|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
|
........................................................
|
Original
Contribution/Clinical Investigation
|
|
|
<-- Abu Dhabi -->
Knowledge,
attitude and behaviour of asthmatic patients
regarding asthma in primary care setting in
Abu Dhabi, United Arab Emirates
[pdf version]
Osama Moheb Ibrahim Mohamed, Wael Karameh Karameh
<-- Egypt -->
DASH Diet: How
Much Time Does It Take to Reduce Blood Pressure
in Pre-hypertensive and Hypertensive Group 1
Egyptian patients?
[pdf version]
Rehab Abdelhai, Ghada Khafagy, Heba Helmy
<-- Egypt -->
Assessment of TB
stigma among patients attending chest hospital
in Suez Canal University area, Egypt
[pdf version]
Nahed Amen Eldahshan, Rehab Ali Mohammed, Rasha
Farouk Abdellah, Eman Riad Hamed
<-- Egypt -->
Awareness
of diabetic retinopathy in Egyptian diabetic
patients attending Kasra Al-Ainy outpatient
clinic: A cross-sectional study
[pdf version]
Marwa Mostafa Ahmed, Mayssa Ibrahim Ali, Hala
Mohamed El-Mofty, Yara Magdy Taha
<-- Iraq -->
Estimation of
some biophysical parameters in semen of fertile
and infertile patients
[pdf version]
Dhahir Tahir Ahmad, Suhel Mawlood Alnajar, Tara
Nooradden Abdulla, Zhyan Baker Hasan
|
|
........................................................ |
Medicine and Society
|



|
<-- Iraq -->
Celebrating lives
from the Region
[pdf version]
Lesley Pocock
<-- Regional/International -->
Health
Promotion, Disease Prevention and Periodic Health
Checks: Perceptions and Practice among Family
Physicians in Eastern Mediterranean Region
[pdf version]
Waris Qidwai, Kashmira Nanji, Tawfik A M Khoja,
Salman Rawaf, Nabil Yasin Al Kurashi, Faisal
Alnasir, Mohammed Ali Al Shafaee, Mariam Al
Shetti,Nagwa Eid Sobhy Saad, Sanaa Alkaisi,
Wafa Halasa, Huda Al-Duwaisan, Amal Al-Ali
<--
Australia/Iran -->
Virology
vigilance - an update on MERS and viral mutation
and epidemiology for family doctors
[pdf version]
Lesley Pocock, Mohsen
Rezaeian
|
........................................................
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| July / August
2015 - Volume 13 Issue 5 |
|
Awareness
of diabetic retinopathy in Egyptian diabetic patients
attending Kasr Al-Ainy outpatient clinic: A cross-sectional
study
Marwa
Mostafa Ahmed (1)
Mayssa Ibrahim Ali (2)
Hala Mohamed El-Mofty (3)
Yara Magdy Taha (4)
( 1) Marwa Mostafa Ahmed
Lecturer of family medicine
Family Medicine Department, Cairo University,
Egypt
(2) Mayssa Ibrahim Ali
Professor of internal medicine
Internal Medicine Department, Cairo University,
Cairo, Egypt
(3) Hala Mohamed El-Mofty
Professor of Ophthalmology
Ophthalmology Department, Cairo University,
Cairo, Egypt
(4) Yara Magdy Taha
Assistant lecturer of family medicine
Family Medicine Department, Cairo University,
Egypt
Correspondence:
Marwa Mostafa Ahmed,
Lecturer of Family Medicine
Department of Family Medicine, Faculty of Medicine,
Cairo University
Cairo, Egypt
Mobile Number: 002 0100 5681817
Email: marwamostafa@kasralainy.edu.eg
|
Abstract
Background: Diabetic
retinopathy (DR) is a sight-threatening
microvascular complication of diabetes.
Objectives: The
objectives of this study were to assess
the awareness of diabetic patients about
the screening for diabetic retinopathy
and to detect the presence of different
stages of retinopathy among a sample of
patients attending the Diabetic clinic
in Kasr Al-Ainy hospital.
Methods: This
study is a cross sectional study in which
100 adult diabetic patients were interviewed
and visual acuity, retinopathy status,
and presence of other ocular diseases
were assessed.
Results: It
was found that there is general awareness
of diabetic retinopathy among the majority
of the study participants; however there
is little awareness as regards the importance
of screening. The main barrier for performing
fundus examination was lack of awareness
of its importance. Around half of the
participants had performed one fundus
examination after diagnosis of diabetes.
Ophthalmic examination revealed that 47%
of the study participants had no DR at
the time of the examination, 22% had non-proliferative
retinopathy and 31% had proliferative
retinopathy. Only 16% of the participants
had diabetic maculopathy.
Conclusion:
Awareness creation is crucial for decreasing
diabetic eye complications.
Key words:
Egypt, diabetic retinopathy, awareness,
fundus examination, screening.
|
Diabetes is a complex, chronic illness requiring
continuous medical care with multifactorial
risk-reduction strategies beyond glycemic control
(1). The International Diabetes Federation (IDF)
in 2013 estimated that there were 382 million
diabetic patients worldwide; 80% of them lived
in low- and middle-income countries and the
number will increase to be 592 million by the
year 2035. The Diabetic population in Egypt
was estimated to be 7.5 million in 2013 and
it is projected to reach 13.1 million by the
year 2035 (2).
Diabetic retinopathy (DR) and diabetic macular
edema (DME) are common microvascular complications
of diabetes and may have a debilitating impact
on visual acuity, eventually leading to blindness.
Other eye disorders including glaucoma and cataracts
occur earlier and more frequently in people
with diabetes. The current management strategy
for DR/DME requires early detection and optimal
glycemic control to slow the progression of
disease (3).
An initial dilated and comprehensive eye examination
should be performed shortly after the diagnosis
for all type 2 diabetic patients. Subsequent
examinations for type 1 and type 2 diabetic
patients should be repeated annually in the
absence of retinal changes, otherwise shorter
intervals are recommended (4).
Having a high prevalence of diabetes and its
complications in Egypt, there is a strong need
to assess the awareness of consequences or the
end organ damage due to diabetes mellitus among
diabetics. In addition, there is a great need
to estimate the likelihood of diabetics to seek
medical advice for the assessment of the consequences
of diabetes, like diabetic retinopathy. Therefore,
in our study, we have made an attempt to assess
the awareness of diabetic retinopathy and detect
the retinopathy changes among a sample of diabetic
patients.
This
cross-section
observational
study
was
conducted
in
the
Diabetic
Clinic
in
Kasr
Al-Ainy
hospital
from
February
2011
till
February
2012.
Sample
selection:
Purposive
non-probability
sampling
technique
was
used
in
which
100
diabetic
patients
attending
the
Diabetic
Clinic
in
Kasr
Al-Ainy
hospital
were
included
in
the
study.
All
adult
patients
with
type
2
diabetes
who
agreed
to
participate
were
enrolled
in
the
study.
Any
patient
with
other
ophthalmic
diseases
obscuring
retinal
view
or
affecting
the
quality
of
digital
photography
was
excluded
from
the
study.
Study
tool
A
structured
questionnaire
was
designed
to
assess
patient
awareness
regarding
the
importance
of
screening
for
DR,
its
frequency
and
causes
of
non-adherence.
The
content
validation
of
the
questionnaire
was
done
by
two
experts.
The
questionnaire
was
tested
on
10
diabetic
patients
in
order
to
check
the
clarity
of
the
structured
questionnaire
and
to
estimate
the
time
needed
to
complete
the
questionnaire.
It
was
found
that
most
of
the
patients
were
illiterate,
so
the
questionnaire
could
not
be
self-administered
and
was
completed
by
interviewing.
Data
collection
The
first
step:
Following
consent,
participants
completed
an
interview,
that
included:
•
Demographic
characteristics
including:
Age,
gender,
marital
status,
number
of
children,
level
of
education,
employment
status,
insurance
and
its
type.
•
Medical
data
including:
Smoking
status,
previous
eye
diseases
and
operations,
age
of
onset
of
diabetes,
its
duration
and
treatment.
•
Self-perception
regarding
diabetes
control.
•
Chronic
diseases
and
drug
intake
including
aspirin
and
vitamin
B
complex.
•
Family
history
of
diabetes.
•
Previous
fundus
examination
including:
Frequency,
time
of
first
and
last
fundus
examination
and
causes
of
non-adherence
to
previous
fundus
examination.
•
The
awareness
of
the
patients
including:
awareness
about
diabetic
complications,
awareness
about
the
importance
of
screening
of
DR,
available
treatment
options
for
DR
and
the
source
of
their
knowledge.
The
second
step:
Complete
ophthalmological
examination
was
done
including:
•
Visual
acuity
measurement:
using
WHO
classifications
for
grading
of
VA,
which
classified
to,
in
the
best
eye
(WHO,
1992):
-
Blindness:
<
3/60.
-
Severe
visual
impairment:
<6/60
-
3/60.
-
Visual
impairment:
<6/18
-
6/60.
-
Normal:
6/6
-
6/18.
•
Anterior
segment
examination
by
slit-lamp
and
measurement
of
the
intra-ocular
pressure
using
applanation
tonometry.
•
Fundus
examination
using
indirect-ophthalmoscope
was
done
to
reveal
peripheral
abnormalities.
A
fundus
camera
(Topcon,
USA)
was
used
to
take
colored
fundus
photographs
and
fluorescein
angiography.
Photographs
were
evaluated
for
the
presence
of
non-proliferative
DR,
proliferative
DR,
clinically
significant
macular
edema
and
previous
retinal
laser
treatment.
Overall
retinopathy
and
maculopathy
levels
were
assessed
based
on
the
International
Clinical
Diabetic
Retinopathy
and
Diabetic
Macula
Edema
Disease
Severity
Scale
(6).
The
third
step:
Blood
glucose
measurement
was
done
either
by
fasting
blood
sugar,
2
hour
post
prandial
or
HBA1c
to
assess
the
state
of
diabetes
control.
Statistical
analysis
The
data
were
coded
and
entered
using
the
statistical
package
for
social
science
(SPSS)
version
15.
The
data
were
summarized
using
descriptive
statistics:
mean,
standard
deviation,
minimum
and
maximum
values
for
quantitative
variables,
number
and
percentage
for
qualitative
variables.
Statistical
difference
between
groups
was
tested
using:
Chi
square
test,
independent
sample
test
and
ANOVA
test
while
non-parametric
tests
were
used
for
quantitative
variables
which
were
not
normally
distributed.
P
value
less
than
0.05
was
considered
statistically
significant.
Pearson's
correlation
coefficient
was
used
to
assess
the
correlation
between
the
quantitative
variables.
Correlation
was
mild
if
correlation
coefficient
(r)
was
less
than
0.3,
moderate
if
0.7
>
r
>0.3,
powerful
if
more
than
0.7.
Ethical
approval
Ethical
approval
was
obtained
from
the
Research
Committee
of
Cairo
University.
Informed
written
consent
was
taken
from
all
participants
after
explaining
the
steps
of
the
study
to
them.
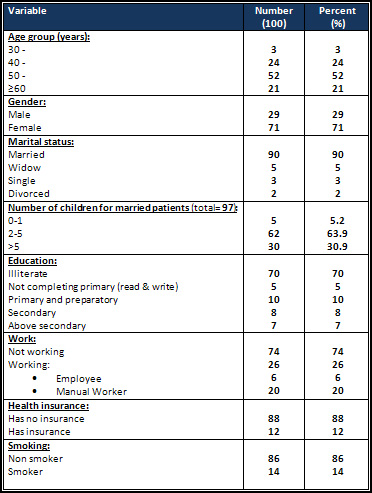
Around
half
of
the
participants
were
50
to
60
years
old
and
71%
of
them
were
females.
Seventy
percent
of
the
participants
were
illiterate
and
74%
were
unemployed.
Most
of
the
study
participants
(88%)
had
no
health
insurance
(Table
1).
Table
1:
Socio-demographic
characteristics
of
the
diabetic
patients
attending
diabetic
clinic
in
2011
Figure
1:
Reasons
stated
by
the
study
participants
for
not
attending
for
the
screening
of
DR
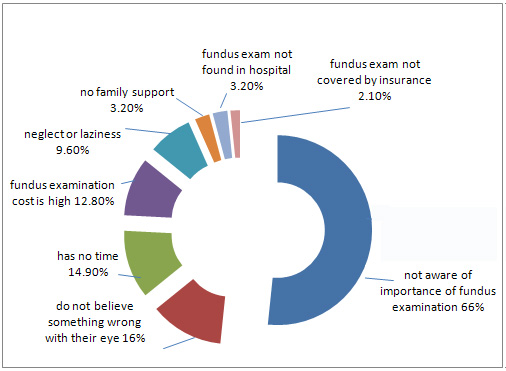
The
range
of
age
of
onset
of
diabetes
was
from
34
-
68
years;
the
mean
was
44.24
±
7.94
years.
The
range
of
the
duration
of
diabetes
was
from
0.5
to
30
years;
the
mean
was
11.13
±
6.61
years.
Family
history
of
diabetes
was
positive
in
65%
of
the
participants.
Around
half
of
the
participants
(51%)
were
taking
anti-hyperglycemic
drugs
for
control
of
diabetes;
22%
were
on
insulin
and
27%
were
on
combined
insulin
and
oral
hypoglycemic
drug.
Vitamin
B
complex
was
taken
by
only
26%
of
the
participants
for
associated
diabetic
neuropathy,
and
only
9%
of
them
were
taking
Aspirin
for
associated
ischemic
heart
diseases.
Regarding
history
of
previous
ophthalmic
diseases,
thirty-six
percent
had
history
of
cataract
(33
of
them
were
treated
by
cataract
operation),
16%
had
history
of
retinal
affection
(treated
by
retinal
laser
or
injection),
16%
had
recurrent
eye
infections,
4%
had
glaucoma
and
2%
had
pterygium.
Awareness
regarding
diabetes
complications
Most
of
the
participants
(79%)
were
aware
of
diabetic
complications
on
various
body
organs
while
85%
of
them
were
aware
of
diabetes
complications
on
the
eye.
From
those,
38.8%
of
the
participants
were
aware
that
diabetes
may
cause
blindness
or
diminution
of
vision,
35.3%
were
aware
that
diabetes
may
cause
retinal
affection
and
31.8%
were
aware
that
diabetes
may
cause
cataract.
Only
10.6%
and
5.9%
mentioned
glaucoma
and
recurrent
eye
infections
as
eye
complications
of
diabetes.
Less
than
half
of
them
(42.4%)
didn`t
know
what
the
exact
effect
of
diabetes
on
the
eye
is,
although
they
knew
that
diabetes
affects
the
eye.
Table
2
shows
the
relation
between
awareness
of
diabetic
eye
complications
and
some
variables.
Click
here
for
Table
2:
Relation
between
awareness
of
diabetic
eye
complications
and
importance
of
screening
and
some
variables
Awareness
regarding
screening
of
DR
Most
of
the
participants
were
not
aware
of
the
importance
of
frequent
screening
of
DR
(75%),
while
20%
of
them
didn't
know
the
routine
screening
frequency.
When
asked
about
the
importance
of
regular
screening
for
DR
in
well-controlled
diabetes,
65%
stated
that
they
did
not
know,
while
15%
of
the
participants
thought
that
there
is
no
need.
Most
of
the
participants
didn't
know
whether
there
is
available
treatment
for
DR
or
not
(88%).
The
sources
of
the
participants'
knowledge
were
mainly
from
the
physicians
(71%);
the
ophthalmologist
(27.3%),
the
family
physician
(21.6%),
the
endocrinologist
(18.2%)
and
the
internal
medicine
specialist
(13.6%).
The
patients'
friends
or
relatives
were
the
second
source
of
their
knowledge
(20.5%).
Mass
media
had
a
less
important
role
in
their
knowledge
(11.4%).
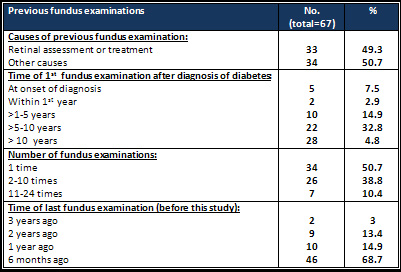
Only
67%
of
the
participants
attended
for
previous
fundus
examination
(Table
3).
From
those,
7.5%
did
fundus
examination
at
the
time
of
diagnosis
of
diabetes
while
41.8%
had
the
fundus
examination
10
years
later.
The
time
of
1st
fundus
examination
was
directly
proportionate
to
both
the
age
of
the
participants
(P
value:
0.01,
person
correlation:
0.29)
and
duration
of
diabetes
(P
value:
<0.001,
person
correlation:
0.91),
and
inversely
proportionate
to
age
of
onset
of
diabetes
(P
value:
<0.001,
person
correlation:
-0.48)
and
these
data
were
statistically
significant.
Table
3:
Causes
of
patients'
attendance
for
previous
fundus
examination
and
frequency
of
their
fundus
examination
(diabetic
clinic
in
2011)
Around
half
of
the
participants
(50.7%)
had
performed
one
fundus
examination
after
diagnosis
of
diabetes.
The
number
of
fundus
examinations
was
directly
proportionate
to
both
HBA1C
(P
value:
0.04,
person
correlation:
0.48),
and
degree
of
DR
(P
value:
0.01,
person
correlation:
0.31)
and
these
data
were
statistically
significant.
Ophthalmic
examination
Ophthalmic
examination
revealed
that
11%
of
the
participants
were
blind,
6%
had
severe
visual
impairment,
46%
percent
had
visual
impairment
and
37%
were
normal.
Also,
54%
of
the
participants
had
cataract
and
2%
had
glaucoma
at
the
time
of
the
examination.
Around
half
of
the
study
participants
(47%)
had
no
DR
at
the
time
of
the
examination,
22%
had
non
proliferative
retinopathy
and
31%
had
proliferative
retinopathy.
Only
16%
of
the
participants
had
diabetic
maculopathy.
Table
4
shows
that
65%
of
males
and
47.9%
of
females
were
affected
by
DR
while
51.7%
and
22.5%
had
proliferative
retinopathy
respectively
and
these
findings
were
statistically
significant.
Click
here
for
Table
4:
Effect
of
some
variables
on
diabetic
retinopathy
of
diabetic
patients
attending
diabetes
clinic
in
2011
Regarding
the
effect
of
smoking,
29.1%
of
non-smokers
and
42.9%
of
smokers
had
proliferative
retinopathy.
On
the
other
hand,
56.9%
of
the
participants
who
were
taking
OHD
had
no
DR,
and
92.2%
of
them
had
no
diabetic
maculopathy.
More
than
half
of
the
participants
(56.7%)
who
were
well-controlled
had
no
retinopathy
and
the
majority
of
them
(90%)
had
no
maculopathy.
The
prevalence
of
DR
in
both
hypertensive
and
non-hypertensive
participants
was
nearly
equal.
But
all
these
data
were
statistically
insignificant.
DR
was
directly
proportionate
to
duration
of
diabetes
(P
value:
0.01,
person
correlation:
0.29),
and
inversely
proportionate
to
age
of
onset
of
diabetes
(P
value:
0.03,
person
correlation:
-0.24)
and
these
data
were
statistically
significant.
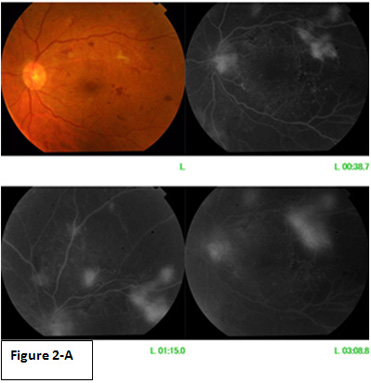
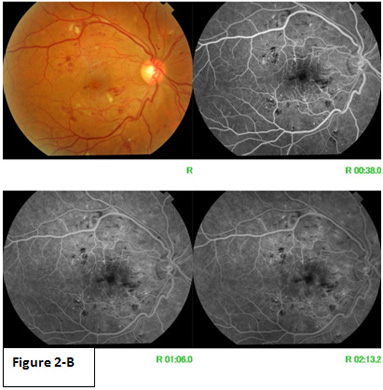
Figure
2
shows
a
sample
of
the
result
of
fundus
examination
done
to
the
study
participants.
Figure
2-A
belongs
to
a
55-year-old
male
patient
with
16-year-duration
of
type
2
diabetes.
His
last
fundus
examination
was
11
years
ago.
His
fundus
picture
reveals
proliferative
retinopathy.
On
the
other
hand,
Figure
2-B
belongs
to
a
56-year-old
male
patient
with
7-year-duration
of
type
2
diabetes.
He
has
not
performed
any
fundus
examination
before.
His
fundus
picture
reveals
non
proliferative
retinopathy
with
diffuse
macular
edema.
Figure
2:
A
Sample
of
the
result
of
fundus
examination
done
to
the
study
participants
Perception
gap
of
diabetes
control
Regarding
self-perception
of
diabetes
control,
41%
of
the
participants
thought
that
they
were
controlled,
32%
of
the
them
thought
that
they
were
not
controlled,
24%
of
them
stated
that
they
were
sometimes
controlled
and
only
3%
of
them
stated
that
they
didn't
know
whether
their
blood
glucose
was
controlled
or
not.
Assessment
of
blood
glucose
level
of
the
study
participants
revealed
that
only
30%
of
them
were
controlled.
It
was
found
that
66.7%
of
the
participants
who
thought
that
they
were
controlled
were
actually
controlled.
And
42.9%
of
them
who
thought
that
they
were
not
controlled
were
actually
not
controlled.
And
these
relations
were
statistically
significant
(Table
5).
Click
here
for
Table
5:
Distribution
of
diabetic
patients
attending
diabetic
clinic
regarding
perceived
glycemic
control
and
its
relation
to
objective
glycemic
control
(2011)
DR
is
increasingly
becoming
a
major
cause
of
blindness
throughout
the
world.
In
addition
to
loss
of
productivity,
it
has
negative
impact
on
the
patient's
quality
of
life
leading
to
additional
socioeconomic
burden
on
the
community.
Lack
of
health
education
and
dominance
of
wrong
beliefs
adversely
affect
the
progression
of
diabetic
eye
complications
among
the
Egyptian
patients.
Around
half
of
the
study
participants
had
DR
at
the
time
of
the
examination;
22%
had
non-proliferative
retinopathy
and
31%
had
proliferative
retinopathy.
Only
16%
of
the
participants
had
diabetic
maculopathy.
This
percent
is
higher
than
other
studies
done
in
Malaysia
(31.4%),
Emirates
(19%),
and
China
(25%)
(7,8,9).
Therefore
there
is
an
urgent
need
to
increase
awareness
and
knowledge
of
Egyptian
diabetic
patients
regarding
diabetic
eye
complications
as
well
as
the
importance
of
routine
eye
evaluations,
so
as
to
detect
early
ocular
complications.
In
the
current
study,
79%
of
the
patients
were
aware
of
diabetic
complications
on
various
body
organs
and
85%
were
aware
of
diabetic
complications
on
the
eye.
However,
36%
of
the
patients
do
not
know
the
exact
effect
of
diabetes
on
the
eye,
although
they
know
that
diabetes
affect
the
eye,
and
only
33%
of
them
knew
that
diabetes
causes
blindness
or
diminution
of
vision.
This
percentage
of
awareness
of
diabetic
eye
complications
was
higher
compared
to
other
studies
from
Nepal
(63.3%)
and
India
(37%)
(10,
11),
and
was
closer
to
other
studies
from
Malaysia
(86.1%)
and
Nigeria
(84.3%)
(12,
13).
On
the
other
hand,
the
percentage
of
awareness
of
blindness
as
a
complication
of
DR
was
lower
compared
to
another
study
from
Nigeria
(80.5%)
(13).
Providing
health
education
to
diabetic
patients
is
crucial
to
increase
the
patients'
compliance
to
the
routine
screening
and
to
deal
with
the
patient's
faulty
beliefs.
In
our
study,
only
25%
of
the
patients
were
aware
of
the
importance
of
screening
of
DR
while
20%
had
a
faulty
belief
that
there
is
no
need
for
regular
screening
if
diabetes
is
well
controlled.
Also,
most
of
the
participants
didn't
know
whether
there
is
available
treatment
for
DR
or
not
(88%).
This
finding
was
worrisome
especially
when
compared
to
the
earlier
study
from
India
(11),
in
which
over
90%
of
individuals
were
aware
of
the
importance
of
screening
of
DR,
approximately
one-third
were
under
the
impression
that
control
of
blood
sugar
is
enough
to
avoid
visiting
an
ophthalmologist
and
around
half
of
participants
knew
about
the
availability
of
laser
treatment
to
treat
DR.
In
the
current
study,
the
main
source
of
information
was
the
physician
(71%);
27.3%
from
the
ophthalmologist,
21.6%
from
the
family
physician,
16%
from
the
endocrinologist
and
12%
from
the
internal
medicine
specialist.
The
second
source
of
awareness
was
from
family
members
and
friends
(18%),
especially
that
65%
of
cases
had
a
positive
family
history
of
diabetes.
Mass
media
(such
as
magazines
and
radio)
and
reading
played
a
less
important
role
in
disseminating
information
among
our
study
participants
(10%),
This
may
be
due
to
the
fact
that
most
of
them
were
illiterate
(70%).
On
comparing
our
results
with
that
of
Thapa
et
al
(10),
it
was
found
that
only
half
of
the
patients
had
received
their
information
from
physicians
and
family
members
were
the
second
source
of
the
patients'
awareness.
This
finding
emphasizes
that
health
education
provided
by
trained
professionals
and
aggressive
health
campaigns
promoted
via
the
media
regarding
diabetic
eye
complications
could
help
in
dispersing
information
regarding
this
potentially
blinding
disease.
Lack
of
awareness
leads
to
delay
in
seeking
medical
advice;
this
was
evidenced
by
the
low
percentage
of
study
participants
who
have
done
previous
fundus
examination
(67%)
especially
during
the
1st
year
of
diagnosis
of
diabetes
(10.4%).
Also,
the
frequency
of
fundus
examination
is
directly
proportionate
to
HBA1c
level
and
to
the
severity
of
DR.
This
highly
suggests
that
diabetic
patients
don't
seek
medical
advice
unless
they
suffer
from
severe
visual
impairment,
which
leads
to
the
fact
that
they
perform
fundus
examination
for
diagnosis
rather
than
screening.
This
was
also
reported
by
Mohammed
&
Waziri
in
2009
(13),
where
patients
tend
to
wait
until
they
suffer
from
visual
complaints
before
screening.
In
the
present
study,
although
the
duration
of
diabetes
was
10
±
6.6
years,
33%
of
the
patients
had
never
had
a
fundus
evaluation
prior
to
this
study.
This
result
is
slightly
lower
than
in
the
study
of
Thapa
et
al,
2012
(10),
in
which
half
of
the
patients
had
never
had
fundus
examination
before
the
study.
However,
this
result
is
higher
than
the
study
of
Mohammed
and
Waziri,
2009
(13),
where
only
15.7%
had
ever
had
retinopathy
screening.
This
emphasizes
the
crucial
need
of
providing
health
education
shortly
after
the
diagnosis
of
diabetes
especially
in
a
community
with
low
literacy
as
the
case
in
our
study.
Health
education
sessions
should
highlight
the
important
of
screening
and
follow
up
visits.
In
the
current
study,
the
main
barrier
to
do
fundus
examination
was
being
unaware
of
its
importance
(66%),
in
agreement
with
a
study
conducted
in
Malaysia
(12)
where
the
main
barrier
for
diabetic
eye
screening
was
lack
of
understanding
of
diabetic
eye
disease.
In
the
present
study,
the
patients'
awareness
at
the
age
30
to
<40
years
was
the
least,
while
the
patients'
awareness
at
the
age
40
to
<50
years
was
the
highest,
but
this
result
is
insignificant.
Also,
awareness
of
illiterate
participants
was
the
least
and
the
awareness
increased
with
the
increase
in
the
level
of
education,
but
this
result
was
insignificant
due
to
the
small
number
of
educated
patients.
On
comparing
these
figures
with
that
of
Rani
et
al,
2008
(11),
it
was
found
that
the
awareness
of
the
patients
was
higher
at
the
age
>
45
years
and
lower
at
the
age
from
35
to
45
years
and
it
increased
with
the
increase
in
the
level
of
education.
This
supports
the
importance
of
providing
health
education
regarding
DR
screening
especially
to
illiterate
patients.
In
the
current
study,
51%
of
the
patients
were
taking
OHD
for
control
of
diabetes;
22%
were
on
insulin
and
27%
were
on
combined
insulin
and
OHD.
The
patients
who
were
taking
combined
treatment
for
diabetes
were
more
aware
than
other
patients,
and
this
result
was
statistically
significant.
This
represents
an
indirect
relationship
as
the
patients
on
combined
treatment
for
diabetes
had
higher
exposure
rate
to
medical
health
facilities
which
had
a
positive
impact
on
their
health
literacy.
In
addition,
awareness
was
higher
among
patients
with
positive
family
history
of
diabetes
than
patients
with
negative
family
history,
and
this
result
was
statistically
significant.
This
highly
suggests
that
increasing
the
health
awareness
of
all
the
family
members
of
the
patients
is
an
important
step
to
battle
against
DR.
In
our
study,
it
was
found
that
DR
is
directly
proportionate
to
duration
of
diabetes
and
inversely
proportionate
to
age
of
onset
of
diabetes
and
these
data
were
statistically
significant.
Also
Herman
et
al,
in
1994
(14)
reported
that
retinopathy
was
associated
with
the
duration
of
diabetes
and
hyperglycemia.
The
same
finding
was
also
reported
in
another
study
conducted
in
Egypt
(15).
This
highlights
the
necessity
of
creating
awareness
among
diabetics
of
the
importance
of
routine
eye
evaluations,
so
as
to
detect
early
ocular
complications
that
may
arise
from
diabetes
mellitus.
Limitations
of
the
study:
The
findings
of
this
study
can't
be
generalized
beyond
the
studied
cases
because
the
sample
was
collected
from
one
clinic
and
the
number
of
cases
is
too
limited
for
broad
generalizations.
Awareness
creation
is
the
corner-stone
of
any
program
aimed
at
reducing
Diabetic
Retinopathy.
It
was
found
that
there
was
general
awareness
of
diabetic
retinopathy
among
the
majority
of
the
study
participants;
however
there
was
little
awareness
of
the
importance
of
the
screening.
Around
half
of
the
participants
had
performed
only
one
fundus
examination
after
diagnosis
of
diabetes.
The
main
barrier
for
performing
the
fundus
examination
was
lack
of
awareness
of
its
importance.
Physicians
should
provide
patient
centered
care
to
address
the
patient
barriers,
provide
individual
care
for
each
patient
and
give
health
education
to
motivate
patients
and
increase
adherence
to
the
screening
examination.
1)
American
Diabetes
Association.
Initial
evaluation
and
diabetes
management
planning.
Sec.
3.
In
Standards
of
Medical
Care
in
Diabetes-2015.
Diabetes
Care
2015;38(Suppl.
1):S17-S19
2)
International
Diabetes
Federation
(IDF).
Diabetes
Atlas,
6th
ed.
International
Diabetes
Federation,
2013.
3)
Ciulla
TA,
Amador
AG,
Zinman
B.
Diabetic
Retinopathy
and
Diabetic
Macular
Edema,
pathophysiology,
screening,
and
novel
therapies.
Diabetes
Care.
2003;vol.
26(
9):
2653-2664.
doi:
10.2337/diacare.26.9.2653
4)
Standards
of
medical
care
in
diabetes-2015:
summary
of
revisions.
Diabetes
care
2015;
38
suppl:S4
5)
World
Health
Organization
(WHO):
Programme
for
the
prevention
of
blindness-Management
of
Low
Vision
in
Children-
report
of
a
WHO
consultation.
Bankok
1992;
7
6)
Knudsen
LL,
Lervang
HH,
Lundbye-Christensen
S,
Gorst-Rasmussen
A.
The
North
Jutland
Country
Diabetic
Retinopathy
Study
(NCDRS)
2.
Non-ophthalmic
parameters
and
clinically
significant
macular
edema.
Br
J
Ophthalmol.2007;91:1593-1595.
7)
Addoor
KR,
Bhandary
SV,
Khanna
R,
et
al.,
Assessment
of
Awareness
of
Diabetic
Retinopathy
Among
the
Diabetics
Attending
the
Peripheral
Diabetic
Clinics
in
Melaka,
Malaysia.
Med
J
Malaysia.
2011;
vol
66(1):
48-52
8)
Al-Maskari
F,
El-Sadig
M,
Prevalence
of
diabetic
retinopathy
in
the
United
Arab
Emirates:
a
cross-sectional
survey.
BMC
Ophthalmology.
2007;7:11
9)
Du
ZD,
Hu
LT,
Zhao
GQ,
Ma
Y,
Zhou
ZY,
Jiang
T.
Epidemiological
characteristics
and
risk
factors
of
diabetic
retinopathy
in
type
2
diabetes
mellitus
in
Shandong
Peninsula
of
China.
Int
J
Ophthalmol.
2011;4(2):202-206
10)
Thapa
R,
Paudyal
G,
Maharjan
N,
et
al.
Demographics
and
awareness
of
diabetic
retinopathy
among
diabetic
patients
attending
the
vitreo-retinal
service
at
a
tertiary
eye
care
center
in
Nepal.
Nepal
J
Ophthalmol.
2012;
4(7):10-16.
11)
Rani
PK,
Raman
R,
Subramani
S,
Perumal
G,
Kumaramanickavel
G,
Sharma
T.
Knowledge
of
diabetes
and
diabetic
retinopathy
among
rural
populations
in
India,
and
the
influence
of
knowledge
of
diabetic
retinopathy
on
attitude
and
practice.
Rural
and
Remote
Health.2008;8:838.
12)
Tajunisah
I,
Wong
PS,
Tan
LT,
Rokiah
P,
Reddy
SC.
Awareness
of
eye
complications
and
prevalence
of
retinopathy
in
the
first
visit
to
eye
clinic
among
type
2
diabetic
patients.
Int
J
Ophthalmol.
2011;4(5):519-524
13)
Mohammed
I,
Waziri
AM.
Awareness
of
Diabetic
Retinopathy
amongst
Diabetic
Patients
at
the
Murtala
Mohammed
Hospital,
Kano,
Nigeria.
Nigerian
medical
journal.2009;50:38-41.
14)
Herman
WH,
Aubert
RE,
Engelgau
MM,
et
al.
Diabetes
mellitus
in
Egypt:
glycaemic
control
and
microvascular
and
neuropathic
complications.
Diabet
Med,
1998;15:1045-
51.
15)
El-Shazly
M,
Zeid
M,
Osman
A.
Risk
factors
for
eye
complications
in
patients
with
diabetes
mellitus:
development
and
progression.
Eastern
Mediterranean
Health
Journal,
2000;2/3:313-325
|
|
.................................................................................................................

|
| |
|

