|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
........................................................
In Memoriam
Professor
Orhan Ekrem Müftüoglu
|
........................................................
Original
Contribution / Clinical Investigation
|







|
Cholelithiasis
and cholecystectomy may lower the low density
lipoprotein cholesterol in plasma
DOI: 10.5742/MEWFM.2017.93010
[pdf
version]
Mehmet Rami Helvaci, Mursel Davarci, Orhan Veli
Ozkan, Ersan Semerci, Abdulrazak Abyad, Lesley
Pocock
Serum
and follicular fluid vitamin D and follicular
response among infertile women undergoing ICSI
DOI: 10.5742/MEWFM.2017.93011
[pdf
version]
Sedighe Esmaeilzadeh, Maryam Aliasgharpour,
Parvaneh Mirabi, Azita Ghanbarpour
Maede Fasihian
Studying
the relation of quality of work life with socio-economic
status and general health among the employees
working in Students Welfare Fund of Ministry
of Health and Medical Education in 2016
DOI: 10.5742/MEWFM.2017.93012
[pdf
version]
Saeed Reza Azami, Nasrin Shaarbafchizadeh, Soheil
Mokhtari, Ali Maher
On the Effect
of Cognitive Behavioural Counseling on Sexual
Satisfaction of Mothers with Autistic Children:
A Randomized Clinical Trial
DOI:
[pdf version]
Leila Arbil, Mitra Kolivand, Farzaneh Golboni,
Effat MerghatiKhoei, Mansour Rezaei
Pre-operative
sublingual misoprostol and intra-operative blood
loss during total abdominal hysterectomy: a
randomized single-blinded controlled clinical
trial
DOI: 10.5742/MEWFM.2017.93013
[pdf
version]
Taravat Fakheri, Tayebe Noori
Investigating
the Effect of Endotracheal Tube Cuff Pressure
on Sore Throat, Hoarseness and Cough in Patients
with Coronary Artery Bypass Surgery
DOI: 10.5742/MEWFM.2017.93014
[pdf
version]
Ali Akbar Vaezi, Mohammad Hassan Mondegari Bamakan
Comparing
the Self-Esteem and Resiliency between Blind
and Sighted Children and Adolescents in Kermanshah
City
DOI: 10.5742/MEWFM.2017.93015
[pdf
version]
Saeedeh Bakhshi, Nafiseh Montazeri , Babak Nazari,
Arash Ziapour, Hashem Barahooyi,
Fatemeh Dehghan
|
........................................................
Population
and Community Studies
|







|
Frequency
of Uric Acid Levels, Symptomatic and Asymptomatic
Hyperuricemia among the Pakistani Population
DOI: 10.5742/MEWFM.2017.93016
[pdf
version]
Waris Qidwai, Masood Jawaid
Determinants
of Tooth Brushing among Primary School Students
DOI: 10.5742/MEWFM.2017.93017
[pdf
version]
Mohammad Mahboubi, Mohammad Ismail Motlagh,
Mehdi Mirzaei-Alavijeh, Farzad Jalilian, Hassan
Gharibnavaz,
Mohammad Fattahi
Depression
in patients suffering from gender dysphoria:
The hospitalized patients of Legal Medicine
Center in Southwest of Iran
DOI: 10.5742/MEWFM.2017.93018
[pdf
version]
Zahra Gorjian, Mohammad Zarenezhad, Mohhamad
Mahboubi, Saeid Gholamzadeh,
Nahid Mahmoodi
An epidemiological
study of suicide attempts and to determine the
correlation between attempted suicide causes
and demographic characteristics of people in
Kermanshah Province during a year
DOI: 10.5742/MEWFM.2017.93019
[pdf
version]
Hamid Reza Shetabi, Samira Rostami, Mohsen Mohammadi,
Mahsa Cheleii, Lida Saedi, Saba Amiri Nasab,
Shirin Zardui GolAnbari
The
effectiveness of life skills training on happiness,
mental health, and marital satisfaction in wives
of Iran-Iraq war veterans
DOI: 10.5742/MEWFM.2017.93038
[pdf
version]
Kamal Solati
The
Role of Self-Compassion Factors in Predicting
the Marital Satisfaction of Staff at Kermanshah
University of Medical Sciences
DOI:10.5742/MEWFM.2017.93020
[pdf
version]
Parisa Janjani, Lida Haghnazari, Farahnaz Keshavarzi,
Alireza Rai
Mediating
role of irrational beliefs in the relationship
between the quality of family communication
and marital satisfaction
DOI:10.5742/MEWFM.2017.93021
[pdf
version]
Parisa Janjani, Khodamorad Momeni, Alireza Rai,
Mohammad Reza Saidi
|
........................................................
Review Article
........................................................
International Health
Affairs
........................................................
Education
and Training
........................................................
Clinical
Research and Methods
|





|
Adaptive
LASSO Logistic Regression applied on gene expression
of prostate cancer
DOI: 10.5742/MEWFM.2017.93028
[pdf version]
Amir Hossein Hashemian, Maryam Ghobadi Asl,
Soodeh Shahsavari, Mansour Rezaei,
Hadi Raeisi Shahraki
The
prevalence of brain and neck injuries in patients
with maxillofacial fractures in teaching hospitals
of Rasht in 2016
DOI: 10.5742/MEWFM.2017.93029
[pdf
version]
Seyed Mohammad Talebzadeh, Ali Khalighi Sigaroudi,
Babak Alijani, Safa Motevasseli,
Saied Dashtyari, Mahsa Shariati, Zeinab Davoudmanesh
Cultural
competency: a concept analysis in TUMS (Tehran
University of Medical Science) DOI:
10.5742/MEWFM.2017.93030
[pdf version]
Foruzan Khatamidoost, Mandana Shirazy, Hamid
Khankeh, Nemat Allah Musapour
Majid Sadeghi, Kamran Soltani Arabshahi
The
Effect of Proprioceptive Neuromuscular Facilitation
(PNF) on Activities of Daily Living of client
with Cerebrovascular accident
DOI: 10.5742/MEWFM.2017.93031
[pdf
version]
Najafi Doulatabad Shahla, Afrasiabifar Ardashir,
Parandvar Yaghoub
Evaluation
of the ratio of T helper 17 and T regulatory
cells in patients with chronic idiopathic urticaria
DOI: 10.5742/MEWFM.2017.93032
[pdf
version]
Hossein Shahriari, Farahzad Jabbari, Seyyed
Abdolrahim Rezaee, Houshang Rafatpanah
Majid Jafari, Reza Farid Hosseini, Majid Asadi-Samani
|
........................................................
Model
and System of Primary Care
........................................................
Case
Series and Case Reports
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| September 2017
- Volume 15, Issue 7 |
|
|
The effectiveness of
sexual skills training with a cognitive-behavioral
approach on sexual dysfunction among infertile
women
Nasrin
Jalilian
Zahra Mokari
Maternity Research Center,
Kermanshah University of Medical Sciences,
Kermanshah, Iran
Correspondence:
Zahra Mokari
Maternity Research Center,
Imam Reza Hospital, Kermanshah University of
Medical Sciences,
Kermanshah, Iran,
Email: Zahramokari@
yahoo.com
|
Abstract
Background:
There is evidence that sexual dysfunction
in infertile women is more common than
fertile women. As there is a relation
between infertility and sexual dysfunction,
treatment of this disorder seems necessary.
Therefore, the current study was done
to determine the effectiveness of sexual
skills training with a cognitive-behavioral
approach on sexual dysfunction among infertile
women.
Methods: This was a quasi-experimental
pre-test and post-test study which lasted
from June 2015 to February 2016. Study
population consisted of infertile women
aged 22 to 36 years with sexual dysfunction
who presented to our academic infertility
center. Considering the inclusion and
exclusion criteria, 40 patients with informed
consent were randomly assigned to experimental
or control group. Subjects in the experimental
group received sexual skills training
for 10 weekly sessions. No intervention
was done in control group. Sexual dysfunction
scores were recorded using the Female
Sexual Function Index (FSFI). The gathered
data were analyzed using SPSS software
and the Chi-square test and co-variance
analysis.
Results: The
results showed that sexual skills training
had significant effect on sexual dysfunction
scores. The scores increased significantly
in the experimental group (P< 0.001).
Conclusion:
It is suggested that psychologists, psychotherapists,
and obstetric and gynecologists use sexual
skills training with cognitive-behavioral
approach for infertile women who suffer
from sexual dysfunction.
Key words:
Sexual skills training; cognitive-behavioral;
sexual dysfunction; infertile women
|
Infertility which is defined as pregnancy failure
despite at least one year of unprotected sexual
intercourse now has a prevalence of 20% and
has become a public health issue (1). A previous
study reported the prevalence of infertility
as 24.9% in Iran (2). One of the concerns in
infertility is sexual dysfunction (3) which
is persistent or recurring disorders in four
domains including sexual desire, sexual arousal,
penetration disorder or inability to achieve
orgasm according to DSM-IV. In DSM-V some modifications
have been made and sexual desire and arousal
have been combined and the item pain during
intercourse has been removed. The latter has
been combined with vaginismus under a new disorder
in DSM-V (4).
An important aspect of infertility is the relationship
of this condition with sexual health. It seems
that this aspect of infertility has been overlooked
in developing countries (5). In other words,
sexual dysfunction is a silent partner of infertility
treatments (6). Sexual satisfaction is among
the most important issues among infertile couples,
especially in women. This can affect all aspects
of marital life and even treatment progress
(7). It is likely that sexual dysfunction is
the etiology of infertility or may be the result
of another psychologic stress in one of the
couples or both of them (8). Most experts believe
that there is association between infertility
and sexual dysfunction (9). One of the biggest
objectives of sexual desire is to have children
(10). We encounter decreased sexual desire in
infertile persons which reduces the chance of
fertility. This decreased sexual activity increases
the persons who do not have children in such
a group of patients (11). Pregnancy is an inseparable
component of a sexual relationship and inability
to get pregnant often results in sexual problems
which causes anger and depression in the affected
couples (12).
Previous studies have confirmed sexual dysfunction
among infertile patients (13-17). All these
studies showed higher rate of sexual dysfunction
among infertile couples when compared to fertile
couples. In a former study in 2013, Jamali et
al. studied 502 infertile women and reported
that 87% of the sample had sexual dysfunction.
They noted that this high rate of sexual dysfunction
was due to lack of knowledge about sexual skills
and lack of pertinent training (18).
Another study in 2015 reported the prevalence
of sexual dysfunction as 55.5% among 236 infertile
women (19). The main reasons for sexual dysfunction
in the mentioned study were similarly lack of
knowledge about sexual skills and lack of pertinent
training. Considering these findings, it seems
necessary to resolve the problem of infertile
women through providing knowledge. This requires
more research studies. Miller believes that
cognitive-behavioral therapy should always be
the first step in the management of infertile
couples (20). Various forms of sexual dysfunction
can cause infertility such as intercourse-related
problems, decreased incidence of intercourse
(due to decreased sexual desire in 11% of cases,
impaired erection or premature ejaculation which
are the most common sexual dysfunctions in males
(66%) and lack of ejaculation (8%) in infertile
males. Also, vaginismus or painful intercourse
(58% of cases) and reduced sexual desire (28%
of cases) exist in infertile women. On the other
hand, insufficient sexual excitement in women
causes vaginal dryness which inhibits sperm
migration in the vagina (21).
Andrews stated that if it is not possible to
resolve infertility tension, at least efforts
should be made to decrease its burden. Therefore,
decreasing familial disputes and making the
couples satisfied with regard to sexual and
marital relationships are appropriate methods
for infertile couples (22). The World Health
Organization (WHO) requires its personnel to
go beyond clinical diagnoses and medical interventions
to address sexual dysfunction. This organization
necessitates its personnel to consider the psychological
aspects of sexual dysfunction and by addressing
such issues they try to improve the quality
of life of affected patients (23).
One of the methods that seem to be useful in
addressing the infertility problem and treatment
of sexual dysfunction is cognitive-behavioral
therapy. In this approach, using behavioral
methods, we try to change maladaptive cognitions
of a person (24). This approach was introduced
by Masters and Johnson in 1959. Before introduction
of this approach, sexual disorders were tolerated
in silence by the patients and professional
help was rarely accessible. The approach defined
by Masters and Johnson had a special schedule
that was named a package approach. In this package,
a set of special methods was used in a diagnosis
(25). There are several studies which indicate
the usefulness of sexual skills training. For
example, a previous study reported the efficacy
of sexual skills training on improving psychological
arousal during sexual relations and orgasm in
women (26). A previous study assessed the effect
of cognitive-behavioral based training on sexual
satisfaction among women with reduced sexual
desire. They reported that after training, a
significant difference existed regarding sexual
satisfaction scores between experimental and
control groups which supports the effectiveness
of cognitive-behavioral training (27). Another
study used cognitive-behavioral therapy in couples
with idiopathic infertility and reported this
approach as a successful one in order to help
infertile couples (28). Considering the literature,
there is no study to investigate the effect
of sexual skills training with cognitive-behavioral
approach on infertile couples.
The requirement to address the psychological
needs of infertile people especially women,
lack of accurate research studies regarding
infertility psychology, and the necessity to
find a short-term and affordable method and
the fact that there is no public or governmental
place to train infertile couples shows the fact
that such research studies should be done in
countries like Iran. Considering the fact that
more than half of sexual dysfunctions are due
to lack of knowledge or insufficient knowledge
and an incorrect belief about sexual relations
(30), the current study was carried out.
Research Hypotheses
Hypothesis 1: Sexual skills training improves
sexual desire in infertile women
Hypothesis 2: Sexual skills training improves
psychological arousal in infertile women
Hypothesis 3: Sexual skills training increases
vaginal lubrication in infertile women
Hypothesis 4: Sexual skills training increases
orgasm in infertile women
Hypothesis 5: Sexual skills training improves
sexual satisfaction in infertile women
Hypothesis 6: Sexual skills training reduces
sexual pain in infertile women
Hypothesis 7: Sexual skills training improves
sexual function in infertile women
This quasi-experimental study with pre-test
and post-test design was approved by the ethics
committee of our university. The study population
consisted of infertile women who presented to
our academic infertility center. The sampling
method was convenience method. Considering the
inclusion and exclusion criteria and response
rate, 40 subjects were selected. They were randomly
divided into experimental and control groups
(20 subjects in each group). Subjects in the
experimental group received sexual skills training
for 10 weekly 2-hour sessions. The control group
did not receive any intervention. After completing
this period, both groups completed the Female
Sexual Function Index (FSFI). For ethical considerations,
after 10 weeks, sexual skills training was done
for the control group. The personal data was
kept confidential. Inclusion criteria were written
informed consent, being a volunteer for the
study, age range of 22 to 36 years, sexual dysfunction,
one year passed from unsuccessful pregnancy,
and primary infertility (no children or step
children). Exclusion criteria were having physical
conditions (spinal cord injury, limb amputation,
paralysis, and anatomic disturbances in the
limbs), psychiatric disorders (receiving treatment
for psychiatric disorder by a physician or a
psychiatrist), medical disorder (cardiovascular
diseases, pulmonary diseases, hypo- or hyperthyroidism,
epilepsy or diabetes), having stressful experiences
(death or acute illness of a close relative
and major change in life in the preceding 3-month
period), alcohol or drug addiction, male-factor
infertility, plan for pregnancy-assisted methods
such as intra-uterine insemination or intra-vitro
fertilization in the next 6 months, and taking
medications for sexual dysfunction. The data
were analyzed using multi-variable ANCOVA (analysis
of covariance) by SPSS software (ver. 19.0).
Tool
The Female Sexual Function Index (FSFI) was
developed by Rosen et al in 2000 and is a self-report
measure of sexual function that contains 19
items. This assesses sexual arousal, vaginal
lubrication, orgasm, satisfaction, and pain.
The score range is from 0 to 5 and higher scores
indicate more satisfactory sexual function.
This questionnaire’s validity and reliability
have been approved by Rosen et al. (31). Also
in an Iranian study in 2009, reliability and
validity of the Persian version of this questionnaire
was confirmed (32). The authors declared that
this questionnaire is a valid and reliable one
to investigate female sexual function and as
a useful screening method. Cronbach’s alpha
coefficient by split half and test-retest methods
were respectively 78% and 75%. Subscales had
coefficients of 63% to 75% by split half method
and 70-81% by test-retest method. As this questionnaire
covers all items of sexual dysfunction including
pain, it was selected for this study.
Therapeutic protocol
The cognitive-behavioral protocol used here
is the one described by Masters and Johnson
in 1996 and modified by Azartash in 2011 (33)
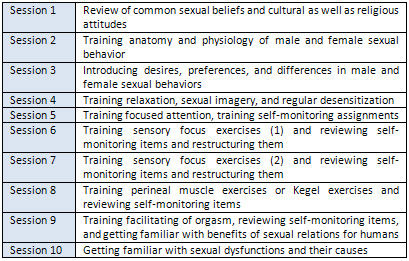
(Table 1).
Table 1. Summary of sexual skills training
with cognitive-behavioral approach
Table
2
shows
Demographic
data
of
experimental
and
control
groups.
Table
2
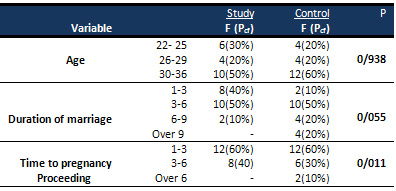
Considering
the
Chi-squared
test
results,
the
hypothesis
of
homogeneity
between
the
groups
is
significant.
Table
3.
Mean
and
standard
deviation
of
sexual
function
and
its
items
at
pre-test
and
post-test
states
in
experimental
and
control
groups
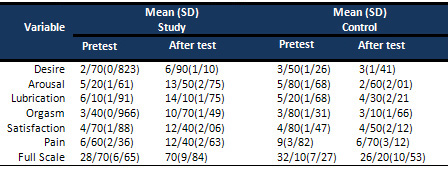
Considering
the
data
presented
in
Table
3,
the
experimental
group
achieved
higher
scores
after
the
intervention.
In
order
to
assess
the
significance
of
the
changes
and
determine
the
effect
size
of
sexual
training
on
sexual
function
improvement
in
the
experimental
group,
first
the
pre-test
scores
were
modified.
Then,
using
the
ANCOVA,
the
effect
size
of
sexual
skills
training
on
sexual
function
improvement
in
infertile
women
was
determined.
Before
using
ANCOVA,
its
assumptions
were
reviewed.
In
order
to
determine
normal
distribution
of
data,
the
Shapiro-Wilk
test
was
used.
To
address
the
assumptions,
Leven’s
test
was
used.
The
Box
test
was
not
significant
for
any
of
the
variables
(BOX=
39.741,
F=
1.191,
P=
0.250).
Other
assumptions
of
ANCOVA
were
reviewed
and
all
of
them
showed
that
assumptions
have
been
addressed.
Table
4.
Analysis
of
covariance
to
compare
sexual
function
scores
between
experimental
and
control
groups
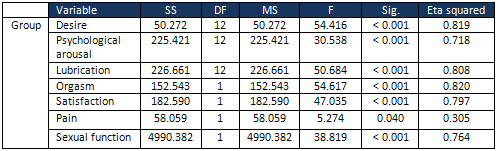
Table
4
shows
that,
after
modifying
pre-test
scores,
there
was
significant
difference
in
post-test
scores
of
desire
(F
(12,
1)=
54.416,
P
<
0.001),
psychologic
arousal
(F
(12,
1)=
30.538,
P<
0.001),
lubrication
(F(12,
1)=
50.648,
P<
0.001),
orgasm
(F(12,
1)=
54.617,
P<
0.001),
satisfaction
(F(12,
1)=
47.035,
P<
0.001),
and
sexual
function
(F(12,
1)=
38.819,
P<0.001)
between
experimental
and
control
groups.
In
other
words,
it
can
be
stated
that
with
9%
confidence
that
sexual
skills
training
improved
sexual
function
of
infertile
women.
Considering
the
Eta
squared
value,
the
effect
size
of
this
training
was
76%.
As
seen
in
Table
4,
sexual
skills
training
was
also
effective
on
pain
(F(12,
1)=
5.274,
P<
0.05).
Considering
Eta
squared
value
of
lower
than
0.35,
it
shows
that
this
training
was
not
so
effective
on
pain.
This
study
was
done
with
the
objective
of
determining
the
effect
of
training
sexual
skills
with
a
cognitive-behavioral
therapy
on
sexual
dysfunction
of
infertile
women.
For
the
experimental
group,
10
weekly
sessions
of
training
sexual
skills
were
performed,
while
no
intervention
was
done
in
the
control
group.
Both
groups
completed
the
FSFI
at
baseline
and
again
after
10
weeks.
Considering
the
ANCOVA
results,
it
can
be
concluded
that
sexual
function
scores
were
significant
after
10
weeks
between
experimental
and
control
groups.
Post-test
scores
were
higher
in
the
experimental
group
which
reflects
the
efficacy
of
the
sexual
skills
training.
Therefore,
all
the
study
hypotheses,
except
hypothesis
6
which
relates
to
pain,
are
approved.
There
are
limited
studies
about
the
effect
of
training
sexual
skills
on
sexual
dysfunction
in
Iran.
The
findings
of
the
study
are
in
agreement
with
some
former
studies
(34-42).
All
the
mentioned
studies
indicated
the
effectiveness
of
sexual
skills
training
with
cognitive-behavioral
therapy
on
sexual
function.
The
intervention
used
here
had
a
significant
effect
on
all
items
of
sexual
function,
except
for
pain.
Although
the
change
in
pain
score
was
not
statistically
significant,
when
mean
score
at
pre-test
(6.60)
is
compared
to
post-test
score
(12.40),
we
observe
improvement.
However,
this
change
was
not
statistically
significant.
It
should
be
noted
that
the
training
used
here
lasted
for
10
weeks
and
this
time
course
is
too
short
to
resolve
pain.
According
to
a
previous
study
(43),
the
required
time
to
address
vaginismus
was
34
sessions
in
12
months.
During
this
long
time,
patients
gradually
achieved
higher
level
of
vaginal
muscles
control
and
non-painful
intercourse.
The
lack
of
significance
regarding
effect
on
pain
may
be
justified
by
the
study
period.
The
current
findings
are
compatible
with
a
previous
study
(44)
that
studied
a
6-month
therapeutic
plan
to
improve
sexual
function
and
satisfaction
and
marital
life
skills.
In
addition
to
relation
between
infertility
and
sexual
function
that
always
should
be
addressed
in
treatment
of
infertility,
sexual
desire
is
also
an
important
factor
(45).
It
can
be
stated
that
sexual
relations
by
affecting
couples’
thoughts
and
feelings
directly
or
indirectly
can
affect
their
life.
The
couples
that
have
agreement
with
regard
to
sexual
relations
are
happier
and
can
ignore
many
life
problems
(46).
One
of
the
main
fundamental
methods
to
achieve
this
healthy
sexual
behavior
is
providing
appropriate
education.
Research
in
this
field
shows
that
sexual
skills
training
is
effective
on
health
behaviors
and
can
improve
understanding
of
persons
about
sexual
issues
(47).
Perhaps
the
reason
for
significant
effect
of
sexual
skills
training
on
sexual
dysfunction
in
infertile
women
is
that
the
need
of
such
patients
for
such
training
to
resolve
problems
in
sexual
function
which
existed
long
ago
or
developed
after
infertility
was
diagnosed,
prepared
them
properly
to
implement
this
training.
The
training
provided
a
basis
that
patients
themselves
see
their
relations
beyond
infertility
and
try
to
improve
their
sexual
relations.
Another
issue
that
is
a
strength
in
this
study
that
spouses
of
the
women
were
contacted
and
were
advised
regarding
sexual
dysfunction.
They
were
notified
that
they
should
also
collaborate
in
this
study
and
as
this
study
was
done
in
a
university
center,
they
allowed
their
spouses
to
participate
at
the
study.
The
sessions
were
held
very
regularly
and
this
helped
the
effectiveness
of
the
intervention.
There
are
some
possibilities
in
terms
of
effectiveness
of
sexual
skills
training
with
cognitive-behavioral
therapy
approach
on
sexual
dysfunction.
First,
exercises
used
were
not
merely
physical
ones.
These
sexual
exercises
can
result
in
complex
psychologic
reactions.
For
example,
with
sensory-focus
exercises
not
only
pleasurable
reactions
are
strengthened,
but
also
prevent
unwanted
sexual
tensions.
By
reducing
unpredictable
sexual
tensions
in
couples,
emotional
relations
are
enhanced
by
such
exercises
and
cause
couples
to
be
more
kind
towards
each
other.
Secondly,
the
treatments
used
here
allowed
the
subjects
to
state
their
excitement
freely.
This
free
relation
usually
resolves
anxiety
and
facilitates
subjects’
feelings.
Third,
suppressing
guilty
feelings
or
unconscious
fear
of
enjoyment
and
replacing
prohibiting
cognitions
with
correct
cognitions
can
justify
the
effectiveness
of
the
therapeutic
intervention
studied
here.
When
pregnancy
does
not
occur,
infertile
couples
may
think
that
they
do
not
have
effective
sexual
relation
and
gradually
may
forget
that
sexual
relation
is
mainly
to
address
a
fundamental
need
and
its
ignorance
can
cause
damage
to
their
life
(48).
In
the
current
study,
the
sessions
were
held
only
for
women
in
the
absence
of
their
spouses.
It
is
suggested
that
in
the
future
studies,
such
training
be
held
in
the
presence
of
the
spouses
(couple
therapy)
and
compare
this
with
group
therapy.
The
results
of
this
study
indicated
that
sexual
skills
training
with
cognitive-behavioral
approach
was
effective
on
sexual
dysfunction
among
infertile
women.
We
suggest
that
obstetricians
and
gynecologists,
midwives,
nurses,
and
psychologists
use
this
method
in
addition
to
other
approved
methods.
Treatment
of
sexual
dysfunction
in
infertile
women
is
very
important
by
twofold.
Firstly,
treatment
of
infertility
is
important.
Secondly,
by
treating
sexual
dysfunction,
marital
relations
are
improved.
This
is
an
effective
method
to
avoid
marital
and
familial
conflicts
and
resultant
consequences.
As
married
individuals
have
various
sexual
behaviors
and
patterns,
by
training
couples,
it
is
possible
to
enhance
their
sexual
knowledge
and
make
cognitive
changes.
Acknowledgements
We
thank
all
patients
and
staff
who
helped
us
in
conducting
this
study
1.
Baldur-Felskov
B,
Kjaer
SK,
Albieri
V,
Steding-
Jessen
M,
Kjaer
T,
JohansenC,
et
al.
Psychiatric
disorders
in
women
with
fertility
problems:
results
from
a
large
Danish
register-based
cohort
study.
Hum
Reprod2013;
28:
683-690.
2.
Vahidi
S,
Ardalan
A,
Mohammad
K.
Prevalence
of
primary
infertility
in
the
Islamic
Republic
of
Iran
in
2004-2005.Asia
Pac
J
Public
Health2009;
21:
287-293.
3.
BoivinJ
&Takefman
JE.
Impact
of
the
in-vitro
fertilization
process
on
emotional,
physical
and
relational
variables.
Hum
Reprod
1996;
11:
903-7.
4.
Stephanie
S,
FaubionMD&
Jordan
E.
Rullo,
PhD,
Mayo
Clinic,
Rochester,
Minnesota.
Sexual
Dysfunction
in
Women:
A
Practical
Approach.
Am
Fam
Physician
2015;92(4):281-288.
5.
World
Health
Organization:
WHO.
Developing
sexual
health
programmes:
a
framework
for
action.
Geneva:
World
Health
Organization;
2010.
Available
from:
http://apps.who.int/iris/handle/10665/70501.
6.
Mechanick
Braverman
AN.
Psychological
aspects
of
infertility:
Sexual
dysfunction.
International
Congress
series,
2004;
1266:270-274.
7.
Koochak
Sarai
Ranjbar
F,
Gholizadeh
M
,
Bahrami
N.
Compare
sexual
satisfaction
between
fertile
and
infertile
couples
who
referred
to
hospitals
in
Tabriz
Zahra.
Journal
of
Nursing
and
Midwifery
2006;
5:
47-
56.
8.
Alan
W,
S,
Hinde
L,
Christian
J,
Nelson
Cathy
K,
John
P,
Mulhall.
Sexual
function
and
quality
of
life
in
the
Male
partner
of
Infertile
couple.
Prevalence
and
correlates
of
dysfunction.
Urology
2008;179:1056-1059.
9.
Lenzi
AF,
Lombeerdo
P,
Salacone
L,
Gandini
E
A.
Stress,
sexual
dysfunction,
and
male
infertility.
JEnocrinol
Invest
2003:
26-72.
10.
Noraei
Sadodin
S,
Joneydi
E
,
Shakeri,
M
T
,
Mokhber,
N.
Comparison
of
sexual
satisfaction
in
fertile
and
infertile
governmental
centers
of
the
city
Mashhad.
Journal
of
Reproduction
&
Infertility
2009;
10(4):
269-277.
11.
Nene
UA.
K
&
Coyagi
H
Apte.
Infertility
a
label
of
choice
in
the
case
of
sexuality
dysfunctional
couples.
Patient
Educ
Couns,
2005:59-234.
12.
Burns
LH.
An
overview
of
sexual
dysfunction
in
the
infertile
couple.
J
FamPsychother
1995;6:25-46.
13.
Arruda
JT.
Amaral,
WN.
Mendonça,
CR.Nov.
Sexual
function
in
women
undergoing
assisted
Reproduction
.Rev
Bras
GinecolObstet2014
;36(11):484-488.
14.
Helmer
AE,
Quintero
RB,
Westphal
L
M,
Milki
A
A,
Lathi
RB.
Is
infertility
a
risk
factor
for
female
sexual
dysfunction?
A
case-control
study2010;
94(6):
2022-5
15.
Carter
J.
Applegarth
L,
Josephs
L,
Grill
E,
Baser
RE,
Rosenwaks
Z.
A
cross-sectional
cohort
study
of
infertile
women
awaiting
oocyte
donation:
the
emotional,
sexual,
and
quality-of-life
impact.
FertilSteril
2011;
95(2):711-6.
16.
Alirezaee
S
,
Ozgoli
G,
AlaviMajd,
H
R.
Comparison
of
sexual
self-efficacy
and
sexual
function
in
fertile
and
infertile
women
referred
to
health
centers
in
Mashhad
in
1392.
Pajoohandeh
Journal
2014;
19
(3)
:131-136
17.
Tayebi
N,
Yasini-ardakani
M.
The
prevalence
of
sexual
dysfunction
in
women
of
reproductive
Infertility
Nabarvr.syzdhmyn
Congress.
Specialized
Scientific
Society
of
Reproductive
Infertility
2006.
18.
Jamali
S
,
Zarei
H
,
Jahromi
A
R.
The
relationship
between
body
mass
index
and
sexual
function
in
infertile
women.
Iranian
Journal
of
Reproductive
Medicine
2014;
12(
3):
189-198.
19.
Bakhtiari
A,
Basirat
Z,
Nasiri-Amiri
F.
Sexual
Dysfunction
in
Women
Undergoing
Fertility
Treatment
in
Iran:
Prevalence
and
Associated
Risk
Factors.
J
ReprodInfertil
2015;
17(1):26-33.
20.
Michelson
L
K
,
Marchion
K.
Behavioral
cognitive,
and
pharmacological
treatments
of
panic
disorder
with
agoraphobia:
Critique
and
synthesis.
J
consult
Clipsychol1991;
59:
100
21.
SiggC.
Sexuality
and
sterility.
TherUmsch
1994;
51(2):
115-9.
German.
22.
Andrews
FM,
Abbey
A,
&
Halman
L
J.
(1992).
Is
fertility
problem
stress
different?
The
dynamics
of
stress
in
fertile
and
infertile
couples.
FertilSteril1992;
57:
1247-1253.
23.
World
Health
Organization.
Current
practices
and
controversies
in
assisted
reproduction.
Report
of
a
meeting
on
Medical
Ethical
and
Social
Aspects
of
Assisted
Reproduction.
Geneva:World
Health
Organization:
2002:
128.
24.
Fahimi
Z.
The
impact
of
sex
education,
skills-based
approach
(cognitive-behavioral)
an
increase
in
sexual
satisfaction,
marital
and
treatment
of
depression
and
anxiety
in
women.
Faculty
of
Education
and
Psychology.
Ferdowsi
University
of
Mashhad
2012.
25.
Spence
SH.
Psychosexual
Therapy:
A
Cognitive
–Behavioural
Approach,
London,
Chapman
and
Hall
1991.
26.
Nobre
PJ&
Pinto-Gouveia
J.
Dysfunctional
sexual
beliefs
as
vulnerability
factors
for
sexual
dysfunction.
J
Sex
Res
2006
;43(1):68-75.
27.Tavakkolizadeh
J,
Haji
authority
N
Sadat.
Cognitive-behavioral
effect
of
education
on
sexual
dissatisfaction
in
women
with
low
sex
work.
University
of
Medical
Sciences
2013:
21(5).
28.
Tuschen-Caffier
B,
Florin
I,
Krause
W,
Pook
M..Cognitive-behavioral
therapy
for
idiopathic
infertile
couples.
PsychotherPsychosom
1999;
68(1):
15-21.
29.
Forotan
SK,
MB
Taghavi
MH.
The
Role
of
sexual
health
Iranian
family.
Journal
judgment,
August
and
September
2011;71:
33
28.
30.
Stulhofer
A,
Gregurovic
M,
Pikic
A,
Galic
I.
Sexual
problems
of
urban
women
in
Croatia:
prevalence
and
correlates
in
a
community
sample.
Croat
Med
J
2005
Feb;46(1):45-51
31.
Rosen
R,
Brown
C,
Heiman
J,
Leiblum
S,
Meston
C,
Shabsigh
R,
D’Agostino
R.
Female
sexual
function
index
(FSFI):
A
multidimensional
self-report
instrument
for
the
assessment
of
female
sexual
function.
Journal
of
Sex
&
Marital
Therapy
2000;
26:
191-208.
32.
Mohammadi
Kh
,
Heydari
M
,
Faghihzadeh
S.
Validity
of
the
Persian
version
of
the
Female
Sexual
Function
Index-FSFI
as
Female
Sexual
Function
Index.
Payesh
Journal
2005;
7(3):
269-278.
33.
Azartash
F.
Training
sexual
skills
to
resolve
conflicts.
Master’s
thesis.
Clinical
Psychology,
Islamic
Azad
University
of
Tehran
Research
2011.
34.
McCabe
MP.
Evaluation
of
a
cognitive
behavior
therapy
program
for
people
with
sexual
dysfunction,
Journal
of
Sexual
Marital
Therapy
2001;
27(3):
259-71.
35.
Kabakci
E,
&
Batur
S.
Who
benefits
from
cognitive
behavioral
therapy
for
vaginismus?
Journal
of
Sex
Marital
Therapy
2003;
29(4):
277-88.
36.
Turkuile
MM,
Vanlankveld
JJ,
Groot
ED,
Melles
R,
Neffs
J
&
Zandbergen
M.
Cognitive-behavioral
therapy
for
women
with
lifelong
vaginismus:
process
and
prognosis
factors,
Behavioral
Research
and
therapy
2007;45(2):
359-73
37.
Nobre
PJ,
Pinto-Gouveia
J.
Dysfunctional
sexual
beliefs
as
vulnerability
factors
for
sexual
dysfunction.
J
Sex
Res
2006;43(1):
68-75.
38.
Nobre
PJ,
Pinto-Gouveia
J,
Cognitive
Schema
Activation
in
Sexual
Context:
A
Questionnaire
to
Assess
Cognitive
Schemas
Activated
in
Sexual
Failure
Situations.
J
Sex
Res
2008;
15(3):
175-89.
39.
Pakgohar
M,
Vizheh
M,
BabaeeGh
,
Ramezanzadeh
F,
Abedininia
N
.
Effect
of
Counseling
on
Sexual
Satisfaction
among
Infertile
Women
Referred
to
Tehran
Fertility
Center.
Journal
of
Faculty
of
Nursing
and
Midwifery,
Tehran
University
of
Medical
Sciences
2008;
14(1):
21-30
40.
Etemadi
A,
Navaabi
NejadSh,
Ahmadi
A,
Farzad
V.
The
Effect
of
Cognitive
Behavioral
Couple
Therapy
on
Couple’s
Intimacy
of
Isfahan.
J
psychological
studying2004;
2(1):15_29.
41.
Salehzadeh
M,
Kajbaf
MB,
Molavi
H
,
Zolfaghari
H.
The
effectiveness
of
cognitive-behavioral
therapy
on
sexual
dysfunction
in
women.
University,
Faculty
of
Education
and
psychology
2011;
7(1).
42.
Ziaee
P,
Sepehri-shamlou
Z,
Mashhadi
A.
The
Effectiveness
of
Sexual
Education
Focused
on
Cognitive
Schemas,
on
the
Improvement
of
Sexual
Functioning
among
Female
Married
Students.
Journal
of
Evidence-based
Care
2014;
4(11).
43.Crespo
E
&
Fernandez
F.
Cognitive
Behavioural
treatment
of
a
case
of
vaginism
and
phobia
about
pelvic
examination,
Journal
of
psychology
2004:106-121.
44.
Tuschen-Caffier
B,
Florin
I,
Krause
W,
Pook
M.
Cognitive-behavioral
therapy
for
idiopathic
infertile
couples.
Psychother
Psychosom1999;68(1):15-21.
45.
Smith
M
A,
&Shimp
L
A.
20
Common
problems
in
women’s
health
care.
New
York:
McGaw
Hill.
2000.
46.
Lawrence
K,
&
Bycrs
E
S.
Sexual
Satisfaction
in
Long
term
heterosexual
relationship:
The
interpersonal
exchange
model
of
sexual
Satisfaction.
Personal
Relationships
1995;2:
267-285
47.
Olson
D
H.
Circumcises
model
of
marital
and
family
systems:
The
association
for
family
therapy.
Philadelphia:
Black-Well,
2010.
48.
Bokaie
M,
Simbar
M,
Yassini
Ardekani
S.
Sexual
behavior
of
infertile
women:
A
qualitative
study.
Iran
J
Reprod
Med
2015;13(10):645-656.
|
|
.................................................................................................................

|
| |
|

