do
not
come
in
direct
contact
with
community
members
such
as
men.
In
another
study
work-related
aspects
of
stigma
were
frequently
re-ported,
and
they
were
more
likely
to
be
an
issue
for
men
(28).
In
urban
areas,
there
may
be
more
fears
of
being
discriminated
in
the
work
environment,
or
of
losing
jobs.
This
explains
the
study
results
that
show
that
immense
stigma
observed
among
urban
residence.
Abioye
et
al,
2011
found
that
patients
presenting
with
previous
smoking
history
were
more
likely
to
experience
stigma
in
a
study
in
Lagos,
Nigeria
(27)
and
this
also
can
be
found
in
this
study,
where
there
is
a
statistically
significant
relation
between
stigma
and
smoking.
Abioye
et
al.(2011),
studied
stigma
among
patients
with
pulmonary
tuberculosis
in
Lagos,
Nigeria.
They
found
that
limited
education
and
patients
who
are
in
the
working
age
groups
(20
to
50
years)
had
TB
stigma.
However
according
to
the
current
study
results,
no
statistically
significant
association
could
be
revealed
between
these
two
sociodemographic
determinants.
TB
stigma
has
been
raised
as
a
potential
barrier
to
home-
and
work-based
direct
observational
therapy
(DOT)
(31).
Perceived
TB
stigma
was
also
associated
with
noncompliance
among
Pakistani
patients
on
DOT
(32).
However,
this
study
shows
an
insignificant
relation
between
TB
stigma
and
regularity
of
TB
treatment
and
this
may
have
contributed
to
the
effect
of
TB-related
stigma
and
social
discrimination
on
the
patients
that
forces
them
to
be
compliant
to
drugs
so
that
they
can
avoid
the
stigmatization.
Although
several
survey
instruments
are
in
development
for
measuring
perceived
and
internalized
TB
stigma,
most
research
uses
qualitative
techniques
for
assessing
TB
stigma.
The
use
of
different
measurement
tools
may
explain
why
TB
stigma
is
a
predictor
of
diagnostic
delay
and
treatment
nonadherence
in
some
studies
and
not
in
others(33).
In
this
study
Toxic
symptoms
were
the
most
prevalent
among
TB
patients
(58.5
%)
followed
by
fever
(39.6
%)
and
cough
with
sputum
(35.8
%),
but
the
relation
between
TB
symptoms
and
stigma
were
not
statistically
significant
as
most
stigmatized
TB
patients
usually
do
not
disclose
their
symptoms
as
this
increases
the
state
of
discrimination
in
their
life;
they
want
to
hide
their
symptoms
from
others.
Some
of
the
patients
also
revealed
that
they
go
to
the
DOTS
center
which
is
farther
from
their
home
so
that
nobody
knows
that
they
are
taking
TB
drugs
(26).
In
this
study
35.8%
lose
friends
when
they
share
with
them
that
they
have
TB.
This
is
in
agreement
with
another
study
conducted
in
southern
India
that
showed
that
many
men
felt
inhibited
from
revealing
the
diagnosis
to
friends
(43%)
and
even
to
their
spouse
(16%)
(34).
The
study
results
shows
that
41.5%
reported
feeling
hurt
by
how
others
react
to
knowing
that
they
have
TB
and
35.8%
lose
friends
when
they
share
with
them
that
they
have
TB.
This
was
revealed
in
another
study
in
India
where
most
of
the
patients
said
that
they
have
impaired
self-esteem,
felt
shamed
or
embarrassed,
and
have
felt
less
respect
from
others
in
the
society
(34).
Another
study
conducted
revealed
that
TB
patients
perceive
their
neighbors
and
friends
attitudes
towards
them
as
rather
negative
(35)which
was
in
agreement
with
this
study.
TB
stigma
has
been
raised
as
a
potential
barrier
to
home-
and
work-based
direct
observational
therapy
(DOT)
(31).
Health
education
programs
should
be
conducted
to
reduce
TB
stigma
and
improve
patients'
compliance.
Acknowledgment:To
all
patients
who
agreed
to
participate
in
the
study
and
to
all
members
of
chest
hospitals
in
Suez
Canal
area
for
their
cooperation
and
help.
1.
Facts
about
health
in
African
Subregion,
Fact
sheet
N314
World
Health
Organisation,
2011.
2.
2010/2011tuberculosis
global
fact;
World
Health
Organisation,
http://www.who.int/tb/country/en/index.html,
Nov.
2010.
3.
Global
tuberculosis
control:
a
short
update
to
the
2009
report,
Tech.
Rep.,
World
Health
Organization,
Geneva,
Switzerland,
(WHO/HTM/TB/2009.426),
2009.
4.
Global
tuberculosis
control
2010,
Tech.
Rep.,
World
Health
Organization,
Geneva,
Switzerland,
(WHO/HTM/TB/2010.),
2010.
5.
World
Health
Organization,
Commission
on
Social
Determinants
of
Health.
Closing
the
gap
in
a
generation:
health
equity
through
action
on
the
social
determinants
of
health.
Final
report
of
the
Commission
on
Social
Determinants
of
Health.
Geneva:
WHO;2008.
6.
Heijnders
M,
Van
Der
Meij
S.
The
fight
against
stigma:
an
overview
of
stigma-reduction
strategies
and
interventions.
Psychol
HealthMed
2006;11:353-63.
7.
Link
B,
Phelan
J.
Conceptualizing
stigma.
Annu
Rev
Sociol
2001;27:363-85.
8.
Goffman
E.
Stigma:
notes
on
the
management
of
spoiled
identity.
Garden
City
(NY):
Anchor
Books;
1963.
9.
Smith
R,
Rossetto
K,
Peterson
BL.
A
meta-analysis
of
disclosure
of
one's
HIV-positive
status,
stigma
and
social
support.
AIDS
Care2008;20:1266-75.
10.
Collins
PY,
von
Unger
H,
Armbrister
A.
Church
ladies,
good
girls,
and
locas:
stigma
and
the
intersection
of
gender,
ethnicity,
mental
illness,
and
sexuality
in
relation
to
HIV
risk.
SocSci
Med
2008;67:389-97.
11.
Deacon
H.
Towards
a
sustainable
theory
of
health-related
stigma:
lessons
from
the
HIV/AIDS
literature.
J
Community
ApplSocPsychol
2006;16:418-25.
12.
Courtwright
AM.
Justice,
stigma,
and
the
new
epidemiology
of
health
disparities.
Bioethics
2009;23:90-6.
13.
Major
B,
O'Brien
LT.
The
social
psychology
of
stigma.
Annu
Rev
Psychol
2005;56:393-421.
14.
Parker
R,
Aggleton
P.
HIV
and
AIDS-related
stigma
and
discrimination:
a
conceptual
framework
and
implications
for
action.
SocSci
Med
2003;57:13-2
15.
Whalen
CC.
Failure
of
directly
observed
treatment
for
tuberculosis
in
Africa:
a
call
for
new
approaches.
Clin
Infect
Dis.
2006
Apr
1;42(7):1048-1050.
[PubMed]
16.
Lienhardt
C,
Ogden
JA.
Tuberculosis
control
in
resource-poor
countries:
have
we
reached
the
limits
of
the
universal
paradigm?
Trop
Med
Int
Health.
2004
Jul;9(7):833-841.
[PubMed]
17.
Barker
RD,
Millard
FJ,
Malatsi
J,
et
al.
Traditional
healers,
treatment
delay,
performance
status
and
death
from
TB
in
rural
South
Africa.
Int
J
Tuberc
Lung
Dis.
2006
Jun;10(6):670-675.
[PubMed]
18.
Golub
JE,
Bur
S,
Cronin
WA,
et
al.
Delayed
tuberculosis
diagnosis
and
tuberculosis
transmission.
Int
J
Tuberc
Lung
Dis.
2006
Jan;10(1):24-30.
[PubMed]
19.
Lin
X,
Chongsuvivatwong
V,
Lin
L,
Geater
A,
Lijuan
R.
Dose-response
relationship
between
treatment
delay
of
smear-positive
tuberculosis
patients
and
intra-household
transmission:
a
cross-sectional
study.
Trans
R
Soc
Trop
Med
Hyg.
2008
Aug;102(8):797-804.
[PubMed]
20.
Madebo
T,
Lindtjorn
B.
Delay
in
Treatment
of
Pulmonary
Tuberculosis:
An
Analysis
of
Symptom
Duration
Among
Ethiopian
Patients.
MedGenMed.
1999
Jun
18;E6.
[PubMed]
21.
Storla
DG,
Yimer
S,
Bjune
GA.
A
systematic
review
of
delay
in
the
diagnosis
and
treatment
of
tuberculosis.
BMC
Public
Health.
2008
Jan
14;8(1):15.
[PMC
free
article]
[PubMed]
22.
Weiss
MG,
Ramakrishna
J.
Stigma
interventions
and
research
for
international
health.
Lancet.
2006
Feb
11;367(9509):536-538.
[PubMed]
23.
Baral
SC,
Karki
DK,
Newell
JN.
Causes
of
stigma
and
discrimination
associated
with
tuberculosis
in
Nepal:
a
qualitative
study.
BMC
Public
Health.
2007;7:211.
[PMC
free
article]
[PubMed]
24-
World
Health
Organisation:
Global
Tuberculosis
Control:
surveillance,
planning,
financing.
WHO
report
2006.
Geneva:
World
Health
Organisation;
2006.
25-
Sushil
C
Baral,
Deepak
K
Karki
and
James
N
Newell.
Causes
of
stigma
and
discrimination
associated
with
tuberculosis
in
Nepal:
a
qualitative
study.
BMC
Public
Health
2007,
7:211.
This
article
is
available
from:http://www.biomedcentral.com/1471-2458/7/211.
26-
Aryal
S,
Badhu
A,
Pandey
S,
Bhandari
A,
Khatiwoda
P,
Khatiwada
P,
et
al.
Stigma
related
to
Tuberculosis
among
patients
attending
DOTS
clinics
of
Dharan
Municipality.
Kathmandu
Univ
Med
J
2012;37(1)48-52.
27-
Abioye
IA,
Omotayo
MO,
Alakija
W.
Socio-demographic
determinants
of
stigma
among
patients
with
pulmonary
tuberculosis
in
Lagos,
Nigeria
African
Health
Sciences
Vol
11
Special
Issue
1
August
2011.
28-
D.
Somma,
B.
E.
Thomas,
F.
Karim,
J.
Kemp,
N.
Arias,
C.
Auer,
G.
D.
Gosoniu,
A.
Abouihia,
M.
G.
Weiss.
Gender
and
socio-cultural
determinants
of
TB-related
stigma
in
Bangladesh,
India,
Malawi
and
Colombia.
INT
J
TUBERC
LUNG
DIS
12(7):856-866
2008.
29-
Rie
AV,
Sengupta
S,
Pungrassami
P,
Balthip
Q,
Choonuan
S,
Kasetjaroen
Y,
et
al.
Measuring
stigma
associated
with
tuberculosis
and
HIV?AIDS
in
southern
Thailand:
exploratory
and
confirmatory
factor
analyses
of
two
new
scales.
Tropical
Medicine
and
International
Health
2008;13(1):21-30.
30-
Thorson
A,
Johansson
E.
Equality
or
equity
in
health
care
access:
a
qualitative
study
of
doctors'
explanations
to
a
longer
doctor's
delay
among
female
TB
patients
in
Vietnam.
Health
Policy.
2004
Apr;68(1):37-46.
31-
Ngamvithayapong
J,
Yanai
H,
Winkvist
A,
Saisorn
S,
Diwan
V.
Feasibility
of
home-based
and
health
centre-based
DOT:
perspectives
of
TB
care
providers
and
clients
in
an
HIV-endemic
area
of
Thailand.
Int
J
Tuberc
Lung
Dis.
2001
Aug;5(8):741-5.
32-
Meulemans
H,
Mortelmans
D,
Liefooghe
R,
Mertens
P,
Zaidi
SA,
Solangi
MF,
et
al.
The
limits
to
patient
compliance
with
directly
observed
therapy
for
tuberculosis:
a
socio-medical
study
in
Pakistan.
Int
J
Health
PlannManag
2002;
17:249-67.
33-
Andrew
Courtwright,
and
Abigail
Norris
Turner.
Tuberculosis
and
Stigmatization:
Pathways
and
Interventions.
Public
Health
Rep.
2010;
125(Suppl
4):
34-42.
34-
Rajeswari
R,
Muniyandi
M,
Balasubramanian
B,
Narayanan
PR.
Perceptions
of
tuberculosis
patients
about
their
physical,
mental
and
social
well-being:
a
field
report
from
south
India.
Social
Science
&
Medicine
2005;
60:1845-53.
35-
Liefooghe
R,
Michiels
N,
Habib
S,
Moran
MB,
Muynck
DA.
Perception
and
social
consequences
of
tuberculosis:
a
focus
group
study
of
tuberculosis
patients
in
Sialkot,
Pakistan.
Social
Science
and
Medicine
1995;41(12):1085-92.
|
|
.................................................................................................................

|
| |
|

