|
The comparison of quality
of life, self-efficacy and resiliency in infertile
and fertile women
Mahya Shamsi Sani (1)
Mohammadreza Tamannaeifar (2)
(1) MA
Student of Psychology, Department of Psychology,
Islamic Azad University- Kashan Branch, Kashan,
Iran
(2)Associate Professor of Psychology, Department
of Psychology, University of Kashan, Kashan,
Iran
Correspondence:
Mohammadreza
Tamannaeifar
Associate Professor of Psychology,
Department of Psychology,
University of Kashan,
Kashan, Iran
Email:
tamannai@kashanu.ac.ir
|
Abstract
Background:
Pregnancy and infertility are important
life events that are associated with specific
psychosocial aspects, and infertility
is usually regarded as a stressful and
threatening event that is influenced by
psychological factors.
Objective:
The purpose of this study was to evaluate
and compare the quality of life, self-efficacy
and resiliency in infertile and fertile
women.
Method: This
causal comparative study, included all
fertile and infertile women referred to
Arash Hospital and Mirza Kuchak Khan Hospital
in Tehran; 60 infertile women and 60 fertile
women were selected using convenience
sampling method. To collect data, the
quality of life questionnaire (WHOQOL-BREF),
Sherer’s self-efficacy Questionnaire,
and Conner and Davidson’s Resilience
Questionnaire were used. Descriptive statistics
(mean and standard deviation) and inferential
statistics (correlation test and regression
analysis) were used to analyze the data.
Results:
The results showed that mean (standard
deviation) of quality of life, self-efficacy
and resiliency in fertile women was 86.62
(11.162), 64.40 (9.048), and 71.40 (11.640),
respectively. The mean (standard deviation)
of quality of life, self-efficacy and
resiliency for fertile women was 79.13
(10.829), 58.05 (7.688), and 66.92 (10.339),
respectively. The results of t-test showed
that between fertile and infertile women,
in terms of quality of life, self-efficacy
and resiliency there is a significant
difference.
Discussion and Conclusion: The results
showed that the level of quality of life,
self-efficacy and resiliency in infertile
women is less than in fertile women. Based
on these results, it can be said that
considering the importance of psychological
factors in exacerbating the physical and
mental damage associated with infertility,
psychological interventions focused on
quality of life, self-efficacy and resiliency
with the aim of improving the mental health
of the infertile people, is necessary.
Key words: Fertility,
Infertility, Quality of Life, Self-efficacy,
Resiliency
|
In many countries of the world, including Iran,
pregnancy and having a child are generally a
positive and welcome event and an important
factor in gaining social status and strength
of marital life, and infertility is often a
great stigma, leading to psychological and social
harm. Infertility is defined as lack of pregnancy
following one year of intercourse without the
use of contraceptive methods (Richard et al.,
2014). The World Health Organization (WHO, 2004)
estimates that 60-80 million couples experience
infertility around the world. In recent years,
infertility has risen (Jisha & Thomas, 2016).
In this way, it is estimated that in the world,
8-15 percent of couples may experience infertility
(El Kissi et al., 2013). The prevalence of primary
infertility in Iran was reported at 24.9% in
2004 (Vahidi et al., 2004; quoted by Jamshidimanesh
et al., 2015). Infertility is considered one
of the most important stressful events in life
and a negative event for couples, which causes
interpersonal distress in marital relationships
(Rashidi et al., 2008; El Kissi et al. 2013),
a serious threat to marriage and the continuation
of marital life (Khetarpal &Colleagues,
2012), and in some cases, separates couples
(Galhardo et al., 2011).
It seems that the impact of infertility is
not limited to marital and sexual relationships,
but it affects all dimensions of the individual’s
life and its effects are imposed on other psychosocial
aspects of the infertile people (Chachamovich
et al., 2010). Psychological problems are the
consequences of infertility (Cwikle, Gidron
& Sheiner, 2004). Research on the consequences
of infertility has shown that infertility causes
emotional disturbances in both women and men
and their spouses (Greil, et al., 2011; Faramarzi
et al., 2013; Takaki & Hibino, 2014). Infertility
is linked to the prevalence of psychological
and psychiatric problems, and numerous studies
have reported the prevalence of these problems
in infertile couples (De Berardis et al., 2014).
Anxiety, depression and other psychiatric disorders
are reported in couples and people with infertility,
and studies report the prevalence of psychiatric
problems from 6 to 68 percent (Sule, Gupte &
De Sousa, 2017).
In several studies, it has been shown that
infertility leads to reduced mental (subjective)
well-being (Tovliat & Tamannaeifar, 2015),
reduced mental health and marital adjustment
(Tamannaeifar, 2011), decreased quality of life
(Xiaoli et al., 2016; Chachamovich et al. 2010;
Lau et al, 2008), decreased sexual function
(Hassanin et al., 2010; Monga et al., 2004),
anxiety, depression and decreased quality of
marital life (Matsubayashi et al., 2004), feeling
of helplessness and experience of negative emotions
(Chandra et al., 2014).
Infertility due to its unfortunate consequences
affects people’s attitudes about themselves,
toward life and the quality of life (Chachamovich
et al., 2010) and causes a loss in quality of
life (Hassanin et al., 2010; Drosdzol&Skrzypulec,
2008).
Quality of life is one of the most important
health components that has received considerable
attention in recent years. The concept of quality
of life has been defined in various ways. The
World Health Organization (WHO) defines quality
of life as “the individual’s perception
of one’s position in life, according to
the cultural context and the value system of
the community in which he/she lives,” and
considers this concept as a combination of physical
health, state of Psychological health, level
of independence, social relations, individual
beliefs of these factors with environmental
characteristics (Ghafari et al., 2012). Several
studies have shown that quality of life in infertile
women is lower than that of fertile women (Trent
et al., 2002; Coffey, Bano & Mason, 2006;
Nilfrooshan et al., 2006). It has been shown
that the quality of life in infertile people
with mental disorders is lower (Van der Akker,
2005; Chachamovich et al., 2010). It has been
widely demonstrated that clinical symptoms of
depression are related to the outcomes of quality
of life (Schweikert et al., 2008; Ohaeri, Awadalla,
& Gado, 2009).
Some studies have shown that demographic variables
such as age, educational level, weak marital
relationships, and the length of lifetime attempts
to treat infertility are predictive of the quality
of life in infertile people (Fekkes et al.,
2003; Ragni et al., 2005; Lau et al. 2008).
The study of Chachamovich et al. (2010) has
shown that anxiety and depression are associated
with a low level of quality of life in the infertile
and the effect of depression is greater than
anxiety and other clinical variables and socio-demographic
factors.
Although numerous studies have shown the negative
effect of infertility on the quality of life
in infertile women (Fekkes et al., 2003), some
studies have reported that there is no difference
in the quality of life of the infertile population
compared to the healthy population (Hearn et
al., 1987). Even some studies have shown that
quality of life and marital adjustment of infertile
women are higher than fertile women (Onat&Beji,
2012). The attitude towards women’s infertility
is often influenced by racial differences and
religion and culture undoubtedly affect quality
of life in some aspects, such as infertility
(Inhorn& Buss, 1994).
Another factor that has been addressed in women’s
infertility is self-efficacy of infertile people.
In the case of infertile people, self-efficacy
is the perception of patients of their ability
to use cognitive skills to control emotions.
An infertile person with high self-efficacy
has more emotional (affective) stability and
more insistence on treatment (Cousineau et al.,
2006). Self-efficacy is an indicator of the
individual’s ability to use stress coping
skills and the use of personal resources necessary
to meet situational demands. There is some evidence
that self-efficacy plays a role in managing
illness, symptoms, and functional limitations
(Banik et al., 2017). Hence, infertile people
with high self-efficacy can maintain calmness.
High self-efficacy enhances health behaviors
and improves health status, and may even lead
to an increased probability of pregnancy (Cousineau
et al., 2006). Jamshidimanesh et al. (2015)
showed that self-efficacy training for infertile
women had a positive effect and training programs
that include familiarity with the reproductive
system, definition of infertility, prevalence,
causes, diagnostic methods, treatment protocol,
and the necessary tests will increase the self-efficacy
of infertile women. Sami and Tazeen (2012) reported
that the increase in infertile women’s
information about the causes and treatments
of infertility and ways to reduce stress and
self-efficacy training can have positive effects
and will lead to better healthcare of infertility
and to avoid traditional and insecure methods.
Considering that studies have shown that infertility
is associated with a lot of stress, the issue
of resiliency has also been of particular importance,
because resiliency is considered as one of the
personality traits that play a protective role
against life-threatening factors including diseases.
Resiliency is the process or ability to adapt
to the challenges and threats of life and to
overcome them (Newman, 2003). Resiliency is
the ability to resist against difficult living
conditions and a dynamic process in adapting
to important disasters; therefore, resiliency
is considered as a positive symmetry of vulnerability
(Herrmann et al., 2011). Resiliency focuses
on groups exposed to risk factors, but who are
faced with few negative consequences and may
even have positive outcomes (Tiet& Huizinga,
2002).
Studies have shown that infertile people’s
resiliency is less than fertile people (Sexton,
Byrd & Kluge, 2010; Kagan et al., 2011;
Lee et al., 2012). Rezaie et al’s (2013)
study showed that with increasing resiliency,
patients are helped to better deal with harsh
conditions. A study conducted by Lee et al.
(2012) shows that resiliency can lead to optimism,
spirituality, psychic calm and an increase in
the quality of life of infertile women. Abbasi
et al. (2014) showed that considering the fact
that resiliency causes people to reasonably
and positively deal with life stresses, they
can positively evaluate life events. Therefore,
low levels of resiliency in infertile women
can reduce their psychological well-being.
Researchers believe that infertility is a life
crisis for the couples involved, and others
consider it as the most stressful event after
a divorce and the death of a dear one (Herrmann
et al., 2011). Even if most couples with infertility
show that infertility does not have a long-term
effect on their life satisfaction, at the time
of diagnosis and subsequent treatment, the level
of satisfaction is reduced (Verhaak et al.,
2007) and can affect many aspects of life including
the quality of life. Therefore, the present
study was conducted to compare the quality of
life, self-efficacy and resiliency in infertile
and fertile women.
This study is a causal comparative study. The
statistical population of this study consisted
of all fertile and infertile women referring
to Arash Hospital and Mirza Kuchak Khan Hospital
in Tehran. 60 infertile women and 60 fertile
women were selected using convenience sampling
method. After expressing the research aim for
the subjects, they were asked to respond to
the questionnaires if they wished. Subjects
were told that the data of the questionnaires
were completely confidential. To collect data,
Quality of Life Inventory (WHOQOL-BREF), Sherer’s
Self- efficacy Questionnaire, and Connor &
Davidson’s Resilience Questionnaire were
used.
Quality of life questionnaire
The Quality of Life Questionnaire (WHOQOL-BREF)
assesses the quality of life totally and in
general, and has four areas of physical health,
mental health, social relationships and environmental
health. This questionnaire has 24 questions,
each of the areas has 3. 6, 7 and 8 questions,
respectively. The questionnaire has two other
questions that do not belong to any of the areas
and that generally assess health status and
quality of life. Nejat et al. (2006) have reported
the reliability of this scale by Cronbach’s
alpha method in areas of physical, psychological,
social and environmental health, respectively,
0.70, 0.73, 0.55 and 0.84, and after two weeks
using test-retest method a coefficient of 0.70.
In the study of Kiaei et al. (2016), Cronbach’s
alpha in all areas was above 0.70 and only in
the social relationships was 0.55.
Self-efficacy questionnaire
Sherer’s Self- efficacy Questionnaire has
17 items. Sherer (1982) argues that this questionnaire
measures three aspects of behavior, including
the desire to initiate behavior, the desire
to expand efforts to complete a task and being
different in confronting obstacles. The scoring
of this scale is on a Likert scale from absolutely
disagree (1) to absolutely agree (5). Sherer
(1982) reported the Cronbach’s alpha of
this scale 0.76. In the study of Behrozian et
al. (2013), the coefficient of reliability of
this test was 0.80.
Resilience questionnaire
This questionnaire was developed by Connor and
Davidson (2003) to measure the power of coping
with stress and threat, and has 25 questions.
This questionnaire is scored on the Likert scale
from zero (completely false) to 4 (completely
true). The average score of this scale is 25,
and the higher score indicates the more resiliency.
In the research by Samani, Jokar and Sahragard
(2006), the reliability of this tool using Cronbach’s
alpha coefficient was reported to be 0.87. In
another study by Bavali et al. (2013), Cronbach’s
alpha coefficient was 0.83.
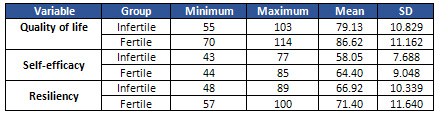
Table 1 shows the mean and standard deviation
of quality of life, self-efficacy and resiliency
in infertile and fertile women, and tables 2,
3 and 4 show the results of t-tests.
Data in Table 1 show that the mean (SD) of
quality of life, self-efficacy and resiliency
in fertile women are 86.62 (11.162), 64.40 (9.048),
and 71.40 (11.640), respectively. The mean (standard
deviation) of quality of life, self-efficacy
and resiliency for infertile women are 79.13
(10.829), 58.05 (7.688), and 66.92 (10.339),
respectively.
Table 1: Mean and standard deviation of quality
of life, self-efficacy and resiliency in infertile
and fertile women
Click here for Table
2: T-test results for comparing infertile and
fertile women in the quality of life variable
Click here for Table
3: T-test results for comparing infertile and
fertile women in the self-efficacy variable
Click here for Table
4: T-test results for comparing infertile and
fertile women in the resiliency variable
Data from Tables 2, 3 and 4 show that there
is a significant difference between infertile
and fertile women in terms of quality of life,
self-efficacy and resiliency, and the level
of quality of life, self-efficacy and resiliency
in infertile women is lower.
|
DISCUSSION
AND
CONCLUSION
|
Infertility
is
not
just
a
gynecological
illness,
but
also
a
bio-psycho-social
problem
that
includes
psychiatric
problems,
reduced
quality
of
life,
marital
conflicts
and
sexual
disturbances
(Onat
&
Beji
2012).
Therefore,
the
present
study
aimed
to
compare
the
quality
of
life,
self-efficacy
and
resiliency
in
infertile
and
fertile
women.
The
present
study
showed
that
quality
of
life
in
infertile
women
is
lower
than
in
fertile
women.
This
finding
is
in
line
with
the
results
of
the
research
by
Xiaoli
and
others
(2016),
Chachamovich
et
al.
(2010),
Drosdzol
and
Skrzypulec
(2008),
Lau
et
al.
(2008),
Fekkes
et
al.
(2003)
and
Alami
et
al.
(2009).
In
explaining
the
difference
in
the
quality
of
life
of
infertile
women
and
fertile
women,
it
can
be
said
that
the
quality
of
life
in
infertile
women
is
related
to
the
amount
of
pressure
of
people
around
for
giving
birth,
the
intensity
of
desire
for
having
a
child,
the
burden
of
infertility
treatment
costs,
an
individual’s
assessment
of
the
household’s
economic
situation
and
irrational
thoughts
related
to
having
a
child
and
the
duration
and
cause
of
infertility.
Infertile
women
also
suffer
more
stress
and
with
increasing
stress,
their
therapeutic
response
decreases
and
leads
to
a
decline
in
quality
of
life.
Attitudes
toward
the
issue
of
women’s
infertility
are
often
affected
by
racial
and
cultural
differences,
and
on
this
basis,
culture
affects
the
quality
of
life
of
the
infertile
people
(Inhorn
&
Buss,
1994).
Because
of
the
problems
and
consequences
of
infertility
and
a
decrease
in
quality
of
life,
most
researchers
state
that
the
primary
objective
of
psychosocial
counseling
should
be
the
promotion
of
the
quality
of
life
in
infertile
people,
regardless
of
their
wish
to
have
a
child
is
fulfilled
or
not
(Van
den
Broeck
et
al.,
2010).
Another
result
of
this
study
was
that
self-efficacy
in
infertile
women
is
weaker
than
in
fertile
women.
This
finding
is
in
line
with
the
results
of
research
by
Pahlavani
et
al.
(2002),
Alizadeh
et
al.
(2005),
Nene,
Coyaji
and
Apte
(2009)
and
Faramarzi
et
al.
(2014).
It
has
been
reported
that
self-efficacy
plays
a
role
in
predicting
health
behaviors
and
quality
of
life.
When
dealing
with
a
chronic
disease,
it
is
necessary
to
carry
out
behaviors
and
activities
that
reduce
the
effect
of
the
disease
on
the
quality
of
life;
self-efficacy
can
play
an
important
role
in
this
regard
and
affect
the
physical,
emotional
and
social
dimensions
of
quality
of
life
(Cramm
et
al.
,
2013).
A
study
by
Van
der
Slot
et
al.
(2010)
showed
that
high
levels
of
self-efficacy
in
patients
are
associated
with
their
better
quality
of
life.
Self-efficacy
contributes
to
individual
adaptation
to
symptoms
of
illness,
and
one’s
beliefs
about
controlling
disease
and
dealing
with
it,
prevent
quality
of
life
from
being
reduced
(Motl
&
Snook,
2008).
People
who
see
themselves
as
inefficient
individuals
avoid
difficult
assignments
and
suffer
when
faced
with
discomfort.
Therefore,
self-efficacy
is
critical
to
understanding
the
health
status
and
quality
of
life.
Hence,
patients
with
higher
self-efficacy
report
fewer
effects
of
illnesses
and
better
quality
of
life
(Astrid
et
al.,
2005).
Jamshidimanesh
et
al.
(2015)
found
that
self-efficacy
training
for
infertile
women
had
a
positive
effect,
and
a
training
program
that
included
familiarity
with
the
reproductive
system,
definition
of
infertility,
prevalence,
causes,
diagnostic
methods,
treatment
protocol,
necessary
tests,
and
fertility
methods,
enhances
the
self-efficacy
of
infertile
women.
People
who
have
high
self-efficacy
take
part
in
the
health
care
program,
and
participation
in
these
programs
increases
the
quality
of
life
of
patients
(Rafii,
Naseh
&
Yadegary,
2012).
Also,
the
present
study
showed
that
the
resiliency
level
in
infertile
women
is
lower
than
in
fertile
women.
Some
other
studies
have
also
shown
that
the
resiliency
rate
in
infertile
people
is
lower
than
in
fertile
individuals
(Sexton,
Byrd
&
Kluge,
2010;
Kagan
et
al.,
2011;
Lee
et
al.,
2012).
Infertility
causes
tension
in
infertile
women
reduces
self-esteem,
physical
health
and
increases
depression,
stress
and
anxiety
(Greil,
Slauson-Blevins
&
McQuillan,
2010)
and
by
reducing
an
individual’s
coping
resources
leads
to
low
levels
of
resiliency
(Jebraeili,
Hashemi,
&
Nazemi
,
2016).
The
study
by
Sexton,
Byrd
&
Kluge
(2010)
showed
that
infertility
reduces
people’s
resistance
to
life
problems,
such
that
these
people
have
less
hardiness
and
resilience
facing
problems
compared
to
other
people.
Resiliency,
on
the
other
hand,
causes
a
logical
and
positive
coping
with
the
stresses
and
leads
to
a
positive
reassessment
of
events
(Abbasi
et
al.,
2014).
Resilient
people
have
self-esteem,
self-efficacy,
problem-solving
skills,
and
satisfactory
interpersonal
relationships
(Wagnild
&
Young,
1993).
If
we
transfer
this
concept
into
infertile
patients,
it
means
that
these
patients
have
a
good
quality
of
life
despite
the
fact
that
infertility
has
severe
stress
for
them
(Ridenour,
Yorgason
&
Peterson,
2009).
According
to
the
findings
of
this
research
and
previous
studies,
it
can
be
said
that
infertility
as
a
gynecologic
illness
is
associated
with
negative
consequences
such
as
psychopathology,
loss
of
quality
of
life
and
marital
dissatisfaction.
Therefore,
in
addition
to
the
medical
treatment
process,
psychological
interventions
aimed
at
improving
the
mental
health
of
infertile
women
is
necessary.
1.
Abbasi,
M.,
Dargahi,
SH.,
Jabraeili,
H.,
Ghasemi
Jobaneh,
R.,
&
Dargahi,
A.
(2014).
Role
of
meta
emotion
and
resiliency
in
psychological
the
well-being
of
infertile
women
of
Gonabad
City
in
2012-
2013.
Community
Health
journal,
8(1),
9-17.
2.
Alami,
M.,
Amanati,
L.,
Shokrabi,
SH.,
Haghani,
H.,
&Ramezanzadeh,
F.
(2009).
Factors
influencing
quality
of
life
among
infertile
women.
IJN.
21
(56),
27-35.
3.
Alizadeh,
T.,
Farahani,
M.N.,
Shahraray,
M.
&Alizadegan,
Sh.
(2005)
The
relationship
between
self-esteem
and
locus
of
control
with
infertility
related
stress
of
no
related
infertile
men
and
women.
Medical
Journal
of
Reproduction&
Infertility,
6(22),
194-204.
4.
Astrid,
K.,
Wahl,
A.
K.,
Rustoen,
T.,
Hanestad,
B.R.,
Gjengedal,
E.,
&
Moum,
T.
(2005).
Self-efficacy,
pulmonary
function,
perceived
health
and
global
quality
of
life
of
cystic
fibrosis
patients,
Social
Indicators
Research,
72,
239–261.
5.
Banik,
A.,
Luszczynska,
A.,
Pawlowska,
I.,
Cieslak,
R.,
Knoll,
N.,
&
Scholz,
U.
(2017).
Enabling,
not
cultivating:
received
social
support
and
self-efficacy
explain
quality
of
life
after
lung
cancer
surgery,
Annals
of
Behavioural
Medicine,
51(1),
1-12.
6.
Bavali,
F.,
Faramarzi,
S.,
Manshaie,
GH.,
&Khaledian,
M.
(
2013).
Effectiveness
of
group
logo
therapy
on
promotion
of
resiliency
of
the
mothers
with
intellectual
disability
children.
World
of
Sciences
Journal,
1(7),
115-
23.
7.
Behrozian,
S.,
&Ahmadi,
E.
(2013).
The
assessment
of
self-efficacy
and
the
dimension
of
quality
of
life
on
smokers
and
non-smokers.
The
Journal
of
Urmia
University
of
Medical
Sciences,
24(4),
257-262.
8.
Chachamovich,
J.R,
Chachamovich,
E.,
Ezer,
H.,
Fleck,
M.P.,
Knauth,
D.,
&
Passos,
EP.
(2010).
Investigating
quality
of
life
and
health-related
quality
of
life
in
infertility:
a
systematic
review.
J
Psychosom
Obstet
Gynaecol.
31(2):101–10
9.
Chachamovich,
Juliana
LR.
Chachamovich,
E.,
Ezer,
H.,
Fernanda
P
Cordova,
F.P.,
Fleck,
M.P.,
Knauth,
D.R.,
&Passos,
E.P.
(2010).
Psychological
distress
as
predictor
of
quality
of
life
in
men
experiencing
infertility:
a
cross-sectional
survey,
Reproductive
Health,
7(3),
1-9.
10.
Chandra,
A.,
Copen,
C.
E.,
&Stephen,
E
.H.(2014).
Infertility
service
use
in
the
United
States:
data
from
the
national
survey
of
family
growth,
1982–2010,
National
Health
Statistics
Reports,
73(22),
1-21.
11.
Coffey,
S.,
Bano,
G.,
&
Mason,
H.D.
(2006).
Health-related
quality
of
life
in
women
with
polycystic
ovary
syndrome:
a
comparison
with
the
general
population
using
the
polycystic
ovary
syndrome
questionnaire
(PCOSQ)
and
the
Short
Form-
36
(SF-36),
Journal
Gynaecological
Endocrinology,
22(2),
80-86.
12.
Cousineau,
T.
M.,
Green,
T.
C.,
Corsini,
E.
A.,
Barnard,
T.,
Seibring,
A.
R,
&
Domar,
A.
D.
(2006).
Development
and
validation
of
the
infertility
self-efficacy
scale.
Fertility&
Sterility,
85(6),
1684-1696.
13.
Cramm,
J.M.,
Strating,
M.
M.
H.,
Roebroeck,
M.E.,
&
Nieboer,
A.P.
(2013).
The
importance
of
general
self-efficacy
for
the
quality
of
life
of
adolescents
with
chronic
conditions,
Soc
Indic
Res.
113,
551–561.
14.
Cwikle,
J.,
Gidron,
Y.,
&
Sheiner,
E.
(2004)
Psychological
interactions
with
infertility
among
women.
European
Journal
of
Obstetrics
and
Reproductive
Biology,
117(2),
126-131.
15.
De
Berardis,
D.,
Mazza,
M.,
Marini,
S,
Del
Nibletto,
L.,
Serroni,
N.,
Pino,
MC.
Valchera,
A.,
Ortolani,
C.,
Ciarrocchi,
F.,
Martinotti,
G.,
&
Di
Giannantonio,
M.
(2014).
Psychopathology,
emotional
aspects
and
psychological
counselling
in
infertility:
a
review.
Clin
Ter.
165(3):163–9.
16.
Drosdzol,
A.,
&
Skrzypulec,V.
(2008).
Quality
of
life
and
sexual
functioning
of
Polish
infertile
couples.
European
Journal
of
Contraception
and
Reproductive
Health
Care,
13(3),
271-281.
17.
El
Kissi,
Y.,
Romdhane,
A.B.,
Hidar,
S.,
Bannour,
S.,
Idrissi,
K.A.,
Khairi,
H.,
&Ali,
B.B.
(2013).
General
psychopathology,
anxiety,
depression
and
self-esteem
in
couples
undergoing
infertility
treatment:
a
comparative
study
between
men
and
women.
Eur
J
Obstet
Gynecol
Reprod
Biol.
167(2):185–9.
18.
Faramarzi.M.
Pasha,
H.,
Esmailzadeh,
S.,
Kheirkhah,
F.,
Hajian-ilaki,
K.,
&
Salmalian,
H.
(2014).
A
survey
of
correlation
infertility
self-efficacy
with
behavioural
health
scales
in
infertile
women,
Health,
6(10),
943-949.
19.
Faramarzi,
M.,
Pasha,
H.,
Esmailzadeh,
S.,
Kheirkhah,
F.,
Heidary,
S.,
&
Afshar,
Z.
(2013).
The
effect
of
the
cognitive
behavioural
therapy
and
pharmacotherapy
on
infertility
stress:
a
randomized
controlled
trial.
Int
J
FertilSteril,
7(3),
199-206.
20.
Fekkes,
M.,
Buitendijk,
S.E.,
Verrips,
G.H,
Braat
D,
D.,
Brewaeys,
A.M.,
Dolfing,
J.G.,
Kortman,
M.,
Leerentveld,
R.A.,
&
Macklon,
N.S.
(2003).
Health-related
quality
of
life
in
relation
to
gender
and
age
in
couples
planning
IVF
treatment.
Hum
Reprod,
18,
1536-1543.
21.
Galhardo,
A.,
Pinto-Gouveia,
J.,
Cunha,
M.,
&Matos,
M.
(2011).The
impact
of
shame
and
self-judgment
on
psychopathology
in
infertile
patients.
Hum
Reprod.
26(9):2408–14.
22.
Ghafari,
G.
H.,
Karimi,
A.,
&
Nozari,
H.
(2012).
Process
of
the
study
on
quality
of
life
in
Iran.
Journal
of
Social
Studies,
1(3),
107-134.
23.
Greil,
A,
L.,
McQuillan,
J.,
Lowry,
M.,
&
Shreffler,
KM.
(2011).
Infertility
treatment
and
fertility-specific
distress:
a
longitudinal
analysis
of
a
population-based
sample
of
US
women.
Soc
Sci
Med.
73(1):87–94.
24.
Greil,
A.L.,
Slauson-Blevins,
K.,
&
McQuillan,
J.
(2010).
The
experience
of
infertility:
A
review
of
recent
literature.
Social.
Health
Illn,
32(1),
140-162.
25.
Hassanin,
I,
M.
A.,
Abd-El-Raheem,
T.,
&
Shahin,
A.Y.
(2010).
Primary
infertility
and
health-related
quality
of
life
in
Upper
Egypt,
International
Journal
of
Gynaecology
and
Obstetrics,
110,
118–121.
26.
Hearn,
M.
T.,
Yuzpe,
A.
A.,
Brown,
S.
E.,
&
Casper,
R.
F.
(1987).
Psychological
characteristics
of
in
vitro
fertilization
participants.
Am
J
ObstetGynecol,
156(2),
269-274.
27.
Herrmann,
D.,
Scherg,
H.,
Verres,
R.,
Hagens,
C.,
Strowitzki,
T.,
&
Wischmann,
T.
(2011).
Resilience
in
infertile
couples
acts
as
a
protective
factor
against
infertility-specific
distress
and
impaired
quality
of
life,
J
Assist
ReprodGenet,
28,
1111–1117.
28.
Inhorn,
M.C.,
&
Buss,
K.A.
(1994).
Ethnography,
epidemiology
and
infertility
in
Egypt.
SocSci
Med,
39(5),
671-86.
29.
Jamshidimanesh,
M.,
Alimanesh,
N.,
Behbodi
Moghaddam,
Z.,
&
Haghani,
H.
(2015).
Effect
of
an
Educational
package
on
self-efficacy
of
infertile
women,
Journal
of
the
Iranian
Institute
for
Health
Sciences
Research,
2,
227-237.
30.
Jebraeili,
H.,
Hashemi,
J.,
&
Nazemi,A.(2016).
Comparative
study
of
resiliency,
meta
emotions
and
psychological
well-being
in
fertile-infertile
women,
Fundamentals
of
Mental
Health,
18(5),
259-264.
31.
Jisha,
P,
R.,
&
Thomas,
I.(2016).
Quality
of
life
and
infertility:
influence
of
gender,
years
of
marital
life,
resilience,
and
anxiety,
Psychol
Stud.
DOI
10.1007/s12646-016-0358-6.
32.
Kagan,
L.,
Psaros,
C.,
Alert,
M.D.,
Styer,
A.K.,
Shifren,
J.L.,
&
Park,
E.R.
(2011).
Improving
resilience
among
infertile
women:
a
pilot
study.
Fertil
Steril,
96(3),
151.
33.
Khayata,
GM.,
Rizk,
DE.,
Hasan,
MY.,
Ghazal-Aswad,
S.,
&Asaad,
M.A.
(2003).
Factors
influencing
the
quality
of
life
of
infertile
women
in
United
Arab
Emirates.
Int
J
GynaecolObstet,
80(2),
183-8.
34.
Khetarpal,
A.,
&
Singh,
S.
(2012).
Infertility:
why
can’t
we
classify
this
inability
as
disability?
Australian
Medical
Journal,
5(6),
334-
339.
35.
Kiaei,
MZ,
Ferdosi,
M.,
Moradi,
R.,
Chelongar,
Q.,
Ahmadzadeh,
M.S.,
&
Bahmanziari,
N.
(2016).
Association
of
self-efficacy
and
quality
of
life
in
women
with
breast
cancer
undergoing
chemotherapy.
J
Qazvin
Univ
Med
Sci,
20
(2),
58-65.
36.
Lau,
J.T.,
Wang,
Q.,
Cheng,
Y.,
Kim,
J.H.,
Yang,
X.,
&Tsui,
H.Y.
(2008).
Infertility-related
perceptions
and
responses
and
their
associations
with
quality
of
life
among
rural
Chinese
infertile
couples.
J
Sex
Marital
Ther,
34,
248-267.
37.
Lee,
G.L.,
Blyth,
ED.,
&
Lai-Wan
Chan,
C.
(2012).
Understanding
the
patterns
of
adjustment
to
infertility
of
IVF
users
using
narrative
and
autobiographical
timeline.
Asian
Pac
J
Reprod,
1(2),
125-34.
38.
Matsubayashi,
H.,
Hosaka,
T.,
Izumi,
S.
I.,
Suzuki,
T.,
Kondo,
A.,
&Makino,
T.
(2004)
Increased
depression
and
anxiety
in
infertile
Japanese
women
resulting
from
lack
of
husbands
support
and
feelings
of
stress.
General
Hospital
Psychiatry.
26(5):398-404
39.
Monga,
M.,
Alexandrescu,
B.,
Katz,
S.
E.,
Stein,
M.,
&
Ganiats,
T.
(2004).
Impact
of
infertility
on
quality
of
life,
marital
adjustment
and
sexual
function.
Urology,
63(1):126-130.
40.
Motl,
R.W.,
&
Snook,
E.M.
(2008).
Physical
activity,
self-efficacy,
and
quality
of
life
in
multiple
sclerosis,
ann.
behav.
med.
35,
111–115.
41.
Nejat,
S.,
Montazeri,
A.,
Holakouie,
K.,
Mohammad,
K.,
&
Majdzadeh,
S.
(2006).
The
world
health
organization
quality
of
life
(WHOQOL-BREF)
questionnaire:
translation
and
validation
study
of
the
Iranian
version
(Persian).
Journal
of
School
of
Public
Health
and
Institute
of
Public
Health
Research,
4(4),
1-12.
42.
Nene,
U.A.,
Coyaji,
K.,
&
Apte,
H.
(2009).
Infertility:
a
label
of
choice
in
the
case
of
sexually
dysfunctional
couples.
Patient
EducCounsJ,
59(3),
234–8.
43.
Newman,
R.
(2003).
Providing
direction
on
the
road
to
resilience.
Behavioral
Health
Management,
23(4),
42–43.
44.
Nilforooshan,
P.,
Latifi,
Z.,
Abedi,
M.,
&Ahmad,
A.
(2006).Comparing
the
different
aspects
of
quality
of
life
in
fertile
and
infertile
women.
Journal
of
Behavioral
Sciences,
4(8),
66-70.
45.
Ohaeri,
J.U.,
Awadalla,
A.W.,
&
Gado,
O.
M.
(2009).
Subjective
quality
of
life
in
a
nationwide
sample
of
Kuwaiti
subjects
using
the
short
version
of
the
WHO
quality
of
life
instrument.
Social
Psychiatry
and
Psychiatric
Epidemiology,
44(8),
693-701.
46.
Onat,
G.,
&
Beji,
N.K.
(2012).
Effects
of
infertility
on
gender
differences
in
marital
relationship
and
quality
of
life:
a
case-control
study
of
Turkish
couples,
European
Journal
of
Obstetrics
&
Gynecology
and
Reproductive
Biology,
165,
243–248.
47.
Pahlavani,
H.,
Malakouti,
K.
&
Shahrokh
Tehrani
Nejad,
E.
(2002)
Stressors,
their
coping
strategies
and
relation
to
mental
health
in
infertile
individuals.
Iranian
Journal
of
Psychiatry
and
Clinical
Psychology,
7,
87-79.
48.
Rafii,
F.,
Naseh,
L.,
&
Yadegary,
M.A.(2012).
Relationship
between
self-efficacy
and
quality
of
life
in
ostomates,
Iran
Journal
of
Nursing
(IJN).25(76),
64-76.
49.
Ragni,
G.,
Mosconi,
P.,
Baldini,
MP.,
Somigliana,
E.,
Vegetti,
W.,
Caliari,
I.,
&Nicolosi,
AE.(
2005).
Health-related
quality
of
life
and
need
for
IVF
in
1000
Italian
infertile
couples.
Hum
Reprod,
20,
1286-1291.
50.
Rashidi,
B.,
Montazeri,
A.,
Ramezanzadeh,
F.,
Shariat,
M.,
Abedinia,
N.,
&
Ashrafi,
M.
(2008).
Health-related
quality
of
life
in
infertile
couples
receiving
IVF
or
ICSI
treatment.
BMC
Health
Serv
Res.
8,186.
51.
Rezaie,
R.,
Nazari,
AM.,
Zahrakar,
K.,
&
Smaeelifar,
N.
(2013).
Effectiveness
of
existential
psychotherapy
in
increasing
the
resiliency
of
mentally
retarded
children’s
mothers.
International
Journal
of
Psychology
and
Behavioral
Research,
2(2),
59-64.
52.
Ridenour,
A.,
Yorgason,
J.,
Peterson,
B.
(2009).
The
infertility
resilience
model:
assessing
individual,
couple,
and
external
predictive
factors.
ContempFamTher.
31,
34–51.
53.
Samani,
S.,
Jokar,
B.
A.,
&
Sahragard,
N.
A.
(2006).
Resiliency,
mental
health
and
life
satisfaction.
Journal
of
Psychiatry
and
Clinical
Psychology,
3(3),
290-295.
54.
Sami,
N.,
&
Tazeen
S.A.
(2012).
Perceptions
and
experiences
of
women
in
Karachi,
Pakistan
regarding
secondary
infertility:
results
from
a
community-based
qualitative
study.
Obstetrics
and
Gynecology
International,
10,
235-41.
55.
Schweikert,
B.,
Hunger,
M.,
Meisinger,
C.,
Konig,
H.
H.,
Gapp,
O.,
&
Holle,
R.
(2008).
Quality
of
life
several
years
after
myocardial
infarction:
comparing
the
MONICA/KORA
registry
to
the
general
population.
European
Heart
Journal,
30(4):
436-443.
56.
Sexton,
MB.,
Byrd,
M.R.,
&
Kluge,
S.
(2010).
Measuring
resilience
in
women
experiencing
infertility
using
the
CD-RISC:
Examining
infertility-related
stress,
general
distress,
and
coping
styles.
J
PsychiatrRes.
44(4),
236-41.
57.
Sule,
R.,
Gupte,
S.,
&
De
Sousa.,
A.
(2017).
A
study
on
quality
of
life
and
psychopathology
in
couples
with
infertility,
Journal
of
Psychosocial
Rehabilitation
and
Mental
Health,
4(1),
19-22.
58.
Takaki,
J.,
&
Hibino,
Y.
(2014).
Family-related
opinions
and
stressful
situations
associated
with
psychological
distress
in
women
undergoing
infertility
treatment.
Int
J
Environ
Res
Public
Health,
11(9),
9068-9081.
59.
Tamannaeifar,
M.R.
(2011).
The
comparative
study
of
mental
health,
marital
adjustment
and
coping
responses
in
fertile-infertile
women,
Clinical
Psy
&
Personality
Journal
Of
Shahed
University,
Third
Year,
No.4,
51-60.
60.
Tiet,
Q.
Q.,
&
Huizinga,
D.
(2002).
Dimensions
of
the
construct
of
resilience
and
adaptation
among
Inner
–
city
youth.
Journal
of
Adolescent
Research,
17(3),
260-276.
61.
Tovliat,
V.,
&
Tamannaeifar,
M.R.(2015).
A
comparison
of
stress
reactions,
coping
styles,
subjective
well-being
and
its
sub-scales
in
fertile
and
infertile
women,
Journal
of
Advanced
Medical
Sciences
and
Applied
Technologies,
1(2),
93-97.
62.
Trent,
M
.E.,
Rich,
M.,
Austin,
B.,
&
Gordon,
CM.
(2002).
Quality
of
life
in
adolescent
girls
with
polycystic
ovary
syndrome.
Arch
Pediatr
Adolesc
Adolesc
Med.
156(6),
556-60.
63.
Van
den
Broeck,
U.,
Emery,
M.,
Wischmann,
T.,
&Thorn,
P.
(2010).
Counselling
in
infertility:
individual,
couple
and
group
interventions.
Patient
EducCouns.
81(3),
422–8.
64.
Van
der
Akker,
OB.
(2005).
Coping,
quality
of
life
and
psychological
symptoms
in
three
groups
of
subfertile
women.
Patient
EducCouns.
57(2):183–9.
65.
Van
der
Slot,
W.
M.,
Nieuwenhuijsen,
C.,
van
den
Berg-Emons,
R.
J.,
Wensink
-
Boonstra,
A.
E.,
Stam,
H.
J.,
&
Roebroeck,
M.
E.
(2010).
Participation
and
health-related
quality
of
life
in
adults
with
spastic
bilateral
cerebral
palsy
and
the
role
of
self-efficacy.
Journal
of
Rehabilitation
Medicine,
42,
528–535.
66.
Verhaak,
C.M.,
Smeenk,
J.M.J.,
Evers,
A.W.M.,
Kremer,
J.A.M.,
Kraaimaat,
F.W.,
&
Braat,
DM.
(2007).
Women’s
emotional
adjustment
to
IVF:
a
systematic
review
of
25
years
of
research.
Hum
Reprod
Update.
13(1):27–36.
67.
Wagnild,
GM.,
&
Young,
HM.
(1993).
Development
and
psychometric
evaluation
of
the
Resilience
Scale.
J
Nurs
Meas.
1,
165–78.
68.
Xiaoli,
S.,
Mei,
L.,
Junjun,
B.,
Shu,
D.,
Zhaolian,
W.,
&
Jin,
W.
(2016).
Assessing
the
quality
of
life
of
infertile
Chinese
women:
a
cross-sectional
study,
Taiwanese
Journal
of
Obstetrics
&
Gynecology,
55,
244-250.
|

