|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
........................................................
In Memoriam
Professor
Orhan Ekrem Müftüoglu
|
........................................................
Original
Contribution / Clinical Investigation
|







|
Cholelithiasis
and cholecystectomy may lower the low density
lipoprotein cholesterol in plasma
DOI: 10.5742/MEWFM.2017.93010
[pdf
version]
Mehmet Rami Helvaci, Mursel Davarci, Orhan Veli
Ozkan, Ersan Semerci, Abdulrazak Abyad, Lesley
Pocock
Serum
and follicular fluid vitamin D and follicular
response among infertile women undergoing ICSI
DOI: 10.5742/MEWFM.2017.93011
[pdf
version]
Sedighe Esmaeilzadeh, Maryam Aliasgharpour,
Parvaneh Mirabi, Azita Ghanbarpour
Maede Fasihian
Studying
the relation of quality of work life with socio-economic
status and general health among the employees
working in Students Welfare Fund of Ministry
of Health and Medical Education in 2016
DOI: 10.5742/MEWFM.2017.93012
[pdf
version]
Saeed Reza Azami, Nasrin Shaarbafchizadeh, Soheil
Mokhtari, Ali Maher
On the Effect
of Cognitive Behavioural Counseling on Sexual
Satisfaction of Mothers with Autistic Children:
A Randomized Clinical Trial
DOI:
[pdf version]
Leila Arbil, Mitra Kolivand, Farzaneh Golboni,
Effat MerghatiKhoei, Mansour Rezaei
Pre-operative
sublingual misoprostol and intra-operative blood
loss during total abdominal hysterectomy: a
randomized single-blinded controlled clinical
trial
DOI: 10.5742/MEWFM.2017.93013
[pdf
version]
Taravat Fakheri, Tayebe Noori
Investigating
the Effect of Endotracheal Tube Cuff Pressure
on Sore Throat, Hoarseness and Cough in Patients
with Coronary Artery Bypass Surgery
DOI: 10.5742/MEWFM.2017.93014
[pdf
version]
Ali Akbar Vaezi, Mohammad Hassan Mondegari Bamakan
Comparing
the Self-Esteem and Resiliency between Blind
and Sighted Children and Adolescents in Kermanshah
City
DOI: 10.5742/MEWFM.2017.93015
[pdf
version]
Saeedeh Bakhshi, Nafiseh Montazeri , Babak Nazari,
Arash Ziapour, Hashem Barahooyi,
Fatemeh Dehghan
|
........................................................
Population
and Community Studies
|







|
Frequency
of Uric Acid Levels, Symptomatic and Asymptomatic
Hyperuricemia among the Pakistani Population
DOI: 10.5742/MEWFM.2017.93016
[pdf
version]
Waris Qidwai, Masood Jawaid
Determinants
of Tooth Brushing among Primary School Students
DOI: 10.5742/MEWFM.2017.93017
[pdf
version]
Mohammad Mahboubi, Mohammad Ismail Motlagh,
Mehdi Mirzaei-Alavijeh, Farzad Jalilian, Hassan
Gharibnavaz,
Mohammad Fattahi
Depression
in patients suffering from gender dysphoria:
The hospitalized patients of Legal Medicine
Center in Southwest of Iran
DOI: 10.5742/MEWFM.2017.93018
[pdf
version]
Zahra Gorjian, Mohammad Zarenezhad, Mohhamad
Mahboubi, Saeid Gholamzadeh,
Nahid Mahmoodi
An epidemiological
study of suicide attempts and to determine the
correlation between attempted suicide causes
and demographic characteristics of people in
Kermanshah Province during a year
DOI: 10.5742/MEWFM.2017.93019
[pdf
version]
Hamid Reza Shetabi, Samira Rostami, Mohsen Mohammadi,
Mahsa Cheleii, Lida Saedi, Saba Amiri Nasab,
Shirin Zardui GolAnbari
The
effectiveness of life skills training on happiness,
mental health, and marital satisfaction in wives
of Iran-Iraq war veterans
DOI: 10.5742/MEWFM.2017.93038
[pdf
version]
Kamal Solati
The
Role of Self-Compassion Factors in Predicting
the Marital Satisfaction of Staff at Kermanshah
University of Medical Sciences
DOI:10.5742/MEWFM.2017.93020
[pdf
version]
Parisa Janjani, Lida Haghnazari, Farahnaz Keshavarzi,
Alireza Rai
Mediating
role of irrational beliefs in the relationship
between the quality of family communication
and marital satisfaction
DOI:10.5742/MEWFM.2017.93021
[pdf
version]
Parisa Janjani, Khodamorad Momeni, Alireza Rai,
Mohammad Reza Saidi
|
........................................................
Review Article
........................................................
International Health
Affairs
........................................................
Education
and Training
........................................................
Clinical
Research and Methods
|





|
Adaptive
LASSO Logistic Regression applied on gene expression
of prostate cancer
DOI: 10.5742/MEWFM.2017.93028
[pdf version]
Amir Hossein Hashemian, Maryam Ghobadi Asl,
Soodeh Shahsavari, Mansour Rezaei,
Hadi Raeisi Shahraki
The
prevalence of brain and neck injuries in patients
with maxillofacial fractures in teaching hospitals
of Rasht in 2016
DOI: 10.5742/MEWFM.2017.93029
[pdf
version]
Seyed Mohammad Talebzadeh, Ali Khalighi Sigaroudi,
Babak Alijani, Safa Motevasseli,
Saied Dashtyari, Mahsa Shariati, Zeinab Davoudmanesh
Cultural
competency: a concept analysis in TUMS (Tehran
University of Medical Science) DOI:
10.5742/MEWFM.2017.93030
[pdf version]
Foruzan Khatamidoost, Mandana Shirazy, Hamid
Khankeh, Nemat Allah Musapour
Majid Sadeghi, Kamran Soltani Arabshahi
The
Effect of Proprioceptive Neuromuscular Facilitation
(PNF) on Activities of Daily Living of client
with Cerebrovascular accident
DOI: 10.5742/MEWFM.2017.93031
[pdf
version]
Najafi Doulatabad Shahla, Afrasiabifar Ardashir,
Parandvar Yaghoub
Evaluation
of the ratio of T helper 17 and T regulatory
cells in patients with chronic idiopathic urticaria
DOI: 10.5742/MEWFM.2017.93032
[pdf
version]
Hossein Shahriari, Farahzad Jabbari, Seyyed
Abdolrahim Rezaee, Houshang Rafatpanah
Majid Jafari, Reza Farid Hosseini, Majid Asadi-Samani
|
........................................................
Model
and System of Primary Care
........................................................
Case
Series and Case Reports
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| September 2017
- Volume 15, Issue 7 |
|
|
Carbamazepine-induced
toxic epidermal necrolysis treated with intravenous
immunoglobulin and amniotic membrane: A case
report
Mohammadreza Mobayen (1)
Abbas Darjani (2)
Roghayeh Aghebati (3)
Ramyar Farzan (4)
(1) Assistant Professor of Burn Reconstruction.
Guilan University of Medical Sciences,Rasht
,Iran
(2) Assistant Professor of Department of Dermatology,
Razi Hospital, Guilan University of Medical
Sciences, Rasht, Iran
(3) Graduate of Master’s Degree in Health
Education and health promotion, Faculty of Health,
Guilan University of Medical Sciences, Rasht,
Iran .
(4) Department of Surgery, Plastic Surgeon,
Guilan University of medical science, Rasht,
Iran
Correspondence:
Ramyar FarzanDepartment of Surgery,
Guilan University of Medical Science,
Rasht, Iran
Tel:0989111311055
Email:
ramyarfarzan@yahoo.com
|
Abstract
Introduction: Toxic
epidermal necrolysis (TEN) is a distinct
clinical entity within a spectrum of adverse
cutaneous drug reactions. The common causative
drugs are anticonvulsants, non-steroidal
anti inflammatory drugs, sulfonamides
and other antibiotics. Carbamazepine is
an important antiepileptic drug used to
treat bipolar disorder, seizures and nerve
pain such as trigeminal neuralgia and
diabetic neuropathy, which is considered
to be one cause of TEN.
Case report
We describe TEN in a 7-year-old Iranian
girl with no mucosal involvement treated
as an emergency burns case with intravenous
Immunoglobulin and amniotic membrane.
At the end of the treatment period, there
were no scars and good cosmetic results
achieved.
Conclusion:
We conclude that early diagnosis,
supportive care and careful monitoring
for complications comprise crucial management
in TEN. Moreover, using an effective co-adjuvant
treatment (amniotic membrane and intravenous
immunoglobulin), will improve the skin
lesions of TEN totally without scars.
Key words:
Amniotic membrane, toxic epidermal necrolysis,
intravenous immunoglobulin
|
Toxic epidermal necrolysis (TEN), known as
Lyell’s syndrome, lies within the spectrum
of severe cutaneous adverse reactions (SCAR)
induced by drugs or infections. TEN is an acute
life-threatening dermatosis characterized by
extensive epidermal sloughing at the dermo-epidermal
junction, resulting from hypersensitivity complex
and keratinocyte apoptosis (1). This medical
emergency presents mucocutaneous tenderness
and typically hemorrhagic erosions, erythema
and more or less severe epidermal detachment
presenting as blisters and areas of denuded
skin (affected body surface more than 30% of
total body surface area). The incidence is approximately
one case per million people per year and the
mortality rate varies from 27% to 31% (1, 2).
The drugs commonly implicated as the cause of
TEN are anticonvulsants, non-steroidal anti-inflammatory
drugs, sulfonamides and other antibiotics. Carbamazepine,
an important antiepileptic drug, has been reported
as having potential to cause serious cutaneous
reactions (2). Here, we present a case of TEN
occurring 2 days after beginning the use of
carbamazepine.
On
21
October
of
2015,
a
7-year-old
Iranian
girl
of
Caucasoid
origin
was
admitted
to
Velayat
burn
care
center
in
Rasht,
a
city
in
north
of
Iran,
with
extended
skin
detachment.
10
days
before
admission,
due
to
epilepsy
disorder,
she
was
treated
with
Carbamazepine,
prescribed
by
a_
neurologist,
starting
at
curative
dosage
(150
mg
twice
daily).
Forty-eight
hours
after
beginning
the
treatment,
she
presented
with
fever
and
developed
generalized
rash
all
over
her
body.
Then
she
was
admitted
to
an
internal
medicine
department.
The
carbamazepine
treatment
was
stopped
and
the
drug
was
replaced
with
Sodium-Valproate.
During
7
days,
despite
treating
with
topical
anti-inflammatory
creams
and
oral
non-steroidal
anti-inflammatory
drugs
(NSAIDs),
she
presented
with
fever
and
maculo
papular
skin
eruption
extended
with
few
bullae
on
friction-prone
areas
and
erosions
on
her
oral
mucosa
and
lips.
So
the
doctors
made
a
consultation
with
a
burn
fellow
and
the
patient
was
transferred
to
this
burn
care
center,
10
days
after
beginning
the
use
of
carbamazepine.
On
admission,
she
was
suffering
from
confluent
generalized
erythema
and
widespread
epidermal
necrosis
on
54%
of
her
body
surface
(based
on
rule
of
nines:
legs
(18%
×2
=
36%),
the
front
chest
(9%)
and
the
abdomen
(9%))
(Figure-1a).
Her
mental
status
examination
showed
total
alertness.
Also,
erythematous
papules
and
vesicles,
erosive
and
crusted
lesions,
purpuric
macules
and
papules
and
a
flask
bulla,
with
9x7
cm
diameter
on
the
base
of
the
right
foot,
were
presented.
She
had
eroded
lesions
on
the
lips
covered
with
hemorrhagic
crusts
and
severe
edema
of
eyelids
and
lips
(Figure-1b).
Figure
1a:
the
patient’s
manifestations
at
the
first
day
of
admission
 Figure
1b:
the
patient’s
manifestations
at
the
first
day
of
admission
Figure
1b:
the
patient’s
manifestations
at
the
first
day
of
admission

A
positive
Nikolsky’s
sign
(denudation
of
the
skin
with
gentle
tangential
pressure)
was
also
presented.
A
bacterial
culture
test
from
her
skin
lesions
revealed
no
growth.
She
showed
no
lesions
on
genital
area
and
conjunctiva.
The
skin
lesions
were
covered
with
petrolatum-
impregnated
gauze.
Physical
and
laboratory
data
at
the
first
day
of
admission
are
shown
in
Table
1.
Table
1:
Physical
and
laboratory
data
of
the
patient
at
admission
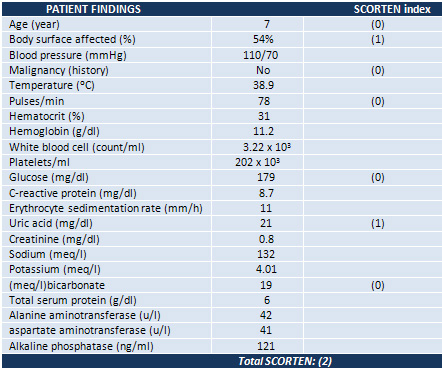
Of
all
SCORTEN
(severity-of-illness
score)
parameters
(3),
she
had
2
positive
indexes:
Initial
surface
of
epidermal
detachment
more
than
10%
and
Serum
urea
more
than
10
mmol/l.
So
she
was
not
managed
in
the
intensive
care
unit,
but
transferred
to
an
isolated
room
and
medical
treatment
with
intravenous
immunoglobulin
(at
a
dosage
of
20
gr
daily)
and
fluid
replacement
(intravenous
dextrose
5%)
was
initiated.
Also,
burn
wounds
were
initially
cleaned
with
gentle
brushing
and
using
soap
and
water.
Using
IVIG
for
2
days,
9
day
after
starting
manifestations,
her
lesions
improved
with
a
marked
decrease
in
the
flask
bulla
on
the
base
of
the
right
foot,
decreasing
body
temperature
on
normal
state
(no
fever),
generalized
scaling
and
decreasing
in
face
edema.
Figure
2
shows
her
clinical
manifestations
after
using
IVIG.
Figure
2:
The
patient’s
manifestation
improves
two
days
after
using
IVIG

Due
to
her
situation
and
because
she
was
not
totally
cured,
we
decided
to
cover
the
areas
of
epidermal
detachment
with
two
amniotic
membranes
approved
by
FDA
taken
from
Iranian
Tissue
Bank
(ITB)
which
is
a
multi-tissue
bank
in
Tehran.
In
the
operation
room,
debridement
was
performed
using
gentle
mechanical
techniques,
and
then
we
placed
the
membrane
on
her
body
surface.
She
was
intubated
during
the
whole
procedure,
and
IVIG
was
maintained.
Amniotic
membranes
dried
and
were
consequently
fixed
to
the
skin
during
the
next
4
days.
We
stopped
using
IVIG
3_
days
after
beginning.
She
improved
dramatically
during
the
following
24_
hours
after
procedure,
with
a
marked
decrease
in
her
generalized
erythema
and
swelling
(Figure
3).
Figure
3:
The
patient’s
manifestations
24
hours
after
membrane
placement

After
time,
all
erythematous
papules
and
vesicles
disappeared
and
her
appetite
rose
significantly.
Complete
re-epithelization
of
the
affected
skin
was
observed
four
days
after
the
membrane
placement
(Figure
4).
Figure
4:
the
patient’s
manifestations
4
days
after
membrane
placement

All
symptoms
and
skin
lesions
resolved
progressively.
The
skin
lesions
healed
without
scarring
but
with
hyper-pigmentation
(Figure
5).
The
patient
left
our
department
in
a
good
general
state
on
5
November
of
2015.
Figure
5:
The
skin
lesions
healed
without
scarring
but
with
hyper-
pigmentation

TEN
is
considered
as
a
medical
emergency
which
may
be
potentially
fatal
and
carries
a
high
mortality
rate
(2).
The
disease
started
with
general
malaise,
myalgia,
and
prodromal
symptoms.
A
burning,
painful
eruption
spread
from
the
face
to
the
neck
and
shoulders
and
later
to
the
entire
trunk
and
proximal
parts
of
limbs.
The
peak
manifestation
of
lesions
usually
occurs
in
a
week.
In
nearly
all
cases,
mucous
membranes
are
involved
and
Nikolsky’s
sign
is
usually
positive
(3).
Different
immuno-inflammatory
pathways
with
early
participation
of
activated
CD8
T-lymphocytes
are
involved.
Microscopically,
there
is
sub-epidermal
bulla
formation,
with
eosinophilic
epidermal
necrosis.
The
dermal
vessels
show
endothelial
swelling
without
any
vasculitis
or
necrosis.
Ultra-structurally
there
is
damage
to
the
basal
and
lower
spinous
levels
of
the
epidermis
and
cleft
formation
at
the
lamina-densa.
Immunofluorescences
is
always
negative
(1-3).
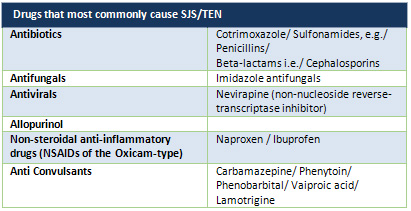
Drugs
are
considered
to
be
the
commonest
cause
of
TEN.
More
than
100
different
drugs
are
considered
as
having
caused
TEN,
but
only
a
minority
of
them
accounts
for
the
majority
of
cases
(2,
3)
(Table
2).
Table
2:
Drugs
that
most
commonly
cause
SJS/TEN
Carbamazepine
is
used
to
treat
bipolar
disorder,
seizures
and
nerve
pain
such
as
trigeminal
neuralgia
and
diabetic
neuropathy.
Some
studies
showed
that
among
anticonvulsant
drugs
which
induced
TEN,
the
majority
of
cases
were
due
to
Carbamazepine.
Also,
Konishi
et
al
(4)
performed
a
prospective
survey
on
335
children
treated
with
carbamazepine
and
the
result
showed
that
the
incidence
of
TEN
was
0.6%.
So
this
antiepileptic
drug
plays
an
important
role
in
skin
reactions
and
hospitalizations
due
to
these
kinds
of
side
effects.
Nowadays,
according
to
most
authors,
systemic
corticosteroids
are
of
unproven
benefit
in
the
early
disease
stage
and
are
clearly
deleterious
in
advanced
forms
of
TEN.
On
the
other
hand,
other
investigators
consider
systemic
corticosteroids
to
provoke
prolonged
wound
healing
and
increased
risk
of
infection,
hiding
early
signs
of
sepsis,
severe
gastrointestinal
bleeding
and
increased
mortality
(5).
So
we
did
not
use
systemic
corticosteroids
for
treatment
of
our
patient.
Historically,
natural
amniotic
membranes
have
been
successfully
used
for
wound
and
reconstructive
purposes
since
the
early
20th
century.
Amniotic
membrane
forms
the
innermost
layer
of
the
placenta
which
consistos
of
an
epithelial
layer
and
an
avascular
matrix
(6).
There
are
many
reports
of
using
amniotic
membrane
in
treatment
of
ocular
reactions
leads
to
good
results.
Enhancement
of
granulation
tissue
production,
production
of
angiogenic
and
anti-inflammatory
proteins,
induction
of
macrophage
apoptosis
and
a
decrease
in
wound
infection
rates
are
advantages
in
using
this
method
(6-7).
In
2002,
Dr.
John
et
al
(7)
presented
two
patients
who
were
the
first
cases
of
acute
toxic
epidermal
necrolysis
treated
with
amniotic
membrane
transplantation
and
the
first
use
of
the
procedure
on
external
eyelid
surfaces
with
good
healing
of
the
eyelids.
He
reported
that
this
new
treatment
for
acute
toxic
epidermal
necrolysis
preserves
normal
ocular
and
eyelid
surfaces
and
may
prevent
blindness.
In
2012,
Maylon-Hsu
et
al
(8)
presented
the
first
case-control
study
using
amniotic
membrane
in
management
of
91
cases
with
Acute
Stevens–Johnson
Syndrome
and
TEN
ocular
lesions.
The
results
showed
patients
with
no
acute
ocular
surface
signs
(such
as
our
patient
in
this
article)
or
mild
ocular
surface
inflammation
have
a
good
prognosis.
To
the
best
of
our
knowledge,
this
is
the
second
case
treated
with
amniotic
membrane
and
IVIG
together
on
skin
detachment
sites
rather
than
ocular
surface
on
a
patient
with
TEN
disorders
(9).
Today,
the
effect
of
amniotic
membrane
on
burnt
skin
of
children
is
approved
(10).
But
we
found
no
reports
of
using
this
method
on
skin
detachment
due
to
TEN
in
children.
So
we
report
this
case
to
present
this
method
as
an
effective
choice
to
cure
TEN
detachment
lesions
on
skin.
The
amniotic
membrane
plays
the
rule
of
an
effective
barrier
to
prevent
dehydration
and
infection.
On
the
other
hand,
we
used
IVIG
which
caused
a
rapid
cessation
of
skin
detachment
and
decreased
her
temperature.
We
believe,
despite
rare
incidence,
TEN
is
a
condition
with
a
high
level
of
complications
and
mortality
and
it
must
be
considered
as
an
important
burn
emergency
which
should
be
treated
in
burn
emergency
units,
so
that
both
adequate
wound
care
and
essential
intensive
supportive
treatment
can
be
given.
Patients
with
a
large
degree
of
affected
surface
area
should
be
treated
as
patients
with
intensive
burn
injuries,
with
close
monitoring
and
anticipation
that
life
threatening
complications
might
arise.
We
conclude
that
early
diagnosis,
supportive
care
and
careful
monitoring
for
complications
comprise
crucial
management
in
TEN.
Moreover,
good
cosmetic
results
are
an
important
goal
which
must
be
considered
during
treatment
period.
Using
an
effective
co-adjuvant
treatment
(amniotic
membranes
and
IVIG),
our
patient’s
lesions
improved
and
her
skin
was
totally
without
any
scars.
Consent:
Written
informed
consent
was
obtained
from
her
parents
for
the
publication
of
this
report
and
accompanying
images.
A
copy
of
the
consent
is
available
in
the
end
of
this
paper.
Acknowledgement:
We
thank
Mr.
M.
Haghiri-Limudahi
and
Mr.
AR
Golzar
for
critical
reading
of
the
manuscript
and
for
the
insightful
suggestions.
Click
here
for
copy
of
Consent
Form
1.
AA
Mohammadi,
H.R.,
MJ
Hasheminasab,
B
Sabet,
MK
Mohammadi,
S
Abbasi
,
M
Amini,
Amniotic
Membrane
Dressing
vs
Conventional
Topical
Antibiotic
Dressing
in
Hospitalized
Burn
Patients.
Iranian
Red
Crecent
Medical
Journal,
2009.
11(1):
p.
66-70.
2.
Beck
A,
Q.K.,
Gamelli
RL,
Mosier
MJ,
Pediatric
toxic
epidermal
necrolysis:
using
SCORTEN
and
predictive
models
to
predict
morbidity
when
a
focus
on
mortality
is
not
enough.
J
Burn
Care
Res,
2015.
36(1):
p.
167-177.
3.
Hsu
M,
J.A.,
Verner
R,
Lin
A,
Bouchard
C,
Indications
and
outcomes
of
amniotic
membrane
transplantation
in
the
management
of
acute
Stevens-Johnson
syndrome
and
toxic
epidermal
necrolysis:
A
case
control
study.
Cornea,
2012.
31(12):
p.
1394-1402.
4.
John
T,
F.G.,
John
ME,
Cheng
K,
Hu
D,
Amniotic
membrane
in
the
surgical
management
of
acute
toxic
epidermal
necrolysis.
Ophthalmology,
2002.
109(2):
p.
351-360.
5.
Konishi
T,
N.,
Hongo
K,
Murakami
M,
Yamatani
M,
Eokada
T,
Carbamazepine
induced
skin
rash
in
children
with
epilepsy.
Eur
J
Pediatr,
1993.
152:
p.
605-608.
6.
Mostaque
AK,
R.K.,
Comparisons
of
the
effects
of
biological
membrane
(amnion)
and
silver
sulfadiazine
in
the
management
of
burnwounds
in
children.
J
Burn
Care
Res,
2011.
32(2):
p.
200-209.
7.
Quirke
KP,
B.A.,
Gamelli
RL,
Mosier
MJ,
A
15-year
review
of
pediatric
toxic
epidermal
necrolysis.
J
Burn
Care
Res,
2015.
36(1):
p.
130-136.
8.
Roongpisuthipong
W,
P.S.,
Klangjareonchai
T,
Retrospective
Analysis
of
Corticosteroid
Treatment
in
Stevens-Johnson
Syndrome
and/or
Toxic
Epidermal
Necrolysis
over
a
Period
of
10
Years
in
Vajira
Hospital,
Navamindradhiraj
University,
Bangkok.
Dermatol
Res
Pract,
2014.
9.
Schwartz
R,
A.E.,
Palisson
F,
Lamotrigine-induced
toxic
epidermal
necrolysis
treated
with
intravenous
immunoglobulin
and
amniotic
membranes.
Arch
Dermatol,
2008.
144(6):
p.
724-726.
10.
Singh
PK,
K.M.,
Kumar
D,
Kumar
P,
Morphological
Pattern
of
Cutaneous
Adverse
Drug
Reactions
due
to
Antiepileptic
Drugs
in
Eastern
India.
J
Clin
Diagn
Res,
2015.
9(1):
p.
WC01-3.
|
|
.................................................................................................................

|
| |
|

