|
The Relationship between
Chronic Pain and Obesity:
The Mediating Role of Anxiety
Leila Shateri (1)
Hamid Shamsipour (2)
Zahra Hoshyari (3)
Elnaz Mousavi (4)
Leila Saleck (5)
Faezeh Ojagh (6)
(1) Ph.D.
student in Clinical Psychology, Department of
Clinical Psychology, Medicine Faculty, Shahid
Beheshti University of Medical Sciences, Tehran,
Iran.
(2) Assistant Prof. Department of Clinical Psychology,
Medicine Faculty, Shahid Beheshti University
of Medical Sciences, Tehran, Iran.
(3) Phd student in psychometric, Allameh Tabatabaee
University Tehran, Iran.
(4) Ph.D. student in Clinical Psychology, Department
of Clinical Psychology, Medicine Faculty, Shahid
Beheshti University of Medical Sciences, Tehran,
Iran.
(5) Ph.D. student in Clinical Psychology, Department
of Clinical Psychology, Medicine Faculty, Shahid
Beheshti University of Medical Sciences, Tehran,
Iran.
(6)Master degree in clinical psychology Shahid
Beheshti University of Medical Sciences, Tehran,
Iran.
Correspondence:
Hamid Shamsipour
Assistant Professor Department of Clinical Psychology,
Medicine Faculty, Shahid Beheshti University
of Medical Sciences, Tehran, Iran.
Email: hshamsipour@gmail.com
|
Abstract
Obesity
is nowadays considered as one of the problems
impairing functioning and quality of life.
Obesity is defined by body mass index
(BMI), and most studies on the association
between psychiatric disorders and obesity
have exclusively studied depression. But
there are just a few researchers that
have studied the association between obesity
and anxiety, and the mechanism of this
association remains unclear. This study
aims to evaluate the extent to which the
association between chronic pain and obesity
are mediated by anxiety and moderated
by coping strategies. The study population
comprised 200 participants (100 male and
100 female) aged between 20 and70 (M=45)
years old. All participants completed
the Pain Self-Management Checklist, Beck
Anxiety Inventory-II, and Lazarus Coping
Skills Scale. The statistically significant
paths were anxiety-pain, pain-obesity,
and anxiety-emotional coping strategies
(p<0/005). In summary, chronic pain
predicted obesity directly, and specific
coping strategies (emotional coping strategies)
did not moderate the relationship between
chronic pain, obesity and anxiety, but
anxiety mediated this relationship.
Key words:
Obesity, Anxiety, Chronic pain, coping
strategies
|
In the coming decades, global health will be
faced with enormous challenges with several
public health problems such as Obesity, major
depressive disorder (MDD), and anxiety (Kelly,
Yang, Chen, Reynolds, & He, 2008; Kessler
et al., 2003). Obesity and Major depressive
disorder and/or anxiety disorders impose a large
cost on individuals, health care services and
society and are associated with long-term disabilities,
morbidity and mortality (Müller-Riemenschneider,
Reinhold, Berghöfer, & Willich, 2008;
Pi-Sunyer, 2009). Several studies have suggested
bilateral relationship between obesity and MDD
and/or anxiety disorders and also the possibility
of their comorbidity (Afari et al., 2010; Luppino
et al., 2010).
Pain is the most common physical symptom-based
condition reported in both the general population
and in primary care (Kroenke, 2003) and it causes
several functional and work-related disabilities
(Greenberg et al., 1999; Institute of Medicine,
2011). Additionally, several studies have proved
additive and adverse effects of different kinds
of pain such as osteoarthritis pain, chronic
headaches (Bigal et al., 2007) and neuropathic
pain (Miscio et al., 2005). In obese people
the impact of pain on the functional status
and health-related quality of life is greater
than people with normal weight (Marcus, 2004;
Ray, Lipton, Zimmerman, Katz, & Derby, 2011).
The underlying mechanisms of the pain and obesity
relationship is still unclear (Rossi, Luu, DeVilbiss,
& Recober, 2013). In some literature obesity
has been defined as a pro-inflammatory state
and inflammatory mechanisms are involved in
the development of pain, so inflammation can
be considered as a part of the causal pathway.
Additionally, evidence suggested a causal relationship
between acute pain and transient insulin resistance
(Greisen et al., 2001; Ray et al., 2011). Eventually,
there is an association between depression and
both obesity and chronic pain, and obsessive
patients with comorbidity of depression and
anxiety have worse experience of pain (Ray et
al., 2011; Tietjen et al., 2007). A potential
unifying mechanism may be found in the metabolic
syndrome, which is known to be associated with
chronic pain (Loevinger, Muller, Alonso, &
Coe, 2007; Ray et al., 2011), inflammation (Lee,
Lee, Huang, & Sheu, 2007), insulin resistance
(Lann & LeRoith, 2007) and mood disorders
(Räikkönen, Matthews, & Kuller,
2007).
There are several ways and strategies to cope
with chronic pain which has been examined by
various studies (Büssing, Ostermann, Neugebauer,
& Heusser, 2010). Pain-related coping may
be defined as individuals’ attempts to
manage problems associated with their pain state
(DeGood & Tait, 2011) and according to their
ability to effect symptoms, coping strategies
has been divided into two categories: adaptive
and maladaptive. Often, adaptive and maladaptive
coping responses have been known as active and
passive responses, respectively. For instance,
adaptive coping appears in the form of staying
active and pacing problem solving, while maladaptive
coping tends to present passive strategies such
as resting and avoiding (Jensen, Turner, Romano,
& Nielson, 2008). It’s assumed that
the role of maladaptive coping strategies in
chronic pain consequences is more important
than adaptive coping strategies (Geisser, Robinson,
& Riley, 2000). This assumption has been
examined frequently in different studies. For
instance, the increased use of passive coping
responses after multidisciplinary pain treatment
has been associated with increased disabilities
and depression (Jensen, Turner, & Romano,
2007). In a study on 106 military veterans who
suffered from chronic pain, there was a strong
association among maladaptive responses, pain
interference and depression, while the relation
of adaptive coping styles and pain intensity
was considerable (Tan, Teo, Anderson, &
Jensen, 2011). It is hypothesized in the present
study that coping strategies and anxiety would
impact the relationship between chronic pain
symptoms and obesity.
This study explores the mediating role of anxiety
and moderating role of coping strategies in
the relationship between chronic pain and obesity.
As one of the inclusion criteria, participants
had to meet the criteria for chronic pain and
obesity (BMI >30). Additional inclusion criteria
for this study were being at least 18 years
of age, current self-report of chronic pain
(of more than 6 months’ duration) confirmed
by medical record and diagnosis, obesity, and
having received treatment for a painful condition
within the last 5 years (recorded in their medical
records). Participants were excluded if they
were older than 70 years old. All participants
(N=200) signed informed consent and completed
study-related tasks. Participants were selected
through accessible sampling from the general
population.
Data collection
Demographic characteristics, such as participants’
age, gender and educational level, were gathered
with relevant self-report questions.
Measures
Symptoms of anxiety were assessed by Beck anxiety
inventory (BAI-II). The 31-item self-report
Chronic Pain Inventory (CPI) was used for assessment
of pain severity. Coping strategies were evaluated
by Coping Questionnaire, developed by Lazarus
and Folkman, (1984), containing 66 items (16
distractors and 50 main items) that assess direct
confrontation, distancing, self-control, seeking
social support, accepting responsibility, evasion
and avoidance, solving planned problems and
positive re-evaluation (Sadeghi & Niknam,
2015). Lazarus reported the reliability of each
subscale from 0.66 to 0.79 and the reliability
of the coping skills was estimated 0.84 (Rajabi
Damavandi, Poushne, & Ghobari Banab, 2009).
These values reflect the desirable reliability
of the test (Sadeghi & Niknam, 2015).
Asghari-moghaddam et al (2008, 2011, 2008,
2002) assessed chronic pain using Chronic Pain
Inventory (CPI) (Asghari-moghaddam, Abedi Ghelich
Gheshlaghi,
(Asghari-moghaddam, Abedi Ghelich Gheshlaghi,
& Khalilzade Poshtgol, 2008; Asghari Moghadam,
2011; Asghari Moghadam & Golak, 2008; Asghari
Moghadam & Najarian, 2002). This inventory,
which contains 31 items, assesses pain severity,
the start time of pain, pain intensity six months
after pain start time, influence of pain on
the social and family relationships, and the
number of operations because of pain.
Statistical analysis
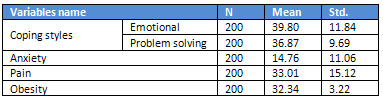
Table 1 shows the mean and standard values of
research variables: the scores mean for emotional
coping and problem solving coping were 39.80
and 36.87, respectively. Furthermore, the means
for anxiety, pain and obesity were 14.76, 33.01
and 32.34, respectively.
Table 1: Descriptive statistics of variables
Path analysis was used for analysis of research
data. As per the obtained results, anxiety proved
to be a mediating variable in the present study
and, based on literature review, pain and coping
styles have effects on obesity after they have
been affected by anxiety; therefore, the following
model was tested (Figures 1 & 2)):
Three paths from anxiety to pain, emotional
coping and problem solving coping; one direct
path from anxiety to obesity; and three direct
paths from pain, emotional coping and problem
solving coping to obesity can be observed on
the path diagram. Analysis results show that
standardized regression weight from anxiety
to emotional coping is 0.23 and p<0.001;
anxiety to problem solving coping is 0.12 and
p>0.08; anxiety to pain is 0.32 and p<0.001;
emotional coping to pain is 0.08 and p>0.23;
problem solving coping to pain is -0.18 and
p<0,01; pain to obesity is 0.25 and p<0.001;
emotional coping to obesity is-0.05 and p>0.50;
problem solving coping to obesity is-0.04 and
p>0.58; and anxiety to obesity is 0.005 and
p<0.94. Table 2 shows the foregoing results
completely. Fitness indexes did not confirm
the fitness of conceptual model with observed
data. Chi-square stood at 141, 983, the degree
of freedom at 1, and Probability level at 0.001.
Chi-square index shows the significant difference
between conceptual model and observed model.
As many references have suggested that chi-square
is dependent upon sample size, it is thus more
desirable to use other fitness indices for model
fit test. Therefore, CFI, NFI and RMSEA indices
were used. As shown in Table 3, these indices
do not confirm the models.
Click here for Table
2: Regression Weights (Default Model)
Table 3: Indices of fitness
Click here for
Figure 1: Unstandardized estimated
Click here for Figure
2: Standardized estimated
The
present
study
explored
the
relationship
between
chronic
pain
and
obesity
with
the
mediating
role
of
anxiety
and
moderating
role
of
coping
strategies.
Personal
resources
play
an
important
role
in
reduction
and
prevention
of
anxiety.
The
results
obtained
by
the
present
study
show
that
anxiety
predicts
emotional
coping
strategies.
In
other
words,
greater
anxiety
correlates
with
greater
emotional
coping
strategies.
The
result
is
consistent
with
the
findings
of
similar
studies.
For
example,
the
importance
of
dysfunctional
coping
strategies
in
predicting
anxiety
and
its
helpful
role
in
managing
anxiety
were
indicated
by
researchers
(Cooper,
Katona,
Orrell,
&
Livingston,
2006).
There
is
a
relationship
between
psychological
distress
and
different
coping
strategies.
There
are
negative
relations
between
the
problem-focused
coping
and
anxiety,
stress
and
depressive
symptoms,
while
this
relation
in
case
of
the
avoidant
coping
is
positive
(van
Berkel,
Boot,
Proper,
Bongers,
&
van
der
Beek,
2014).
Problem-focused
coping
helps
to
manage
the
stress
causing
the
problem,
and
emotional-focused
coping
diminishes
the
negative
emotions
associated
with
the
stressor
(Folkman,
Lazarus,
Dunkel-Schetter,
DeLongis,
&
Gruen,
1986).
However,
avoidance
coping,
as
a
type
of
passive
coping,
is
highly
related
to
psychological
outcomes
due
to
minimizing,
denying
or
ignoring
to
deal
with
a
stressful
situation
(Holahan,
Moos,
Holahan,
Brennan,
&
Schutte,
2005;
Snow,
Swan,
Raghavan,
Connell,
&
Klein,
2003).
Based
on
the
results
obtained
in
this
study,
there
is
a
significant
prediction
between
anxiety
and
chronic
pain.
In
other
words,
anxiety
increases
the
severity
of
pain.
Additionally,
pain,
depression
and
anxiety
frequently
co-occur
and
have
additive
and
adverse
effects
on
health-related
quality
of
life
(HRQL),
functional
impairment
and
treatment
response
(Bair,
Robinson,
Katon,
&
Kroenke,
2003;
Bair,
Wu,
Damush,
Sutherland,
&
Kroenke,
2008).
A
study
on
500
primary
care
patients
with
chronic
pain
discovered
negative
association
between
anxiety
severity
and
pain
severity
(Bair
et
al.,
2008).
There
are
some
findings
that
claim
chronic
pain
substantially
increases
the
likelihood
of
anxiety
disorder
(McWilliams,
Cox,
&
Enns,
2003).
In
other
research,
it
was
concluded
that
the
presence
of
any
of
the
five
common
pain
complaints
increased
the
likelihood
of
having
an
anxiety
disorder
significantly
(Kroenke
&
Price,
1993).
The
other
finding
of
the
current
study
is
related
to
the
prediction
of
obesity
by
chronic
pain.
The
findings
demonstrate
that
obesity
is
strongly
associated
with
chronic
regional
pain
(CRP)
as
well
as
reporting
of
musculoskeletal
pain
at
specific
members
such
as
the
knees.
Furthermore,
obesity
is
associated
with
more
severe
pain
(Deere
et
al.,
2012).
Obesity
is
also
associated
with
an
increased
risk
of
pain
at
any
members,
as
well
as
a
range
of
musculoskeletal
pain
phenotypes.
The
strongest
associations,
as
observed
in
analyses
on
boys
and
girls
combined,
were
between
obesity,
risk
of
CRP,
and
knee
pain.
Whereas
CRP
also
comprised
pain
at
shoulders,
lower
back,
and
hips,
all
of
which
showed
weak
evidence
of
an
association
with
obesity,
the
relationship
between
obesity
and
CRP
may
have
been
driven
by
that
with
knee
pain.
Obesity
was
also
associated
with
pain
severity,
as
reflected
by
higher
average
pain
scores
in
obese
participants
reporting
CRP
and
knee
pain
(Deere
et
al.,
2012).
However,
the
findings
of
the
present
study
are
in
contrast
with
those
of
other
researchers
that
claim
obesity
influences
the
pain.
It
was
found
that
pain
predicts
obesity.
In
general,
the
path
analysis
(as
shown
above)
shows
that
anxiety
is
a
predictor
of
chronic
pain
and
chronic
pain
can
predict
obesity.
On
the
other
hand,
anxiety
can
predict
the
emotional
coping
strategies,
but
the
emotional
coping
strategies
are
not
able
to
predict
obesity.
Limitations
The
present
research
was
faced
with
some
limitations,
such
as
a
small
study
population.
The
population
of
the
present
research
being
200
individuals
can
be
one
of
the
reasons
for
Indices
of
fitness
not
confirming
any
fitness
between
conceptual
model
and
observed
data.
Another
limitation
was
the
cross-sectional
design,
and
the
authors
of
the
present
study
recommend
that
this
research
be
repeated
in
a
longitudinal
prospective
design.
1.
Afari,
N.,
Noonan,
C.,
Goldberg,
J.,
RoyByrne,
P.,
Schur,
E.,
Golnari,
G.,
&
Buchwald,
D.
(2010).
Depression
and
obesity:
do
shared
genes
explain
the
relationship?
Depression
and
anxiety,
27(9),
799-806.
doi:
http://dx.doi.org/10.1002/da.20704
2.
Asghari-moghaddam,
M.
A.,
Abedi
Ghelich
Gheshlaghi,
M.,
&
Khalilzade
Poshtgol,
M.
(2008).
Investigation
of
psychometric
characteristics
of
pain
self-management
checklist
Paper
presented
at
the
Congress
of
Cognitive
Behavioral
Therapy.
3.
Asghari
Moghadam,
M.
(2011).
Screening
of
chronic
pain
patient
inventory
book.
Iran:
Developmental
publication.
4.
Asghari
Moghadam,
M.,
&
Golak,
N.
(2008).
Investigatin
of
multiple
pain
inventories
in
Iranian
population
of
chronic
pain.
Journal
of
Psychology,
1(12),
55-70.
5.
Asghari
Moghadam,
M.,
&
Najarian,
B.
(2002).
Psychology
of
pain.
Tehran:
Roshd
Pub.
6.
Bair,
M.
J.,
Robinson,
R.
L.,
Katon,
W.,
&
Kroenke,
K.
(2003).
Depression
and
pain
comorbidity:
a
literature
review.
Archives
of
internal
medicine,
163(20),
2433-2445.
doi:
http://dx.doi.org/10.1001/archinte.163.20.2433
7.
Bair,
M.
J.,
Wu,
J.,
Damush,
T.
M.,
Sutherland,
J.
M.,
&
Kroenke,
K.
(2008).
Association
of
depression
and
anxiety
alone
and
in
combination
with
chronic
musculoskeletal
pain
in
primary
care
patients.
Psychosomatic
medicine,
70(8),
890.
doi:
http://dx.doi.org/10.1097/PSY.0b013e318185c510
8.
Bigal,
M.
E.,
Tsang,
A.,
Loder,
E.,
Serrano,
D.,
Reed,
M.
L.,
&
Lipton,
R.
B.
(2007).
Body
mass
index
and
episodic
headaches:
a
population-based
study.
Archives
of
internal
medicine,
167(18),
1964-1970.
doi:
http://dx.doi.org/10.1001/archinte.167.18.1964
9.
Büssing,
A.,
Ostermann,
T.,
Neugebauer,
E.
A.,
&
Heusser,
P.
(2010).
Adaptive
coping
strategies
in
patients
with
chronic
pain
conditions
and
their
interpretation
of
disease.
BMC
Public
Health,
10(1),
507.
doi:
10.1186/1471-2458-10-507
10.
Cooper,
C.,
Katona,
C.,
Orrell,
M.,
&
Livingston,
G.
(2006).
Coping
strategies
and
anxiety
in
caregivers
of
people
with
Alzheimer’s
disease:
the
LASER-AD
study.
Journal
of
affective
disorders,
90(1),
15-20.
11.
Deere,
K.
C.,
Clinch,
J.,
Holliday,
K.,
McBeth,
J.,
Crawley,
E.
M.,
Sayers,
A.,
.
.
.
Tobias,
J.
H.
(2012).
Obesity
is
a
risk
factor
for
musculoskeletal
pain
in
adolescents:
findings
from
a
population-based
cohort.
PAIN®,
153(9),
1932-1938.
doi:
http://dx.doi.org/10.1016/j.pain.2012.06.006
12.
DeGood,
D.,
&
Tait,
R.
(2011).
Assessment
of
pain
beliefs
and
pain
coping.
In
Turk
DC
Melzack
R
(Ed.),
Handbook
of
pain
assessment
(pp.
320–334).
New
York:
Guilford
Press.
13.
Folkman,
S.,
Lazarus,
R.
S.,
Dunkel-Schetter,
C.,
DeLongis,
A.,
&
Gruen,
R.
J.
(1986).
Dynamics
of
a
stressful
encounter:
cognitive
appraisal,
coping,
and
encounter
outcomes.
Journal
of
personality
and
social
psychology,
50(5),
992-1003.
doi:
http://dx.doi.org/10.1037/0022-3514.50.5.992
14.
Geisser,
M.
E.,
Robinson,
M.
E.,
&
Riley,
J.
L.
(2000).
Pain
beliefs,
coping,
and
adjustment
to
chronic
pain:
let’s
focus
more
on
the
negative.
Paper
presented
at
the
Pain
Forum.
15.
Greenberg,
P.
E.,
Sisitsky,
T.,
Kessler,
R.
C.,
Finkelstein,
S.
N.,
Berndt,
E.
R.,
Davidson,
J.
R.,
&
Fyer,
A.
J.
(1999).
The
economic
burden
of
anxiety
disorders
in
the
1990s.
The
Journal
of
clinical
psychiatry,
60(7),
427-435.
doi:
http://dx.doi.org/10.4088/JCP.v60n0702
16.
Greisen,
J.,
Juhl,
C.
B.,
Grøfte,
T.,
Vilstrup,
H.,
Jensen,
T.
S.,
&
Schmitz,
O.
(2001).
Acute
pain
induces
insulin
resistance
in
humans.
The
Journal
of
the
American
Society
of
Anesthesiologists,
95(3),
578-584.
doi:
http://dx.doi.org/10.1097/00000542-200109000-00007
17.
Holahan,
C.
J.,
Moos,
R.
H.,
Holahan,
C.
K.,
Brennan,
P.
L.,
&
Schutte,
K.
K.
(2005).
Stress
generation,
avoidance
coping,
and
depressive
symptoms:
a
10-year
model.
Journal
of
consulting
and
clinical
psychology,
73(4),
658.
doi:
http://dx.doi.org/10.1037/0022-006X.73.4.658
18.
Institute
of
Medicine.
(
2011).
Relieving
pain
in
America:
a
blueprint
for
transforming
prevention,
care,
education,
and
research.
Washington,
DC:
National
Academies
Press.
19.
Jensen,
M.
P.,
Turner,
J.
A.,
&
Romano,
J.
M.
(2007).
Changes
after
multidisciplinary
pain
treatment
in
patient
pain
beliefs
and
coping
are
associated
with
concurrent
changes
in
patient
functioning.
Pain,
131(1),
38-47.
20.
Jensen,
M.
P.,
Turner,
J.
A.,
Romano,
J.
M.,
&
Nielson,
W.
(2008).
Chronic
pain
coping
inventory
professional
manual.
Lutz:
FL:
Psychological
Assessment
Resources.
21.
Kelly,
T.,
Yang,
W.,
Chen,
C.-S.,
Reynolds,
K.,
&
He,
J.
(2008).
Global
burden
of
obesity
in
2005
and
projections
to
2030.
International
journal
of
obesity,
32(9),
1431-1437.
doi:
http://dx.doi.org/10.1038/ijo.2008.102
22.
Kessler,
R.
C.,
Berglund,
P.,
Demler,
O.,
Jin,
R.,
Koretz,
D.,
Merikangas,
K.
R.,
.
.
.
Wang,
P.
S.
(2003).
The
epidemiology
of
major
depressive
disorder:
results
from
the
National
Comorbidity
Survey
Replication
(NCS-R).
Jama,
289(23),
3095-3105.
doi:
http://dx.doi.org/10.1001/jama.289.23.3095
23.
Kroenke,
K.
(2003).
Patients
presenting
with
somatic
complaints:
epidemiology,
psychiatric
co-morbidity
and
management.
International
journal
of
methods
in
psychiatric
research,
12(1),
34-43.
doi:
http://dx.doi.org/10.1002/mpr.140
24.
Kroenke,
K.,
&
Price,
R.
K.
(1993).
Symptoms
in
the
community:
prevalence,
classification,
and
psychiatric
comorbidity.
Archives
of
internal
medicine,
153(21),
2474-2480.
doi:
http://dx.doi.org/10.1001/archinte.1993.00410210102011
25.
Lann,
D.,
&
LeRoith,
D.
(2007).
Insulin
resistance
as
the
underlying
cause
for
the
metabolic
syndrome.
Medical
Clinics
of
North
America,
91(6),
1063-1077.
doi:
http://dx.doi.org/10.1016/j.mcna.2007.06.012
26.
Lazarus,
R.
S.,
&
Folkman,
S.
(1984).
Stress,
appraisal,
and
coping.
New
York:
Springer.
27.
Lee,
I.-T.,
Lee,
W.-J.,
Huang,
C.-N.,
&
Sheu,
W.
H.
(2007).
The
association
of
low-grade
inflammation,
urinary
albumin,
and
insulin
resistance
with
metabolic
syndrome
in
nondiabetic
Taiwanese.
Metabolism,
56(12),
1708-1713.
doi:
http://dx.doi.org/10.1016/j.metabol.2007.07.015
28.
Loevinger,
B.
L.,
Muller,
D.,
Alonso,
C.,
&
Coe,
C.
L.
(2007).
Metabolic
syndrome
in
women
with
chronic
pain.
Metabolism,
56(1),
87-93.
doi:
http://dx.doi.org/10.1016/j.metabol.2006.09.001
29.
Luppino,
F.
S.,
de
Wit,
L.
M.,
Bouvy,
P.
F.,
Stijnen,
T.,
Cuijpers,
P.,
Penninx,
B.
W.,
&
Zitman,
F.
G.
(2010).
Overweight,
obesity,
and
depression:
a
systematic
review
and
meta-analysis
of
longitudinal
studies.
Archives
of
general
psychiatry,
67(3),
220-229.
doi:
http://dx.doi.org/10.1001/archgenpsychiatry.2010.2
30.
Marcus,
D.
A.
(2004).
Obesity
and
the
impact
of
chronic
pain.
The
Clinical
journal
of
pain,
20(3),
186-191.
doi:
http://dx.doi.org/10.1097/00002508-200405000-00009
31.
McWilliams,
L.
A.,
Cox,
B.
J.,
&
Enns,
M.
W.
(2003).
Mood
and
anxiety
disorders
associated
with
chronic
pain:
an
examination
in
a
nationally
representative
sample.
Pain,
106(1),
127-133.
doi:
http://dx.doi.org/10.1016/S0304-3959(03)00301-4
32.
Miscio,
G.,
Guastamacchia,
G.,
Brunani,
A.,
Priano,
L.,
Baudo,
S.,
&
Mauro,
A.
(2005).
Obesity
and
peripheral
neuropathy
risk:
a
dangerous
liaison.
Journal
of
the
peripheral
nervous
system,
10(4),
354-358.
doi:
http://dx.doi.org/10.1111/j.1085-9489.2005.00047.x
33.
Müller-Riemenschneider,
F.,
Reinhold,
T.,
Berghöfer,
A.,
&
Willich,
S.
N.
(2008).
Health-economic
burden
of
obesity
in
Europe.
European
journal
of
epidemiology,
23(8),
499-509.
doi:
http://dx.doi.org/10.1007/s10654-008-9239-1
34.
Pi-Sunyer,
X.
(2009).
The
medical
risks
of
obesity.
Postgraduate
Medicine,
121(6),
21-33.
doi:
http://dx.doi.org/10.3810/pgm.2009.11.2074
35.
Räikkönen,
K.,
Matthews,
K.
A.,
&
Kuller,
L.
H.
(2007).
Depressive
symptoms
and
stressful
life
events
predict
metabolic
syndrome
among
middle-aged
women
a
comparison
of
World
Health
Organization,
Adult
Treatment
Panel
III,
and
International
Diabetes
Foundation
definitions.
Diabetes
care,
30(4),
872-877.
doi:
http://dx.doi.org/10.2337/dc06-1857
36.
Rajabi
Damavandi,
G.,
Poushne,
K.,
&
Ghobari
Banab,
B.
(2009).
[Relationship
between
personality
characteristics
and
coping
strategies
in
parents
Children
with
autism
spectrum
disorders]
[Persian].
Research
on
Exceptional
Children,
9(2),
133-144.
37.
Ray,
L.,
Lipton,
R.
B.,
Zimmerman,
M.
E.,
Katz,
M.
J.,
&
Derby,
C.
A.
(2011).
Mechanisms
of
association
between
obesity
and
chronic
pain
in
the
elderly.
Pain,
152(1),
53-59.
doi:
10.1016/j.pain.2010.08.043
38.
Rossi,
H.
L.,
Luu,
A.
K.
S.,
DeVilbiss,
J.
L.,
&
Recober,
A.
(2013).
“Obesity
increases
nociceptive
activation
of
the
trigeminal
system”.
European
journal
of
pain
(London,
England),
17(5),
649-653.
doi:
10.1002/j.1532-2149.2012.00230.x
39.
Sadeghi,
H.
S.,
&
Niknam,
M.
(2015).
The
Relationship
between
Coping
Skills
with
Social
Maturity
and
Adjustment
of
Female
First
Graders
in
High
School:
A
Case
Study
in
Iran.
Asian
Social
Science,
11(25),
144.
40.
Snow,
D.
L.,
Swan,
S.
C.,
Raghavan,
C.,
Connell,
C.
M.,
&
Klein,
I.
(2003).
The
relationship
of
work
stressors,
coping
and
social
support
to
psychological
symptoms
among
female
secretarial
employees.
Work
&
Stress,
17(3),
241-263.
41.
Medical
care,
43(12),
1164-1170.
doi:
http://dx.doi.org/10.1097/01.mlr.0000185750.18119.fd
42.
Tan,
G.,
Teo,
I.,
Anderson,
K.
O.,
&
Jensen,
M.
P.
(2011).
Adaptive
versus
maladaptive
coping
and
beliefs
and
their
relation
to
chronic
pain
adjustment.
The
Clinical
journal
of
pain,
27(9),
769-774.
doi:
http://dx.doi.org/10.1097/AJP.0b013e31821d8f5a
43.
Tietjen,
G.
E.,
Peterlin,
B.
L.,
Brandes,
J.
L.,
Hafeez,
F.,
Hutchinson,
S.,
Martin,
V.
T.,
.
Herial,
N.
A.
(2007).
Depression
and
anxiety:
effect
on
the
migraine–obesity
relationship.
Headache:
The
Journal
of
Head
and
Face
Pain,
47(6),
866-875.
doi:
http://dx.doi.org/10.1111/j.1526-4610.2007.00810.x
44.
van
Berkel,
J.,
Boot,
C.
R.,
Proper,
K.
I.,
Bongers,
P.
M.,
&
van
der
Beek,
A.
J.
(2014).
Effectiveness
of
a
worksite
mindfulness-related
multi-component
health
promotion
intervention
on
work
engagement
and
mental
health:
results
of
a
randomized
controlled
trial.
PloS
one,
9(1),
e84118.
doi:
http://dx.doi.org/10.1371/journal.pone.0084118
|

