|
Chronic obstructive pulmonary
disease may be one of the terminal endpoints
of the sickle cell diseases
Mehmet Rami
Helvaci (1)
Sibel Dogru (2)
(1) Medical Faculty of Mustafa Kemal University,
Professor of Internal Medicine, M.D.
(2) Medical Faculty of the Mustafa Kemal University,
Assistant Professor of Pulmonary Medicine, M.D.
Correspondence:
Mehmet Rami Helvaci, M.D.
Medical Faculty of the Mustafa Kemal University,
31100, Serinyol, Antakya, Hatay, TURKEY
Phone: 00-90-326-2291000 (Internal 3399) Fax:
00-90-326-2455654
Email: mramihelvaci@hotmail.com
|
Abstract
Background: Sickle
cell diseases (SCDs) are chronic destructive
processes on vascular endothelium initiating
at birth all over the body. We tried to
understand whether or not there is an
association between chronic obstructive
pulmonary disease (COPD) and severity
of the SCDs.
Methods: All
patients with the SCDs were taken into
the study.
Results: The
study included 411 patients with the SCDs
(199 females and 212 males). There were
60 patients (14.5%) with the COPD. Mean
age of the patients was significantly
higher in the COPD group (33.0 versus
29.5 years, P=0.005). The male ratio was
significantly higher in the COPD group,
too (80.0% versus 46.7%, P<0.001).
Smoking was also higher in the COPD group,
significantly (36.6% versus 9.9%, P<0.001).
Parallel to the smoking, alcoholism was
also higher among the COPD cases, significantly
(3.3% versus 0.8%, P<0.05). Beside
these, transfused red blood cell units
in their lives (69.1 versus 32.9, P=0.001),
priapism (10.0% versus 1.9%, P<0.001),
leg ulcers (26.6% versus 11.6%, P<0.001),
digital clubbing (25.0% versus 7.1%, P<0.001),
coronary heart disease (26.6% versus 13.1%,
P<0.01), chronic renal disease (16.6%
versus 7.1%, P<0.01), and stroke (20.0%
versus 7.9%, P<0.001) were all higher
among the COPD cases, significantly.
Conclusion: SCDs
are chronic catastrophic processes on
vascular endothelium particularly at the
capillary level, and terminate with accelerated
atherosclerosis induced end-organ failures
in early years of life. COPD may be one
of the terminal endpoints of the diseases.
Key words: Sickle
cell diseases, chronic obstructive pulmonary
disease, chronic endothelial damage
|
Chronic endothelial damage induced atherosclerosis
may be the major cause of aging and death by
causing disseminated tissue ischemia all over
the body. For example, cardiac cirrhosis develops
due to the prolonged hepatic hypoxia in patients
with pulmonary and/or cardiac diseases. Probably
the whole afferent vasculature including capillaries
are involved in the process. Some of the well-known
accelerators of the inflammatory process are
physical inactivity, weight gain, smoking, and
alcohol intake for the development of irreversible
endpoints including obesity, hypertension (HT),
diabetes mellitus (DM), cirrhosis, peripheric
artery disease (PAD), chronic obstructive pulmonary
disease (COPD), chronic renal disease (CRD),
coronary heart disease (CHD), mesenteric ischemia,
osteoporosis, and stroke, all of which terminate
with early aging and death. They were researched
under the title of metabolic syndrome in the
literature, extensively (1, 2). Similarly, sickle
cell diseases (SCDs) are chronic catastrophic
processes on vascular endothelium, particularly
at the capillary level. Hemoglobin S (HbS) causes
loss of elastic and biconcave disc shaped structures
of red blood cells (RBCs). Probably, loss of
elasticity is the major problem, since sickling
is rare in the peripheric blood samples of the
SCDs patients associated with thalassemia minors,
and human survival is not so affected in hereditary
spherocytosis or elliptocytosis. Loss of elasticity
is probably present in whole lifespan, but exaggerated
with increased metabolic rate and various stresses
of the body. The hard cells induced prolonged
endothelial inflammation, remodeling, and fibrosis
mainly at the capillary level terminate with
disseminated tissue hypoxia all over the body
(3, 4). On the other hand, obvious vascular
occlusions may not develop in greater vasculature
due to the transport instead of distribution
function of them. We tried to understand whether
or not there is an association between COPD
and severity of SCDs in the present study.
The study was performed in Medical Faculty
of the Mustafa Kemal University between March
2007 and July 2015. All patients with the SCDs
were studied. The SCDs are diagnosed with the
hemoglobin electrophoresis performed via high
performance liquid chromatography (HPLC) method.
Medical histories including smoking habit, regular
alcohol consumption, painful crises per year,
transfused RBC units in their lives, surgical
operations, priapism, leg ulcers, and stroke
were learnt. Patients with a history of one
pack-year were accepted as smokers, and one
drink-year were accepted as drinkers. Cases
with acute painful crises or any other inflammatory
event were treated at first, and then the laboratory
tests and clinical measurements were performed
on the silent phase. A check up procedure including
serum iron, iron binding capacity, ferritin,
creatinine, liver function tests, markers of
hepatitis viruses A, B, and C and human immunodeficiency
virus, a posterior-anterior chest x-ray film,
an electrocardiogram, a Doppler echocardiogram
both to evaluate cardiac walls and valves and
to measure the systolic blood pressure (BP)
of pulmonary artery, an abdominal ultrasonography,
a computed tomography of brain, and a magnetic
resonance imaging (MRI) of hips was performed.
Other bones for avascular necrosis were scanned
according to the patients' complaints. So avascular
necrosis of bones was diagnosed by means of
MRI (5). Stroke is diagnosed by the computed
tomography of brain. Acute chest syndrome is
diagnosed clinically with the presence of new
infiltrates on chest x-ray film, fever, cough,
sputum production, dyspnea, or hypoxia in the
patients (6). An x-ray film of abdomen in upright
position was taken just in patients with abdominal
distention or discomfort, vomiting, obstipation,
or lack of bowel movement. The criterion for
diagnosis of COPD is post-bronchodilator forced
expiratory volume in one second/forced vital
capacity of less than 70% (7). Systolic BP of
the pulmonary artery of 40 mmHg or higher is
accepted as pulmonary hypertension (8). CRD
is diagnosed with a persistent serum creatinine
level of 1.3 mg/dL in males and 1.2 mg/dL in
females. Cirrhosis is diagnosed with findings
of physical examination, hepatic function tests,
ultrasonographic findings, and histologic procedure
in case of indication. Digital clubbing is diagnosed
with the ratio of distal phalangeal diameter
to interphalangeal diameter which is greater
than 1.0 and with the presence of Schamroth's
sign (9, 10). Associated thalassemia minors
are detected with serum iron, iron binding capacity,
ferritin, and hemoglobin electrophoresis performed
via HPLC method. An exercise electrocardiogram
is just performed in cases with an abnormal
electrocardiogram and/or angina pectoris. Coronary
angiography is taken just for the exercise electrocardiogram
positive cases. So CHD was diagnosed either
angiographically or with the Doppler echocardiographic
findings as the movement disorders in the cardiac
walls. Rheumatic heart disease is diagnosed
with the echocardiographic findings, too. Ileus
is diagnosed with gaseous distention of isolated
segments of bowel, vomiting, obstipation, cramps,
and with the absence of peristaltic activity
of the abdomen. Ophthalmologic examination was
performed according to the patients' complaints.
Eventually, cases with COPD and without were
collected into the two groups, and they were
compared in between. Mann-Whitney U test, Independent-Samples
t test, and comparison of proportions were used
as the methods of statistical analyses.
The
study
included
411
patients
with
the
SCDs
(199
females
and
212
males).
There
were
60
patients
(14.5%)
with
the
COPD.
Mean
age
of
patients
was
significantly
higher
in
the
COPD
group
(33.0
versus
29.5
years,
P=0.005).
The
male
ratio
was
significantly
higher
in
the
COPD
group,
too
(80.0%
versus
46.7%,
P<0.001).
Smoking
was
also
higher
among
the
COPD
cases,
significantly
(36.6%
versus
9.9%,
P<0.001).
Parallel
to
the
smoking,
alcoholism
was
also
higher
among
the
COPD
cases,
significantly
(3.3%
versus
0.8%,
P<0.05).
Prevalence
of
associated
thalassemia
minors
were
similar
in
both
groups
(71.6%
versus
66.6%
in
the
COPD
group
and
other,
respectively,
P>0.05)
(Table
1).
On
the
other
hand,
transfused
RBC
units
in
their
lives
(69.1
versus
32.9,
P=0.001),
priapism
(10.0%
versus
1.9%,
P<0.001),
leg
ulcers
(26.6%
versus
11.6%,
P<0.001),
digital
clubbing
(25.0%
versus
7.1%,
P<0.001),
CHD
(26.6%
versus
13.1%,
P<0.01),
CRD
(16.6%
versus
7.1%,
P<0.01),
and
stroke
(20.0%
versus
7.9%,
P<0.001)
were
all
higher
among
the
COPD
cases,
significantly
(Table
2).
The
differences
according
to
the
mean
white
blood
cell
(WBC)
counts,
hematocrit
(Hct)
value,
and
platelet
(PLT)
counts
of
peripheric
blood
were
nonsignificant
(P>0.05)
between
the
two
groups
(Table
3).
Beside
these
there
were
three
patients
with
sickle
cell
retinopathy,
all
of
them
were
found
in
cases
without
the
COPD.
There
were
27
mortality
during
the
nine-year
follow
up
period,
and
14
of
them
were
males.
The
mean
ages
of
mortality
were
33.6
±
9.5
(range
19-47)
in
females
and
30.8
±
8.9
years
(range
19-50)
in
males
(P>0.05).
Additionally,
there
were
four
patients
with
HBsAg
positivity
(0.9%)
but
HBV
DNA
was
positive
in
none
of
them
by
polymerase
chain
reaction
(PCR)
method.
Although
antiHCV
was
positive
in
25
(6.0%)
of
the
study
cases,
HCV
RNA
was
detected
as
positive
just
in
four
patients
by
PCR
method.
Table
1:
Characteristic
features
of
the
study
cases
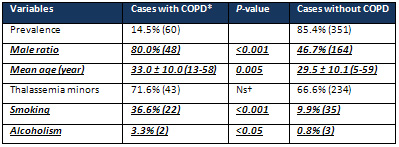
*Chronic
obstructive
pulmonary
disease
†Nonsignificant
(P>0.05)
Table
2:
Associated
pathologies
of
the
study
cases
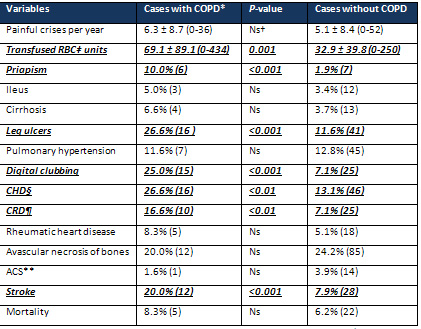
*Chronic
obstructive
pulmonary
disease
†Nonsignificant
(P>0.05)
‡Red
blood
cell
§Coronary
heart
disease
Chronic
renal
disease
**Acute
chest
syndrome
Table
3:
Peripheric
blood
values
of
the
study
cases
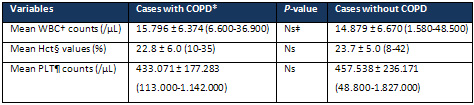
*Chronic
obstructive
pulmonary
disease
†White
blood
cell
‡Nonsignificant
(P>0.05)
§Hematocrit
Platelet
Chronic
endothelial
damage
induced
atherosclerosis
may
be
the
most
common
type
of
vasculitis,
and
the
leading
cause
of
morbidity,
mortality,
and
aging
in
human
beings.
Although
it
is
much
more
common
in
the
elderly,
chronic
inflammatory
processes
including
SCDs,
rheumatologic
disorders,
cancers,
and
chronic
infections
decrease
the
age
of
involvement.
Probably
the
whole
afferent
vasculature
including
capillaries
are
involved
in
the
process.
Much
higher
BP
of
the
afferent
vasculature
may
be
the
major
underlying
cause,
and
efferent
vascular
endothelium
are
probably
protected
due
to
the
much
lower
BP
in
them.
Secondary
to
the
chronic
endothelial
damage,
inflammation,
and
fibrosis,
vascular
walls
become
thickened,
their
lumens
are
narrowed,
and
they
lose
their
elastic
natures
which
reduce
the
blood
flow
and
increase
BP
further.
Although
early
withdrawal
of
the
causative
factors
including
physical
inactivity,
weight
gain,
smoking,
and
alcohol
intake
may
prevent
terminal
consequences,
after
development
of
cirrhosis,
COPD,
CRD,
CHD,
PAD,
or
stroke,
the
endothelial
changes
may
not
be
reversed
completely
due
to
the
fibrotic
nature
of
them
(11).
SCDs
are
life-threatening
genetic
disorders
nearly
affecting
100,000
individuals
in
the
United
States
(12).
As
a
difference
from
other
causes
of
atherosclerosis,
the
SCDs
probably
keep
vascular
endothelium
particularly
at
the
capillary
level
(13),
since
the
capillary
system
is
the
main
distributor
of
the
hard
RBCs
to
the
tissues.
The
hard
cells
induced
chronic
endothelial
damage,
inflammation,
and
fibrosis
build
up,
an
advanced
atherosclerosis
in
much
younger
ages
of
the
patients.
As
a
result,
lifespans
of
the
patients
with
SCDs
were
48
years
in
females
and
42
years
in
males
in
the
literature
(14),
whereas
they
were
33.6
and
30.8
years
in
the
present
study,
respectively.
The
great
differences
may
be
secondary
to
delayed
initiation
of
hydroxyurea
therapy
and
inadequate
RBC
supports
in
emergencies
in
our
country.
On
the
other
hand,
longer
lifespan
of
females
with
the
SCDs
(14)
and
longer
overall
survival
of
females
in
the
world
(15)
can
not
be
explained
by
the
atherosclerotic
effects
of
smoking
or
alcohol
alone,
instead
it
may
be
explained
by
more
physical
power
requiring
role
of
male
sex
in
life
that
may
terminate
with
an
exaggerated
sickling
and/or
atherosclerosis
all
over
the
body
(16).
COPD
is
the
third
leading
cause
of
death
with
differing
causes,
pathogenic
mechanisms,
and
physiological
effects,
worldwide
(17).
It
is
an
inflammatory
disease
that
may
mainly
affect
the
pulmonary
vasculature,
and
aging,
smoking,
and
excess
weight
may
be
major
causes.
As
also
observed
in
the
present
study,
regular
alcohol
consumption
may
also
take
place
in
the
inflammatory
process.
Similarly,
COPD
was
one
of
the
most
frequent
diagnoses
in
patients
with
alcohol
dependence
in
another
study
(18).
Additionally,
30-day
readmission
rate
was
higher
in
COPD
patients
with
alcoholism
(19).
Probably
the
accelerated
atherosclerotic
process
is
the
main
structural
background
of
functional
changes
characteristic
of
the
COPD.
The
inflammatory
process
of
endothelium
is
enhanced
by
release
of
various
chemicals
by
inflammatory
cells,
and
it
terminates
with
fibrosis,
atherosclerosis,
and
pulmonary
losses.
Although
COPD
may
mainly
be
an
accelerated
atherosclerotic
process
of
the
pulmonary
vasculature,
there
are
several
reports
about
coexistence
of
an
associated
endothelial
inflammation
all
over
the
body
(20,
21).
For
example,
there
may
be
a
close
relationships
between
COPD,
CHD,
PAD,
and
stroke
in
a
previous
study
(22).
Similarly,
two-thirds
of
mortality
were
caused
by
cardiovascular
diseases
and
lung
cancers,
and
CHD
was
the
most
common
one
among
them
in
a
multi-center
study
performed
on
5,887
smokers
(23).
When
the
hospitalizations
were
researched,
the
most
common
causes
were
the
cardiovascular
diseases
again
(23).
In
another
study,
27%
of
all
mortality
was
due
to
the
cardiovascular
causes
in
the
moderate
and
severe
COPD
patients
(24).
As
also
shown
in
a
previous
study
(25),
COPD
may
be
one
of
the
terminal
endpoints
of
SCDs
due
to
the
higher
prevalences
of
priapism,
leg
ulcers,
clubbing,
CHD,
CRD,
and
stroke
in
the
group
with
COPD
in
the
present
study.
Smoking
may
have
a
major
role
in
systemic
atherosclerotic
processes
such
as
COPD,
digital
clubbing,
cirrhosis,
CRD,
PAD,
CHD,
stroke,
and
cancers
(11,
26).
Its
atherosclerotic
effects
are
the
most
obvious
in
Buerger's
disease
and
COPD.
Buerger's
disease
is
an
inflammatory
process
terminating
with
obliterative
changes
in
small
and
medium-sized
vessels,
and
it
has
never
been
reported
in
the
absence
of
smoking.
Smoking
induced
endothelial
damage
probably
affects
pulmonary
vasculature
much
more
than
the
other
organs
due
to
the
higher
concentration
of
its
products
in
the
respiratory
system.
But
it
may
even
cause
cirrhosis,
CRD,
PAD,
CHD,
stroke,
and
cancers
with
the
transport
of
its
products
in
the
blood.
COPD
may
also
be
accepted
as
a
localized
Buerger's
disease
of
the
lungs.
Although
its
strong
atherosclerotic
effects,
smoking
in
human
beings
and
nicotine
administration
in
animals
may
be
associated
with
some
weight
loss
(27),
there
may
be
an
increased
energy
expenditure
during
smoking
(28),
and
nicotine
may
decrease
caloric
intake
in
a
dose-related
manner
(29).
Nicotine
may
lengthen
intermeal
time,
and
decrease
amount
of
meal
eaten
(30).
Body
mass
index
(BMI)
seems
to
be
the
highest
in
former,
the
lowest
in
current,
and
medium
in
never
smokers
(31).
Similarly,
smoking
may
also
show
the
weakness
of
volition
to
control
eating,
and
prevalences
of
HT,
DM,
and
smoking
were
the
highest
in
the
highest
triglyceride
having
group
as
a
significant
parameter
of
the
metabolic
syndrome
(32).
Additionally,
although
CHD
were
detected
with
similar
prevalences
in
both
sexes
(26),
smoking
and
COPD
were
higher
in
males
against
the
higher
prevalences
of
BMI
and
its
consequences
including
dyslipidemia,
HT,
and
DM
in
females.
Probably
tobacco
smoke
induced
acute
inflammation
on
vascular
endothelium
all
over
the
body
is
the
major
cause
of
loss
of
appetite,
since
the
body
doesn't
want
to
eat
during
fighting.
On
the
other
hand,
when
we
thought
of
some
antidepressant
properties
of
smoking
and
alcohol,
the
higher
prevalences
of
them
may
also
indicate
some
additional
stresses
on
male
sex
in
life
and
shortened
survival
of
them.
Regular
alcohol
consumption
may
also
cause
an
endothelial
inflammation
all
over
the
body
(33).
Similar
to
the
tobacco
smoke,
alcohol
leads
to
an
increased
proinflammatory
cytokine
secretion
and
reactive
oxygen
species
(ROS)
production
by
tissue
macrophages
that
damage
organs
via
oxidative
stresses,
and
these
effects
lie
far
beyond
lung
and
liver.
Against
harmful
effects
of
the
ROS,
there
are
enzymatic
and
non-enzymatic
antioxidants
in
the
body.
Enzymatic
ones
include
catalase,
superoxide
dismutase,
glutathione
reductase,
and
glutathione
peroxidase
and
non-enzymatic
ones
include
glutathione,
carotene,
bilirubin,
tocopherol,
uric
acid,
and
metal
ions
(34).
In
a
previous
study,
both
tobacco
smoke
and
ethyl
alcohol
resulted
in
a
change
of
glutathione
levels
in
serum
and
tissues
in
rats,
and
tobacco
smoke
had
the
strongest
effect
on
protein
nitrozylation
in
the
brain
(34).
Ethyl
alcohol
had
effects
on
glutathione
level
in
serum,
kidney,
and
brain,
and
superoxide
dismutase
activity
in
the
brain
(34).
Chronic
endothelial
effects
of
alcohol
may
even
be
seen
in
the
absence
of
a
significant
liver
disease.
For
example,
erectile
dysfunction
was
significantly
higher
among
aborigines
with
the
risk
of
alcohol
dependence
in
another
study
(35).
There
was
a
significant
increase
in
leukocyte
adhesion
after
chronic
alcohol
exposition
in
pancreas,
and
histological
changes
and
cytokine
levels
correlated
with
the
duration
of
exposition
in
rats
in
another
study
(36).
Probably,
cirrhosis
is
also
a
capillary
endothelial
inflammation
terminated
with
disseminated
hepatic
destruction
(37),
and
it
may
even
be
accepted
as
a
localized
Buerger's
disease
of
the
liver
caused
by
alcohol.
Stromal
cells
including
hepatic
stellate
and
endothelial
cells
have
been
proposed
to
control
the
balance
between
hepatic
fibrosis
and
regeneration,
but
chronic
damage
eventually
leads
to
progressive
substitution
of
hepatic
parenchyma
by
scar
tissue
resulting
with
cirrhosis
(38).
Although
atherosclerotic
effects
of
alcohol
are
the
most
obvious
on
liver
due
to
the
highest
concentrations
of
its
products
via
the
portal
blood
flow
(33),
alcohol
may
even
cause
COPD,
digital
clubbing,
CRD,
PAD,
CHD,
stroke,
and
cancers
like
other
atherosclerotic
endpoints
by
the
transport
of
its
products
within
the
blood.
Digital
changes
may
help
to
identify
some
systemic
disorders
within
the
body.
For
example,
digital
clubbing
is
characterized
by
loss
of
normal
<165°
angle
between
the
nailbed
and
fold,
increased
convexity
of
the
nail
fold,
and
thickening
of
the
whole
distal
finger
(39).
Some
authors
found
clubbing
in
0.9%
of
all
patients
admitted
to
the
department
of
internal
medicine
(9),
whereas
the
prevalence
was
4.2%
in
both
sexes
in
our
university
(11).
The
exact
cause
and
significance
is
unknown
but
chronic
tissue
hypoxia
induced
vasodilation
and
secretion
of
growth
factors
have
been
proposed
(40-43).
In
the
above
study,
only
40%
of
clubbing
cases
turned
out
to
have
significant
underlying
diseases
while
60%
remained
well
over
the
subsequent
years
(9).
But
according
to
our
experiences,
digital
clubbing
is
frequently
associated
with
smoking
and
pulmonary,
cardiac,
and/or
hepatic
disorders
that
are
featuring
with
chronic
tissue
hypoxia
since
lungs,
heart,
and
liver
are
closely
related
organs
that
affect
their
functions
in
a
short
period
of
time.
Similarly,
digital
clubbing
may
be
an
indicator
of
disseminated
atherosclerosis
particularly
at
the
capillary
level
in
the
SCDs,
and
we
observed
clubbing
in
9.7%
of
all
patients
with
the
SCDs
in
the
present
study.
In
addition
to
the
SCDs,
the
higher
prevalences
of
smoking
(P<0.001)
and
clubbing
(P<0.001)
in
the
COPD
group
may
also
indicate
some
additional
roles
of
smoking
and
COPD
on
clubbing.
Leg
ulcers
are
seen
in
10
to
20%
of
patients
with
the
SCDs
(44),
and
the
ratio
was
13.8%
in
the
present
study.
The
incidence
increases
with
age,
and
they
are
also
common
in
males
and
sickle
cell
anemia
(HbSS)
cases
(44).
Similarly,
leg
ulcers
were
found
as
19.3%
in
males
versus
8.0%
in
females
(P<0.001)
in
the
present
study.
Beside
that,
mean
ages
of
the
patients
with
leg
ulcers
were
significantly
higher
than
the
others
(34.8
versus
29.2
years,
P<0.000).
The
leg
ulcers
have
an
intractable
nature,
and
around
97%
of
healed
ulcers
relapse
in
a
period
of
one
year
(45).
As
an
evidence
of
their
atherosclerotic
natures,
the
leg
ulcers
occur
in
distal
areas
with
less
collateral
blood
flow
in
the
body
(45).
Chronic
endothelial
damage
particularly
at
the
capillary
level
due
to
the
hard
RBCs
may
be
the
major
cause
in
the
SCDs
(44).
Prolonged
exposure
to
the
hard
RBCs
due
to
the
blood
pooling
in
the
lower
extremities
by
the
effect
of
gravity
may
also
explain
the
leg
but
not
arm
ulcers
in
the
SCDs.
As
also
observed
in
venous
ulcers
of
the
legs,
venous
insufficiencies
may
also
accelerate
the
process
by
causing
pooling
of
causative
hard
RBCs
in
the
legs.
Probably
pooling
of
blood
in
the
lower
extremities
is
also
true
for
the
diabetic
ulcers,
Buerger's
disease,
digital
clubbing,
varicose
veins,
and
onychomycosis.
Beside
the
hard
RBCs
of
the
SCDs,
smoking
and
alcohol
may
also
have
some
additional
roles
for
the
leg
ulcers
since
both
of
them
are
much
more
common
in
males,
and
their
atherosclerotic
effects
are
obvious
particularly
in
COPD,
Buerger's
disease,
and
cirrhosis
(44).
According
to
our
nine-year
experiences,
prolonged
resolution
of
ulcers
with
hydroxyurea
may
also
suggest
that
the
ulcers
may
be
secondary
to
increased
WBC
and
PLT
counts
induced
disseminated
endothelial
edema
particularly
at
the
capillary
level.
Stroke
is
also
a
common
complication
of
the
SCDs
(47).
Similar
to
the
leg
ulcers,
it
is
higher
in
the
HbSS
cases
(48).
Moreover,
a
higher
WBC
count
is
associated
with
a
higher
incidence
of
stroke
(49).
Sickling
induced
endothelial
injury
and
activations
of
WBC
and
PLTs
may
terminate
with
chronic
endothelial
inflammation,
edema,
remodeling,
and
fibrosis
in
the
brain
(50).
Stroke
of
the
SCDs
may
not
have
a
macrovascular
origin,
instead
disseminated
endothelial
inflammation
and
edema
may
be
much
more
important
at
the
capillary
level.
Infection,
inflammation,
and
various
stresses
may
precipitate
stroke,
since
increased
metabolic
rate
may
accelerate
sickling
and
secondary
endothelial
edema.
Similar
to
the
leg
ulcers,
a
significant
reduction
of
stroke
with
hydroxyurea
may
also
suggest
that
a
significant
proportion
of
stroke
is
secondary
to
increased
WBC
and
PLT
counts
induced
disseminated
endothelial
edema
in
the
SCDs
(13,
51).
As
a
conclusion,
SCDs
are
chronic
catastrophic
processes
on
vascular
endothelium
particularly
at
the
capillary
level,
and
terminate
with
accelerated
atherosclerosis
induced
end-organ
failures
in
early
years
of
life.
COPD
may
be
one
of
the
terminal
endpoints
of
the
diseases.
1.
Eckel
RH,
Grundy
SM,
Zimmet
PZ.
The
metabolic
syndrome.
Lancet
2005;
365:
1415-1428.
2.
Helvaci
MR,
Kaya
H,
Seyhanli
M,
Yalcin
A.
White
coat
hypertension
in
definition
of
metabolic
syndrome.
Int
Heart
J
2008;
49:
449-457.
3.
Helvaci
MR,
Aydogan
A,
Akkucuk
S,
Oruc
C,
Ugur
M.
Sickle
cell
diseases
and
ileus.
Int
J
Clin
Exp
Med
2014;
7:
2871-2876.
4.
Helvaci
MR,
Acipayam
C,
Aydogan
A,
Akkucuk
S,
Oruc
C,
Gokce
C.
Acute
chest
syndrome
in
severity
of
sickle
cell
diseases.
Int
J
Clin
Exp
Med
2014;
7:
5790-5795.
5.
Mankad
VN,
Williams
JP,
Harpen
MD,
Manci
E,
Longenecker
G,
Moore
RB,
et
al.
Magnetic
resonance
imaging
of
bone
marrow
in
sickle
cell
disease:
clinical,
hematologic,
and
pathologic
correlations.
Blood
1990;
75:
274-283.
6.
Castro
O,
Brambilla
DJ,
Thorington
B,
Reindorf
CA,
Scott
RB,
Gillette
P,
et
al.
The
acute
chest
syndrome
in
sickle
cell
disease:
incidence
and
risk
factors.
The
Cooperative
Study
of
Sickle
Cell
Disease.
Blood
1994;
84:
643-649.
7.
Global
strategy
for
the
diagnosis,
management
and
prevention
of
chronic
obstructive
pulmonary
disease
2010.
Global
initiative
for
chronic
obstructive
lung
disease
(GOLD).
8.
Fisher
MR,
Forfia
PR,
Chamera
E,
Housten-Harris
T,
Champion
HC,
Girgis
RE,
et
al.
Accuracy
of
Doppler
echocardiography
in
the
hemodynamic
assessment
of
pulmonary
hypertension.
Am
J
Respir
Crit
Care
Med
2009;
179:
615-621.
9.
Vandemergel
X,
Renneboog
B.
Prevalence,
aetiologies
and
significance
of
clubbing
in
a
department
of
general
internal
medicine.
Eur
J
Intern
Med
2008;
19:
325-329.
10.
Schamroth
L.
Personal
experience.
S
Afr
Med
J
1976;
50:
297-300.
11.
Helvaci
MR,
Aydin
LY,
Aydin
Y.
Digital
clubbing
may
be
an
indicator
of
systemic
atherosclerosis
even
at
microvascular
level.
HealthMED
2012;
6:
3977-3981.
12.
Yawn
BP,
Buchanan
GR,
Afenyi-Annan
AN,
Ballas
SK,
Hassell
KL,
James
AH,
et
al.
Management
of
sickle
cell
disease:
summary
of
the
2014
evidence-based
report
by
expert
panel
members.
JAMA
2014;
312:
1033-1048.
13.
Helvaci
MR,
Aydin
Y,
Ayyildiz
O.
Hydroxyurea
may
prolong
survival
of
sickle
cell
patients
by
decreasing
frequency
of
painful
crises.
HealthMED
2013;
7:
2327-2332.
14.
Platt
OS,
Brambilla
DJ,
Rosse
WF,
Milner
PF,
Castro
O,
Steinberg
MH,
et
al.
Mortality
in
sickle
cell
disease.
Life
expectancy
and
risk
factors
for
early
death.
N
Engl
J
Med
1994;
330:
1639-1644.
15.
Mathers
CD,
Sadana
R,
Salomon
JA,
Murray
CJ,
Lopez
AD.
Healthy
life
expectancy
in
191
countries,
1999.
Lancet
2001;
357:
1685-1691.
16.
Helvaci
MR,
Ayyildiz
O,
Gundogdu
M.
Gender
differences
in
severity
of
sickle
cell
diseases
in
non-smokers.
Pak
J
Med
Sci
2013;
29:
1050-1054.
17.
Rennard
SI,
Drummond
MB.
Early
chronic
obstructive
pulmonary
disease:
definition,
assessment,
and
prevention.
Lancet
2015;
385:
1778-1788.
18.
Schoepf
D,
Heun
R.
Alcohol
dependence
and
physical
comorbidity:
Increased
prevalence
but
reduced
relevance
of
individual
comorbidities
for
hospital-based
mortality
during
a
12.5-year
observation
period
in
general
hospital
admissions
in
urban
North-West
England.
Eur
Psychiatry
2015;
30:
459-468.
19.
Singh
G,
Zhang
W,
Kuo
YF,
Sharma
G.
Association
of
psychological
disorders
with
30-day
readmission
rates
in
patients
with
Chronic
Obstructive
Pulmonary
Disease.
Chest
2015.
doi:
10.1378/chest.
15-0449.
20.
Danesh
J,
Collins
R,
Appleby
P,
Peto
R.
Association
of
fibrinogen,
C-reactive
protein,
albumin,
or
leukocyte
count
with
coronary
heart
disease:
meta-analyses
of
prospective
studies.
JAMA
1998;
279:
1477-1482.
21.
Mannino
DM,
Watt
G,
Hole
D,
Gillis
C,
Hart
C,
McConnachie
A,
et
al.
The
natural
history
of
chronic
obstructive
pulmonary
disease.
Eur
Respir
J
2006;
27:
627-643.
22.
Mapel
DW,
Hurley
JS,
Frost
FJ,
Petersen
HV,
Picchi
MA,
Coultas
DB.
Health
care
utilization
in
chronic
obstructive
pulmonary
disease.
A
case-control
study
in
a
health
maintenance
organization.
Arch
Intern
Med
2000;
160:
2653-2658.
23.
Anthonisen
NR,
Connett
JE,
Enright
PL,
Manfreda
J;
Lung
Health
Study
Research
Group.
Hospitalizations
and
mortality
in
the
Lung
Health
Study.
Am
J
Respir
Crit
Care
Med
2002;
166:
333-339.
24.
McGarvey
LP,
John
M,
Anderson
JA,
Zvarich
M,
Wise
RA;
TORCH
Clinical
Endpoint
Committee.
Ascertainment
of
cause-specific
mortality
in
COPD:
operations
of
the
TORCH
Clinical
Endpoint
Committee.
Thorax
2007;
62:
411-415.
25.
Helvaci
MR,
Erden
ES,
Aydin
LY.
Atherosclerotic
background
of
chronic
obstructive
pulmonary
disease
in
sickle
cell
patients.
HealthMED
2013;
7:
484-488.
26.
Helvaci
MR,
Aydin
Y,
Gundogdu
M.
Smoking
induced
atherosclerosis
in
cancers.
HealthMED
2012;
6:
3744-3749.
27.
Grunberg
NE,
Greenwood
MR,
Collins
F,
Epstein
LH,
Hatsukami
D,
Niaura
R,
et
al.
National
working
conference
on
smoking
and
body
weight.
Task
Force
1:
Mechanisms
relevant
to
the
relations
between
cigarette
smoking
and
body
weight.
Health
Psychol
1992;
11:
4-9.
28.
Walker
JF,
Collins
LC,
Rowell
PP,
Goldsmith
LJ,
Moffatt
RJ,
Stamford
BA.
The
effect
of
smoking
on
energy
expenditure
and
plasma
catecholamine
and
nicotine
levels
during
light
physical
activity.
Nicotine
Tob
Res
1999;
1:
365-370.
29.
Hughes
JR,
Hatsukami
DK.
Effects
of
three
doses
of
transdermal
nicotine
on
post-cessation
eating,
hunger
and
weight.
J
Subst
Abuse
1997;
9:
151-159.
30.
Miyata
G,
Meguid
MM,
Varma
M,
Fetissov
SO,
Kim
HJ.
Nicotine
alters
the
usual
reciprocity
between
meal
size
and
meal
number
in
female
rat.
Physiol
Behav
2001;
74:
169-176.
31.
Laaksonen
M,
Rahkonen
O,
Prattala
R.
Smoking
status
and
relative
weight
by
educational
level
in
Finland,
1978-1995.
Prev
Med
1998;
27:
431-437.
32.
Helvaci
MR,
Kaya
H,
Gundogdu
M.
Association
of
increased
triglyceride
levels
in
metabolic
syndrome
with
coronary
artery
disease.
Pak
J
Med
Sci
2010;
26:
667-672.
33.
González-Reimers
E,
Santolaria-Fernández
F,
Martín-González
MC,
Fernández-Rodríguez
CM,
Quintero-Platt
G.
Alcoholism:
a
systemic
proinflammatory
condition.
World
J
Gastroenterol
2014;
20:
14660-14671.
34.
Wozniak
A,
Kulza
M,
Sezczuk-Przybyzowska
M,
Cimino
F,
Saija
A,
Ignatowicz
E,
et
al.
Selected
biochemical
parameters
of
oxidative
stress
as
a
result
of
exposure
to
tobacco
smoke
in
animals
addicted
to
ethyl
alcohol.
Przegl
Lek
2012;
69:
824-832.
35.
Chao
JK,
Ma
MC,
Lin
YC,
Chiang
HS,
Hwang
TI.
Study
on
alcohol
dependence
and
factors
related
to
erectile
dysfunction
among
aborigines
in
Taiwan.
Am
J
Mens
Health
2015;
9:
247-256.
36.
Grauvogel
J,
Grauvogel
TD,
Gebhard
MM,
Werner
J.
Combined
effects
of
chronic
and
acute
ethanol
on
pancreatic
injury
and
microcirculation.
Pancreas
2012;
41:
717-723.
37.
Helvaci
MR,
Sevinc
A,
Camci
C,
Keskin
A.
Atherosclerotic
background
of
cirrhosis
in
sickle
cell
patients.
Pren
Med
Argent
2014;
100:
127-133.
38.
Mogler
C,
Wieland
M,
König
C,
Hu
J,
Runge
A,
Korn
C,
et
al.
Hepatic
stellate
cell-expressed
endosialin
balances
fibrogenesis
and
hepatocyte
proliferation
during
liver
damage.
EMBO
Mol
Med
2015;
7:
332-338.
39.
Myers
KA,
Farquhar
DR.
The
rational
clinical
examination.
Does
this
patient
have
clubbing?
JAMA
2001;
286:
341-347.
40.
Uppal
S,
Diggle
CP,
Carr
IM,
Fishwick
CW,
Ahmed
M,
Ibrahim
GH,
et
al.
Mutations
in
15-hydroxyprostaglandin
dehydrogenase
cause
primary
hypertrophic
osteoarthropathy.
Nat
Genet
2008;
40:
789-793.
41.
Toovey
OT,
Eisenhauer
HJ.
A
new
hypothesis
on
the
mechanism
of
digital
clubbing
secondary
to
pulmonary
pathologies.
Med
Hypotheses
2010;
75:
511-513.
42.
Alam
MT,
Sheikh
SS,
Aziz
S,
Masroor
M.
An
unusual
side
effect
of
interferon
alfa
2A:
digital
clubbing.
J
Ayub
Med
Coll
Abbottabad
2008;
20:
165-166.
43.
Fomin
VV,
Popova
EN,
Burnevich
EZ,
Kuznetsova
AV.
Hippocratic
fingers:
clinical
importance
and
differential
diagnosis.
Klin
Med
(Mosk)
2007;
85:
64-68.
44.
Minniti
CP,
Eckman
J,
Sebastiani
P,
Steinberg
MH,
Ballas
SK.
Leg
ulcers
in
sickle
cell
disease.
Am
J
Hematol
2010;
85:
831-833.
45.
Trent
JT,
Kirsner
RS.
Leg
ulcers
in
sickle
cell
disease.
Adv
Skin
Wound
Care
2004:
17;
410-416.
46.
Helvaci
MR,
Sevinc
A,
Camci
C,
Keskin
A.
Smoking
and
sickle
cell
diseases.
Exp
Clin
Cardiol
2014;
20:
3706-3722.
47.
Gueguen
A,
Mahevas
M,
Nzouakou
R,
Hosseini
H,
Habibi
A,
Bachir
D,
et
al.
Sickle-cell
disease
stroke
throughout
life:
a
retrospective
study
in
an
adult
referral
center.
Am
J
Hematol
2014;
89:
267-272.
48.
Majumdar
S,
Miller
M,
Khan
M,
Gordon
C,
Forsythe
A,
Smith
MG,
et
al.
Outcome
of
overt
stroke
in
sickle
cell
anaemia,
a
single
institution's
experience.
Br
J
Haematol
2014;
165:
707-713.
49.
Helvaci
MR,
Aydogan
F,
Sevinc
A,
Camci
C,
Dilek
I.
Platelet
and
white
blood
cell
counts
in
severity
of
sickle
cell
diseases.
Pren
Med
Argent
2014;
100:
49-56.
50.
Kossorotoff
M,
Grevent
D,
de
Montalembert
M.
Cerebral
vasculopathy
in
pediatric
sickle-cell
anemia.
Arch
Pediatr
2014;
21:
404-414.
51.
Charache
S,
Terrin
ML,
Moore
RD,
Dover
GJ,
Barton
FB,
Eckert
SV,
et
al.
Effect
of
hydroxyurea
on
the
frequency
of
painful
crises
in
sickle
cell
anemia.
Investigators
of
the
Multicenter
Study
of
Hydroxyurea
in
Sickle
Cell
Anemia.
N
Engl
J
Med
1995;
332:
1317-1322.
|

