|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
........................................................
In Memoriam
Professor
Orhan Ekrem Müftüoglu
|
........................................................
Original
Contribution / Clinical Investigation
|







|
Cholelithiasis
and cholecystectomy may lower the low density
lipoprotein cholesterol in plasma
DOI: 10.5742/MEWFM.2017.93010
[pdf
version]
Mehmet Rami Helvaci, Mursel Davarci, Orhan Veli
Ozkan, Ersan Semerci, Abdulrazak Abyad, Lesley
Pocock
Serum
and follicular fluid vitamin D and follicular
response among infertile women undergoing ICSI
DOI: 10.5742/MEWFM.2017.93011
[pdf
version]
Sedighe Esmaeilzadeh, Maryam Aliasgharpour,
Parvaneh Mirabi, Azita Ghanbarpour
Maede Fasihian
Studying
the relation of quality of work life with socio-economic
status and general health among the employees
working in Students Welfare Fund of Ministry
of Health and Medical Education in 2016
DOI: 10.5742/MEWFM.2017.93012
[pdf
version]
Saeed Reza Azami, Nasrin Shaarbafchizadeh, Soheil
Mokhtari, Ali Maher
On the Effect
of Cognitive Behavioural Counseling on Sexual
Satisfaction of Mothers with Autistic Children:
A Randomized Clinical Trial
DOI:
[pdf version]
Leila Arbil, Mitra Kolivand, Farzaneh Golboni,
Effat MerghatiKhoei, Mansour Rezaei
Pre-operative
sublingual misoprostol and intra-operative blood
loss during total abdominal hysterectomy: a
randomized single-blinded controlled clinical
trial
DOI: 10.5742/MEWFM.2017.93013
[pdf
version]
Taravat Fakheri, Tayebe Noori
Investigating
the Effect of Endotracheal Tube Cuff Pressure
on Sore Throat, Hoarseness and Cough in Patients
with Coronary Artery Bypass Surgery
DOI: 10.5742/MEWFM.2017.93014
[pdf
version]
Ali Akbar Vaezi, Mohammad Hassan Mondegari Bamakan
Comparing
the Self-Esteem and Resiliency between Blind
and Sighted Children and Adolescents in Kermanshah
City
DOI: 10.5742/MEWFM.2017.93015
[pdf
version]
Saeedeh Bakhshi, Nafiseh Montazeri , Babak Nazari,
Arash Ziapour, Hashem Barahooyi,
Fatemeh Dehghan
|
........................................................
Population
and Community Studies
|







|
Frequency
of Uric Acid Levels, Symptomatic and Asymptomatic
Hyperuricemia among the Pakistani Population
DOI: 10.5742/MEWFM.2017.93016
[pdf
version]
Waris Qidwai, Masood Jawaid
Determinants
of Tooth Brushing among Primary School Students
DOI: 10.5742/MEWFM.2017.93017
[pdf
version]
Mohammad Mahboubi, Mohammad Ismail Motlagh,
Mehdi Mirzaei-Alavijeh, Farzad Jalilian, Hassan
Gharibnavaz,
Mohammad Fattahi
Depression
in patients suffering from gender dysphoria:
The hospitalized patients of Legal Medicine
Center in Southwest of Iran
DOI: 10.5742/MEWFM.2017.93018
[pdf
version]
Zahra Gorjian, Mohammad Zarenezhad, Mohhamad
Mahboubi, Saeid Gholamzadeh,
Nahid Mahmoodi
An epidemiological
study of suicide attempts and to determine the
correlation between attempted suicide causes
and demographic characteristics of people in
Kermanshah Province during a year
DOI: 10.5742/MEWFM.2017.93019
[pdf
version]
Hamid Reza Shetabi, Samira Rostami, Mohsen Mohammadi,
Mahsa Cheleii, Lida Saedi, Saba Amiri Nasab,
Shirin Zardui GolAnbari
The
effectiveness of life skills training on happiness,
mental health, and marital satisfaction in wives
of Iran-Iraq war veterans
DOI: 10.5742/MEWFM.2017.93038
[pdf
version]
Kamal Solati
The
Role of Self-Compassion Factors in Predicting
the Marital Satisfaction of Staff at Kermanshah
University of Medical Sciences
DOI:10.5742/MEWFM.2017.93020
[pdf
version]
Parisa Janjani, Lida Haghnazari, Farahnaz Keshavarzi,
Alireza Rai
Mediating
role of irrational beliefs in the relationship
between the quality of family communication
and marital satisfaction
DOI:10.5742/MEWFM.2017.93021
[pdf
version]
Parisa Janjani, Khodamorad Momeni, Alireza Rai,
Mohammad Reza Saidi
|
........................................................
Review Article
........................................................
International Health
Affairs
........................................................
Education
and Training
........................................................
Clinical
Research and Methods
|





|
Adaptive
LASSO Logistic Regression applied on gene expression
of prostate cancer
DOI: 10.5742/MEWFM.2017.93028
[pdf version]
Amir Hossein Hashemian, Maryam Ghobadi Asl,
Soodeh Shahsavari, Mansour Rezaei,
Hadi Raeisi Shahraki
The
prevalence of brain and neck injuries in patients
with maxillofacial fractures in teaching hospitals
of Rasht in 2016
DOI: 10.5742/MEWFM.2017.93029
[pdf
version]
Seyed Mohammad Talebzadeh, Ali Khalighi Sigaroudi,
Babak Alijani, Safa Motevasseli,
Saied Dashtyari, Mahsa Shariati, Zeinab Davoudmanesh
Cultural
competency: a concept analysis in TUMS (Tehran
University of Medical Science) DOI:
10.5742/MEWFM.2017.93030
[pdf version]
Foruzan Khatamidoost, Mandana Shirazy, Hamid
Khankeh, Nemat Allah Musapour
Majid Sadeghi, Kamran Soltani Arabshahi
The
Effect of Proprioceptive Neuromuscular Facilitation
(PNF) on Activities of Daily Living of client
with Cerebrovascular accident
DOI: 10.5742/MEWFM.2017.93031
[pdf
version]
Najafi Doulatabad Shahla, Afrasiabifar Ardashir,
Parandvar Yaghoub
Evaluation
of the ratio of T helper 17 and T regulatory
cells in patients with chronic idiopathic urticaria
DOI: 10.5742/MEWFM.2017.93032
[pdf
version]
Hossein Shahriari, Farahzad Jabbari, Seyyed
Abdolrahim Rezaee, Houshang Rafatpanah
Majid Jafari, Reza Farid Hosseini, Majid Asadi-Samani
|
........................................................
Model
and System of Primary Care
........................................................
Case
Series and Case Reports
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| September 2017
- Volume 15, Issue 7 |
|
|
New Methods in Treatment
of Renal failure in Patients with Multiple Myeloma:
A Review with Immunological Approach
Ali Saeedi-Boroujeni (1)
Sara Iranparast (1, 2)
Majid Shirani (3)
Tahra Luther (4)
(1) Student Research Committee, Ahvaz Jundishapur
University of Medical Sciences, Ahvaz, Iran;
(2) Medical Plants Research Center, Basic Health
Sciences Institute, Shahrekord University of
Medical Sciences, Shahrekord, Iran;
(3) Cellular and Molecular Research Center,
Basic Health Sciences Institute, Shahrekord
University of Medical Sciences, Shahrekord,
Iran;
(4) Department of General Surgery, University
of Michigan, Ann Arbor, Michigan.
Correspondence:
Majid Shirani; MD; Basic Health Sciences Institute,
Shahrekord University of Medical Sciences,
Shahrekord, Iran
Email: biology_2011@yahoo.com.
|
Abstract
Multiple myeloma
(MM), as one of a variety of autoimmune
diseases, affects the immune system and,
on the other hand, is considered to be
a hematologic impairment. One of the most
common and important complications of
MM is renal impairment (RI), which is
associated with an increase in serum Cr
levels. Although RI is one of the major
complications of MM, the routine therapies
for MM patients practically lack acceptable
efficacy for the improvement of RI patients,
and as a result, RI remains a deadly disease
with high mortality rate and very bad
prognosis; therefore, new treatments have
been proposed for the improvement of nephropathy
in patients with MM, and extensive research
is ongoing in various phases, including
clinical trials. Attempts were made in
this study to review common and advanced
treatments (immunotherapy, cell therapy,
new therapies based on genetic engineering)
in these patients and to consider this
disease from an immunological viewpoint.
Key words:
Multiple myeloma, renal impairment, Immunomodulatory
drugs
|
The immune system is the body’s natural
defense against infection and malignant diseases.
However, sometimes its responses can cause autoimmune
diseases (1-7). Multiple Myeloma (MM) is one
types of autoimmune diseases associated with
B cells and plasma cells are highly proliferated
and IgG antibody is produced at high levels
in serum and urine. It alone accounts for 10%
of all hematologic malignancies. The disease
affects people’s immune system and, is
also considered as a hematological defect. The
disease mainly involves the elderly (8) so that
the average age of people involved with MM is
65 years (9). This disease is more common in
men and the prevalence of this disease in Africa
and the United States is twice as high as in
Europe. One of the most common and important
complications of MM is renal impairment (RI),
which is associated with an increase in serum
creatinine levels. RI is seen in 20-40% of patients
newly diagnosed with MM (NDMM) and 25% of patients
(RRMM) and / or refractory multiple myeloma
with relapsed symptoms and creatinine levels
increases to above 4 mg/ml in most people with
this condition (10). MM begins with acute kidney
injury (AKI), and recurrence is associated with
nephropathy casts.
|
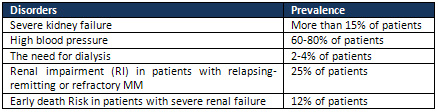
PREVALENCE OF RI IN PATIENTS WITH MM |
RI is seen in half of the patients with MM.
Severe RI is also seen in more than 15% of these
patients. Table 1 presents the prevalence of
all types of disorders involved in this disease.
Today for prevention and treatment most disorders
such as urinary system dysfunctions have been
evaluated and new drugs and methods and their
outcomes have been considered (11-19). Since
routine therapies for patients with MM have
virtually no acceptable efficacy for the improvement
of RI patients and RI is still considered as
a disease with high mortality and very bad prognosis;
new treatments have been proposed for the improvement
of nephropathy in patients with MM. In this
study, attempts were made to review common and
advanced treatments (immunotherapy, -cell therapy
and new therapies based on genetic engineering)
and discuss this disease from an immunological
viewpoint.
Table 1: Prevalence of some types of defects
and RI in patients with MM
|
MECHANISMS OF NEPHROPATHY SYMPTOMS IN PATIENTS
WITH MM |
Renal
damages
in
patients
with
MM
mostly
occur
due
to
the
toxic
effect
of
the
free
light
chain
(FLC).
Light
chains
are
proteins
produced
by
plasma
cells.
Within
a
plasma
cell,
two
light
chains
and
two
heavy
chains
are
combined
to
form
an
immunoglobulin.
The
free
light
chain
is
filtered
through
the
glomeruli
and
is
removed
and
catabolized
by
the
cells
of
the
proximal
tubule
cells
(PTCs).
The
FLC
level
in
the
serum
of
patients
with
MM
can
be
increased
up
to
100
times,
which
indicates
the
high
ability
of
PTCs
cells
in
absorbing
and
catabolizing
these
proteins,
which,
as
a
result
of
increased
activity
of
these
cells,
leads
to
an
increase
in
the
concentration
of
FLC
in
the
urine
and
fluid
in
the
tubule
of
the
kidney(20).
Urinary
FLC
has
a
high
affinity
for
binding
to
the
carbohydrate
portion
of
(THP),
which
causes
aggregates
that
cause
cysts
and
blockage
of
renal
tubules(21).
FLC
can
activate
inflammatory
pathways
and
cause
fibrosis
in
the
tubular
area
during
inflammation
in
cells
in
the
tubule
(20).
Also,
various
factors,
including
nonsteroidal
anti-inflammatory
compounds,
dehydration,
acidosis,
and
angiotensin
converting
enzyme
(ACE)
inhibitors
interfere
with
the
onset
of
RI
and
contribute
to
the
nephropathy
caused
by
FLC.
On
the
other
hand,
factors
like
hypercalcium
may
further
aggravate
the
symptoms
of
nephropathy
(10,
22,
23)(Figure
1).
Click
here
for
Figure
1:
Mechanisms
involved
in
RI-caused
MM
1.
Common
MM
Therapies:
1-1
Primary
Care
Support
In
case
of
transient
but
recurrent
defects
in
the
kidney,
especially
in
people
who
excrete
plenty
of
Bence
Jones
protein,
immediate
supportive
treatments
have
been
taken
for
patients
for
whom
combination
of
bortezomib
and
dexamethasone
is
a
good
therapeutic
option.
And
in
limited
cases,
thalidomide
is
also
prescribed.
Lenalidomide
is
another
low-dose
drug
that
can
control
and
treat
the
symptoms
of
nephropathy
in
patients
with
MM(24).
In
addition,
plasma
replacement
has
been
suggested
as
a
treatment
for
nephropathy
in
patients
with
MM.
However,
the
use
of
this
treatment
is
controversial
in
RI
people
suffering
from
excretion
of
Bence
Jones
protein.
1-2.
Corticosteroids
(dexamethasone)
and
conventional
chemotherapy
Dexamethasone
is
one
of
the
cortical
derivatives
that
plays
an
important
role
in
improving
nephropathy
in
patients
with
MM.
A
high
dose
of
dexamethasone
leads
to
a
higher
rate
of
kidney
regeneration
activity
in
MM
patients
who
have
recently
suffered
RI.
It
is
also
prescribed,
independently
of
dialysis,
for
patients
with
kidney
complications
and
high
risk
of
severe
proteinuria,
which
discharges
Bence
Jones
at
high
levels
in
the
urine
(25).
In
addition,
the
new
drug
combination
of
thalidomide+bortezomib
is
safe
in
the
treatment
of
nephropathy
in
patients
with
MM,
leading
to
renal
function
improvement.
However,
the
use
of
dexamethasone
and
chemotherapy
is
recommended
for
effective
treatment
of
nephropathy
in
these
individuals
(25-27).
2.
New
treatments
and
advanced
drugs:
Over
the
last
decade,
there
has
been
a
major
advance
in
MM
treatment
and
new
and
advanced
therapies
were
later
used
for
the
treatment
of
transplant
recipients
as
well
as
those
who
were
not
eligible
for
transplantation
(28)
and
considering
their
effectiveness,
the
probability
of
complete
responses
(CR),
progression
of
disease,
disease-free
survival
(PFS)
and
total
survival
(OS)
have
been
increased.
Combined
therapeutic
approaches,
including
dietary
regimens
and
chemotherapy,
have
been
proposed
as
a
standard
treatment
approach,
which
can
be
done
in
both
the
ASCT
patients
as
well
as
patients
who
do
not
intend
organ
transplants(29).
The
new
therapeutic
approaches
and
advanced
drugs
that
are
introduced
and
presented
in
this
effort
are
presented
in
more
detail
as
follows.
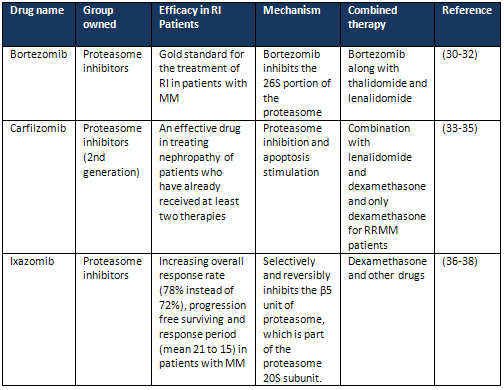
2.1
Proteasome
inhibitors
Proteasome
inhibitors
have
been
able
to
significantly
advance
the
progression
of
MM
disease
independently
of
organ
transplants.
Some
of
the
new
anti-MM
drugs,
the
mechanism
of
action
of
which
is
proteasome
inhibition
are
listed
in
Table
2.
Table
2:
New
anti-
MM
drugs
the
mechanism
of
action
of
which
is
proteasome
inhibition
2.2
Immunomodulatory
drugs
Immunomodulatory
drugs
(IMiDS)
directly
affect
multiple
myeloma
cells
and
bone
marrow
environments,
leading
to
changes
in
cytokines,
inhibition
of
angiogenesis,
and
increased
number
and
function
of
various
cells,
including
T,
NK,
and
NKT.
IMiDs
are
also
capable
of
replicating
Treg
cells.
In
addition,
IMiDs
can
enhance
the
ADCC
defense
response
in
NK
cells
by
increasing
expression
of
FasL
and
granzymes.
Considering
this
feature,
IMiDs
can
be
used
in
targeted
therapies
for
immunotherapy(39).
As
indicated
in
the
mechanism
section,
inflammatory
response
is
one
of
the
effective
factors
in
the
progression
and
treatment
process.
Therefore,
this
group
of
drugs
can
effectively
and
potentially
contribute
to
the
treatment
of
MM
patients
(Table
3).
Given
that
immunomodulators
include
a
wide
range
of
therapeutic
strategies,
some
of
the
most
recent
and
most
important
ones
are
mentioned
here,
and
some
of
them
are
listed
in
Table
3.
Click
here
for
Table
3:
Some
immunomodulatory
drugs
for
the
treatment
of
multiple
myeloma
2-2-1
-
Bispecific
T
cell
engages
(Bi-TEs)
BiTEs
are
a
novel
immunotherapy
approach
in
relation
to
antibodies
and
T
cells.
This
method
enables
us
to
design
antibodies
using
genetic
engineering,
which
is
in
contrast
to
the
usual
dual
specificity.
For
example,
the
antibody
is
designed
in
such
a
way
that,
on
the
one
hand,
as
a
specific
marker
of
T
lymphocytes
for
CD3
and
as
a
specific
marker
for
CD19
on
the
surface
of
the
cells
of
the
lymphoma,
on
the
other
hand.
Thus,
a
tumor
cell
with
T
lymphocyte
(as
the
main
anti-tumor
cell)
will
be
placed
next
to
each
other,
resulting
in
the
destruction
of
tumor
cells
at
higher
intensity.
BiTEs
have
been
investigated
for
the
treatment
of
melanoma
in
vitro
and
in
vivo
and
satisfactory
results
were
also
obtained.
2-2-2
Adoptive
T
cell
Therapies
(ACT)
In
this
method,
the
T-cell
of
a
person
with
MM
is
isolated
from
its
whole
blood,
and
these
cells
lead
to
the
activation
and
development
of
T-cells
in
the
presence
of
anti-CD3-CD28
beads
and
IL2
in
the
ex-vivo
environment
and
after
being
discharged
from
the
bone
marrow
from
the
myeloid
line
and
the
autologous
transplantation,
this
ex-vivo
amplified
compound
is
inoculated
and
leads
to
primary
lymphocytosis.
Recently,
this
method
has
also
been
used
for
the
first
time
in
the
production
of
bone
marrow
infiltrated
t
lymphocytes
(mILs)
as
clinical
anti-tumor
immunity
(40).
The
results
of
this
treatment
are
satisfactory,
but
more
confirmation
is
needed
in
this
regard.
2-2-3
TCR
transgenic
T
cells
In
this
method,
TCR
infusion
occurs
with
high
affinity
and
common
peptide
antigens
between
two
types
of
cancer
(NY-ESO-1,
LAGE-1)(41).
Initial
laboratory
tests
indicate
that
the
infusion
T
cell,
the
function
of
which
is
actively
maintained,
occurs
and
these
cells
remain
active
in
the
body
and
in
the
presence
of
IL2
without
fatigue
for
up
to
one
year.
On
the
other
hand,
all
people
with
MM
are
being
treated
to
respond
to
HLA-dependent
treatment.
Nevertheless,
these
cells
are
HLA-dependent
and
therefore,
this
is
a
therapeutic
constraint
compared
to
the
CART
method(25).
2-2-4
BTK
inhibitors
Bruton
Tyrosine
kinase
is
an
enzyme
from
the
Tec
family
that
is
expressed
in
hematopoietic
cells
such
as
B
and
myeloid
cells,
mast
cells,
and
platelets,
and
plays
a
key
role
in
several
important
cellular
processes,
including
differentiation,
proliferation,
cell
migration
and
apoptosis(42,
43).
In
the
case
of
mutation
in
the
BTK
gene,
the
maturation
of
these
cells
is
impaired
and
genetic
and
hereditary
diseases
such
as
XLA
(X-linked
gamma-globulinemia)
are
created(44).
On
the
other
hand,
the
excessive
activity
of
BTK
refers
to
the
neoplasm
associated
with
B
cells(45).
Ibrutinib
is
one
of
the
drugs
produced
in
this
field
and
is
capable
of
inhibiting
the
function
of
this
enzyme
during
the
binding
of
covalent
to
BTK
and
its
administration
alone
or
in
combination
with
other
drugs
can
provide
satisfactory
therapeutic
results.
In
a
study
in
2015,
a
combination
of
Ibrutinib
and
Carfilzomib
with
or
without
dexamethasone
was
used
to
treat
RRMM
patients
and
a
target
response
rate
of
62%
was
reported(46).
The
effect
of
BTK
expression
in
the
treatment
of
the
disease
is
so
important
that
there
are
many
solutions
to
inhibit
the
expression
of
this
enzyme,
which
can
have
a
significant
effect
on
the
treatment
process.
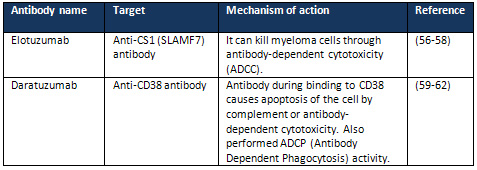
2.3
Monoclonal
Antibodies
Therapies
performed
based
on
monoclonal
antibodies
against
target
antigen
have
been
defeated
due
to
the
lack
of
clear
expression
of
the
target
molecule
on
the
plasma
cells.
In
fact,
early
studies
have
only
shown
the
minimal
activity
of
anti-CD20,
which
is
expressed
in
20%
of
plasma
cells.
Studies
have
also
been
conducted
on
several
other
monoclonal
antibodies
(anti
[TRAIL-R1,
IL6,
CD38,
CD138,
CD74,
CS1,
CD56,
IGF-1R,
CD40]),
among
which
two
monoclonal
antibodies,
Elotuzumab
and
Daratuzumab,
is
important
and
practical
in
MM
disease
(Table
4).
In
addition,
B
cell
maturation
antigen
(BCMA)
antibodies
are
under
construction
and
its
clinical
trial
is
in
progress.
BCMA,
a
superfamily
protein
TNFR,
is
used
as
an
important
target
in
the
construction
of
monoclonal
antibodies
and
can
be
of
great
help
in
treating
patients
with
MM.
On
the
other
hand,
the
production
of
antibodies
against
CD138,
CD56
and
CD74
is
also
under
investigation
in
the
early
stages
of
clinical
practice
(25).
Table
4:
Monoclonal
antibodies
approved
by
the
FDA
for
patients
with
MM
2.4
High-dose
therapy
and
autologous
stem
cell
transplantation
(HDT
&
ASCT)
ASCT
(Post-autologous
Stem
Cell
Transplant
Therapy)
is
one
of
the
supportive
therapies
that
is
used
for
MM
patients
during
a
12-month
period
(63-66),
leading
to
improved
OS
and
better
treatment
outcomes)
during
the
transplantation
process.
The
ASCT
method
is
applicable
to
all
eligible
MM
patients.
In
this
therapeutic
approach,
following
a
stem
cell
transplant,
3-4
courses
of
the
drug
regimen,
including
bortezomib
and
dexamethasone
in
combination
with
lenalidomide,
thalidomide,
or
cyclophosphamide,
is
received
by
the
patient(67).
The
administration
of
this
therapeutic
approach
helps
patients
maintain
their
condition
for
a
progressive
free
survival
(PFS)(68,
69).
In
addition,
bortezomib’s
mechanism
of
action,
which
is
to
inhibit
proteasome,
helps
to
create
better
PFS
in
MM
patients
with
intermediate
and
high-risk;
however,
the
post-ASCT
administration
of
this
drug
compared
with
thalidomide,
which
has
toxic
effects
in
the
blood,
offers
better
treatment
outcomes.
Since
the
relapse
of
the
disease
occurs
almost
entirely
in
MM
patients,
the
relapse
period
can
be
changed
from
2.5
years
to
4
years
(70,
71).
2.5
Plasma
exchange
The
kappa
and
lambda
chains
of
FLC,
which
have
a
molecular
weight
of
45KD
and
22.5KD,
respectively,
are
excreted
from
the
renal
glomeruli
after
a
half-life
of
3
and
6
hours.
Consequently,
anti-myeloma
effects
are
induced
in
individuals
through
the
“plasma
replacement”
and
FLC
levels
are
also
reduced.
Interestingly,
patients
who
receive
this
treatment
are
protected
against
other
kidney
injuries
that
may
occur
in
the
future
(72).
Additionally,
the
combination
of
plasma
replacement
therapy
with
bortezomib-based
therapies
gives
rise
to
strong
responses
in
all
NDMM
and
RRMM
patients
(73).
Plasma
replacement
in
the
short
term
leads
to
the
purification
of
proteins
in
the
extravascular
part,
but
in
any
case,
the
plasma
replacement
in
the
long
run
leads
to
the
purification
of
other
essential
proteins;
therefore,
the
use
of
membranes
have
cut-off
for
higher
molecular
weight
proteins,
can
be
a
remedy
in
this
case
(74).
2.6
Renal
transplantation
One
of
the
treatment
methods
for
MM
patients
involved
with
RI
is
renal
transplantation,
which
can
be
used
as
a
treatment
alternative
for
these
patients,
due
to
the
increasing
number
of
patients.
The
results
of
a
study
which
was
conducted
on
166
patients
in
2013
showed
that
the
risks
of
immunosuppression
should
be
considered
in
those
who
received
ASCT
and
kidney
allograft
transplants,
and
eventually
26
of
them
survived
without
the
need
for
dialysis
(10,
75).
2.7
Histone
deacetylases
(HDACs)
HDACs
deacetylates
lysine
residues
(tails)
in
both
histone
and
non-histone
proteins.
This
enzyme
in
the
chromatin
structure
creates
a
local
relaxation
and
regulates
the
specific
expression
of
the
gene.
HDACs
acts
nonspecifically
and
can
deacetylate
non-histone
proteins
that
is
also
intended
to
alter
the
activity
and
sustainability
of
their
activity,
so
the
inhibitory
effect
of
this
enzyme
complex
on
the
treatment
of
multiple
myeloma
is
very
important
(76)
and
specifically
the
combination
of
inhibitors
of
HDACs
and
proteasome
or
immunomodulatory
drugs
play
a
very
important
role
in
the
progression
of
this
disease
in
pre-clinic
and
clinical
phases.
However,
clinical
studies
that
are
performed
using
selective
HDACs
inhibitors
reduce
the
side
effects
of
treatment,
which
leads
to
increased
tolerance
in
patients
and
has
no
negative
effect
on
the
multiple
myeloma
activity;
therefore
satisfactory
outcomes
were
obtained
when
this
treatment
was
performed
(77).
Panobinostat
is
a
deacetylase
inhibitor
that
can
produce
better
treatment
outcomes
in
combination
with
dexamethasone
and
bortezomib.
Inhibiting
HDACs
activity
leads
to
an
increase
in
acetylated
histone
proteins,
as
a
result
of
this
epigenetic
change,
eventually
during
the
formation
of
the
chromatin
regimen
results
in
the
activation
of
the
transcriptional
process
in
individuals
(78,
79).
Vorinostat
is
another
oral
deacetylase
inhibitor
that
is
effective
in
treating
cutaneous
T-cell
lymphoma
(CTCL)
(80).
Therefore,
both
panobinostat
and
vorinostat
are
involved
during
the
inhibition
of
deacetylation
in
treatment
of
multiple
myeloma.
The
panobinostat
is
so
important
in
the
treatment
of
these
patients
that
it
is
prescribed
in
combination
with
dexamethasone
and
bortezomib
for
RRMM
patients
who
have
received
at
least
two
therapy
y
lines
in
the
past
(80,
81)and
have
shown
resistance
and
this
therapeutic
pattern
was
approved
by
the
FDA
in
February
2015.
Multiple
myeloma
is
a
hematologic
malignancy
that
alone
accounts
for
10%
of
all
hematologic
malignancies.
One
of
the
main
complications
of
the
disease,
which
is
seriously
problematic,
is
high
mortality
and
a
lack
of
satisfactory
effect
of
the
common
treatments
intended
for
this
group
of
patients.
So,
in
the
last
decade,
extensive
researches
and
studies
have
been
carried
out
to
produce
new
drugs;
therefore,
many
drugs
could
help
with
the
treatment
of
patients
with
multiple
myeloma
by
obtaining
approval
from
the
FDA.
Meanwhile,
drugs
that
affect
the
immune
system
of
the
human
body,
namely
immunotherapies,
are
extremely
important.
1.
Bagheri
N,
Azadegan-Dehkordi
F,
Rahimian
G,
Rafieian-Kopaei
M,
Shirzad
H.
Role
of
Regulatory
T-cells
in
Different
Clinical
Expressions
of
Helicobacter
pylori
Infection.
Arch
Med
Res.
2016;47(4):245-54.
2.
Bagheri
N,
Shirzad
H,
Elahi
S,
Azadegan-Dehkordi
F,
Rahimian
G,
Shafigh
M,
et
al.
Downregulated
regulatory
T
cell
function
is
associated
with
increased
peptic
ulcer
in
Helicobacter
pylori-infection.
Microbial
pathogenesis.
2017;110:165-75.
3.
Bagheri
N,
Azadegan-Dehkordi
F,
Rahimian
G,
Hashemzadeh-Chaleshtori
M,
Rafieian-Kopaei
M,
Kheiri
S,
et
al.
Altered
Th17
Cytokine
Expression
in
Helicobacter
pylori
Patients
with
TLR4
(D299G)
Polymorphism.
Immunol
Invest.
2016:1-11.
4.
Bagheri
N,
Azadegan-Dehkordi
F,
Shirzad
H,
Rafieian-Kopaei
M,
Rahimian
G,
Razavi
A.
The
biological
functions
of
IL-17
in
different
clinical
expressions
of
Helicobacter
pylori-infection.
Microbial
pathogenesis.
2015;81:33-8.
5.
Razavi
A,
Bagheri
N,
Azadegan-Dehkordi
F,
Shirzad
M,
Rahimian
G,
Rafieian-Kopaei
M,
et
al.
Comparative
Immune
Response
in
Children
and
Adults
with
H.
pylori
Infection.
J
Immunol
Res.
2015;2015:315957.
6.
Bagheri
N,
Azadegan-Dehkordi
F,
Shirzad
M,
Zamanzad
B,
Rahimian
G,
Taghikhani
A,
et
al.
Mucosal
interleukin-21
mRNA
expression
level
is
high
in
patients
with
Helicobacter
pylori
and
is
associated
with
the
severity
of
gastritis.
Centr
Eur
Immunol.
2015;40(1):61-7.
7.
Ghatreh-Samani
M,
Esmaeili
N,
Soleimani
M,
Asadi-Samani
M,
Ghatreh-Samani
K,
Shirzad
H.
Oxidative
stress
and
age-related
changes
in
T
cells:
is
thalassemia
a
model
of
accelerated
immune
system
aging?
Central-European
journal
of
immunology.
2016;41(1):116-24.
8.
R.
A.
Kyle
,
S.
V.
Rajkumar.
Drug
therapy:
multiple
myeloma.
2004;351(18):1860-921.
9.
Kyle
RA,
Gertz
MA,
Witzig
TE,
Lust
JA,
Lacy
MQ,
Dispenzieri
A,
et
al.,
editors.
Review
of
1027
patients
with
newly
diagnosed
multiple
myeloma.
Mayo
Clinic
Proceedings;
2003:
Elsevier.
10.
Kastritis
E,
Terpos
E,
Dimopoulos
MA.
Current
treatments
for
renal
failure
due
to
multiple
myeloma.
Expert
opinion
on
pharmacotherapy.
2013;14(11):1477-95.
11.
Dadkhah
N,
Shirani
M,
Etemadifar
S,
Mirtalebi
M.
The
effect
of
Cornus
mas
in
preventing
recurrent
urinary
tract
infections
in
women:
A
randomized
controlled
trial.
Advanced
Herbal
Medicine.
2016;2(3):39-46.
12.
Eslami
AA,
Rabiei
L,
Abedi
HA,
Shirani
M,
Masoudi
R.
Coping
skills
of
Iranian
family
caregivers’
in
caretaking
of
patients
undergoing
haemodialysis:
A
qualitative
study.
Journal
of
Renal
Care.
2016;43(2):162-71.
13.
Shirani-Boroujeni
M,
Heidari-Soureshjani
S,
Hafshejani
ZK.
Impact
of
oral
capsule
of
Peganum
harmala
on
alleviating
urinary
symptoms
in
men
with
benign
prostatic
hyperplasia;
a
randomized
clinical
trial.
Journal
of
renal
injury
prevention.
2017;6(2):127-31.
14.
Shirani
M,
Davoudian
A,
Sharifi
A.
Retroperitoneal
fibrosis
associated
with
propranolol:
a
case
report;
is
corticosteroid
administration
necessary
after
ureterolysis?
Journal
of
Renal
Injury
Prevention.
2013;2(2):67-9.
15.
Shirani
M,
Raeisi
R,
Heidari-Soureshjani
S,
Asadi-Samani
M,
Luther
T.
A
review
for
discovering
hepatoprotective
herbal
drugs
with
least
side
effects
on
kidney.
Journal
of
nephropharmacology.
2017;6(2):38-48.
16.
Soleimani
MJ,
Shahrokh
H,
Shadpour
P,
Shirani
M,
Arasteh
S.
Impact
of
dialysis
access
fistula
on
cardiac
function
after
kidney
transplantation.
Iranian
Journal
of
Kidney
Diseases.
2012;6(3):198-202.
17.
Mirhoseini
M,
Moradi
MT,
Asadi-Samani
M.
Traditionally
used
Medicinal
Plants
in
the
Treatment
of
Kidney
Stone:
a
Review
on
Ethnobotanical
Studies
in
Iran.
Ambient
Sci.
2016;3(2):16-21.
18.
Asadi-Samani
M,
Moradi
M,
Mahmoodnia
L,
Alaei
S,
Asadi-Samani
F,
Luther
T.
Traditional
uses
of
medicinal
plants
to
prevent
and
treat
diabetes;
an
updated
review
of
ethnobotanical
studies
in
Iran.
J
Nephropathol.
2017;6(3):118-25.
19.
Heidari-Soreshjani
S,
Asadi-Samani
M,
Yang
Q,
Saeedi-Boroujeni
A.
Phytotherapy
of
nephrotoxicity-induced
by
cancer
drugs:
An
updated
review.
Journal
of
Nephropathology.
2017;6(3):254-63.
20.
Basnayake
K,
Stringer
SJ,
Hutchison
CA,
Cockwell
P.
The
biology
of
immunoglobulin
free
light
chains
and
kidney
injury.
Kidney
international.
2011;79(12):1289-301.
21.
Ying
W-Z,
Wang
P-X,
Aaron
KJ,
Basnayake
K,
Sanders
PW.
Immunoglobulin
light
chains
activate
nuclear
factor-B
in
renal
epithelial
cells
through
a
Src-dependent
mechanism.
Blood.
2011;117(4):1301-7.
22.
Hutchison
CA,
Cockwell
P,
Stringer
S,
Bradwell
A,
Cook
M,
Gertz
MA,
et
al.
Early
reduction
of
serum-free
light
chains
associates
with
renal
recovery
in
myeloma
kidney.
Journal
of
the
American
Society
of
Nephrology.
2011;22(6):1129-36.
23.
Leung
N,
Nasr
SH.
Myeloma-related
kidney
disease.
Advances
in
chronic
kidney
disease.
2014;21(1):36-47.
24.
Dimopoulos
M,
Kastritis
E,
Christoulas
D,
Migkou
M,
Gavriatopoulou
M,
Gkotzamanidou
M,
et
al.
Treatment
of
patients
with
relapsed/refractory
multiple
myeloma
with
lenalidomide
and
dexamethasone
with
or
without
bortezomib:
prospective
evaluation
of
the
impact
of
cytogenetic
abnormalities
and
of
previous
therapies.
Leukemia.
2010;24(10):1769.
25.
Piazzi
G,
Acosta
J,
Smith
B,
Faye
N,
Lekh
B.
Multiple
Myeloma
Overview.
26.
Dimopoulos
MA,
Terpos
E,
Chanan-Khan
A,
Leung
N,
Ludwig
H,
Jagannath
S,
et
al.
Renal
impairment
in
patients
with
multiple
myeloma:
a
consensus
statement
on
behalf
of
the
International
Myeloma
Working
Group.
Journal
of
Clinical
Oncology.
2010;28(33):4976-84.
27.
Shaughnessy
JD,
Zhan
F,
Burington
BE,
Huang
Y,
Colla
S,
Hanamura
I,
et
al.
A
validated
gene
expression
model
of
high-risk
multiple
myeloma
is
defined
by
deregulated
expression
of
genes
mapping
to
chromosome
1.
Blood.
2007;109(6):2276-84.
28.
Cavo
M,
Rajkumar
SV,
Palumbo
A,
Moreau
P,
Orlowski
R,
Bladé
J,
et
al.
International
Myeloma
Working
Group
consensus
approach
to
the
treatment
of
multiple
myeloma
patients
who
are
candidates
for
autologous
stem
cell
transplantation.
Blood.
2011;117(23):6063-73.
29.
Ludwig
H,
Bolejack
V,
Crowley
J,
Bladé
J,
Miguel
JS,
Kyle
RA,
et
al.
Survival
and
years
of
life
lost
in
different
age
cohorts
of
patients
with
multiple
myeloma.
Journal
of
clinical
oncology.
2010;28(9):1599-605.
30.
Dimopoulos
M,
Roussou
M,
Gkotzamanidou
M,
Nikitas
N,
Psimenou
E,
Mparmparoussi
D,
et
al.
The
role
of
novel
agents
on
the
reversibility
of
renal
impairment
in
newly
diagnosed
symptomatic
patients
with
multiple
myeloma.
Leukemia.
2013;27(2):423.
31.
Dimopoulos
MA,
Sonneveld
P,
Leung
N,
Merlini
G,
Ludwig
H,
Kastritis
E,
et
al.
International
myeloma
working
group
recommendations
for
the
diagnosis
and
management
of
myeloma-related
renal
impairment.
Journal
of
Clinical
Oncology.
2016;34(13):1544-57.
32.
Richardson
PG,
Barlogie
B,
Berenson
J,
Singhal
S,
Jagannath
S,
Irwin
D,
et
al.
A
phase
2
study
of
bortezomib
in
relapsed,
refractory
myeloma.
New
England
Journal
of
Medicine.
2003;348(26):2609-17.
33.
Kuhn
DJ,
Chen
Q,
Voorhees
PM,
Strader
JS,
Shenk
KD,
Sun
CM,
et
al.
Potent
activity
of
carfilzomib,
a
novel,
irreversible
inhibitor
of
the
ubiquitin-proteasome
pathway,
against
preclinical
models
of
multiple
myeloma.
Blood.
2007;110(9):3281-90.
34.
Shah
JJ,
Stadtmauer
EA,
Abonour
R,
Cohen
AD,
Bensinger
WI,
Gasparetto
C,
et
al.
A
multi-center
phase
I/II
trial
of
carfilzomib
and
pomalidomide
with
dexamethasone
(Car-Pom-d)
in
patients
with
relapsed/refractory
multiple
myeloma.
Am
Soc
Hematology;
2012.
35.
Stewart
AK,
Rajkumar
SV,
Dimopoulos
MA,
Masszi
T,
Špika
I,
Oriol
A,
et
al.
Carfilzomib,
lenalidomide,
and
dexamethasone
for
relapsed
multiple
myeloma.
New
England
Journal
of
Medicine.
2015;372(2):142-52.
36.
Assouline
S,
Chang
J,
Cheson
B,
Rifkin
R,
Hamburg
S,
Reyes
R,
et
al.
Phase
1
dose-escalation
study
of
IV
ixazomib,
an
investigational
proteasome
inhibitor,
in
patients
with
relapsed/refractory
lymphoma.
Blood
cancer
journal.
2014;4(10):e251.
37.
Gupta
N,
Hanley
MJ,
Harvey
RD,
Badros
AZ,
Lipe
BC,
Kukreti
V,
et
al.
Phase
1/1b
pharmacokinetic
(PK)
and
safety
study
of
the
investigational
oral
proteasome
inhibitor
(PI)
ixazomib
in
relapsed/refractory
multiple
myeloma
(RRMM)
patients
(Pts)
with
severe
renal
impairment
or
end-stage
renal
disease
(ESRD)
requiring
hemodialysis.
Am
Soc
Hematology;
2015.
38.
Moreau
P,
Masszi
T,
Grzasko
N,
Bahlis
NJ,
Hansson
M,
Pour
L,
et
al.
Ixazomib,
an
investigational
oral
proteasome
inhibitor
(PI),
in
combination
with
lenalidomide
and
dexamethasone
(IRd),
significantly
extends
progression-free
survival
(PFS)
for
patients
(Pts)
with
relapsed
and/or
refractory
multiple
myeloma
(RRMM):
the
phase
3
Tourmaline-MM1
study
(NCT01564537).
Am
Soc
Hematology;
2015.
39.
Kocoglu
M,
Badros
A.
The
role
of
immunotherapy
in
multiple
myeloma.
Pharmaceuticals.
2016;9(1):3.
40.
Noonan
KA,
Huff
CA,
Davis
J,
Lemas
MV,
Fiorino
S,
Bitzan
J,
et
al.
Adoptive
transfer
of
activated
marrow-infiltrating
lymphocytes
induces
measurable
antitumor
immunity
in
the
bone
marrow
in
multiple
myeloma.
Science
translational
medicine.
2015;7(288):288ra78-ra78.
41.
Rapoport
A,
al.
e.
NY-ESO-1
–
specifc
TCR
-engineered
T
CELL
mediate
sustained
antigen-specifc
antitumor
effects
in
myeloma.
Nature
Medicine.
2015;21.
42.
Mohamed
AJ,
Yu
L,
Bäckesjö
CM,
Vargas
L,
Faryal
R,
Aints
A,
et
al.
Bruton’s
tyrosine
kinase
(Btk):
function,
regulation,
and
transformation
with
special
emphasis
on
the
PH
domain.
Immunological
reviews.
2009;228(1):58-73.
43.
Bradshaw
JM.
The
Src,
Syk,
and
Tec
family
kinases:
distinct
types
of
molecular
switches.
Cellular
signalling.
2010;22(8):1175-84.
44.
Vihinen
M,
Mattsson
PT,
Smith
C.
Bruton
tyrosine
kinase
(BTK)
in
X-linked
agammaglobulinemia
(XLA).
Front
Biosci.
2000;5:D917-D28.
45.
Buggy
JJ,
Elias
L.
Bruton
tyrosine
kinase
(BTK)
and
its
role
in
B-cell
malignancy.
International
reviews
of
immunology.
2012;31(2):119-32.
46.
Chari
A,
Chhabra
S,
Usmani
S,
Larson
S,
Niesvizky
R,
Matous
J,
et
al.
Combination
Treatment
of
the
Bruton’s
Tyrosine
Kinase
Inhibitor
Ibrutinib
and
Carfilzomib
in
Patients
with
Relapsed
or
Relapsed
and
Refractory
Multiple
Myeloma:
Initial
Results
from
a
Multicenter
Phase
1/2b
Study.
Am
Soc
Hematology;
2015.
47.
Tosi
P,
Zamagni
E,
Tacchetti
P,
Ceccolini
M,
Perrone
G,
Brioli
A,
et
al.
Thalidomide-dexamethasone
as
induction
therapy
before
autologous
stem
cell
transplantation
in
patients
with
newly
diagnosed
multiple
myeloma
and
renal
insufficiency.
Biology
of
Blood
and
Marrow
Transplantation.
2010;16(8):1115-21.
48.
Tosi
P,
Zamagni
E,
Cellini
C,
Cangini
D,
Tacchetti
P,
Tura
S,
et
al.
Thalidomide
alone
or
in
combination
with
dexamethasone
in
patients
with
advanced,
relapsed
or
refractory
multiple
myeloma
and
renal
failure.
European
journal
of
haematology.
2004;73(2):98-103.
49.
Rajkumar
SV,
Jacobus
S,
Callander
NS,
Fonseca
R,
Vesole
DH,
Williams
ME,
et
al.
Lenalidomide
plus
high-dose
dexamethasone
versus
lenalidomide
plus
low-dose
dexamethasone
as
initial
therapy
for
newly
diagnosed
multiple
myeloma:
an
open-label
randomised
controlled
trial.
The
lancet
oncology.
2010;11(1):29-37.
50.
Sonneveld
P,
Heyne
N,
Kueenburg
E,
Glasmacher
AG,
Kasserra
C,
Rosettani
B,
et
al.
MM-013:
An
ongoing
phase
2
trial
of
pomalidomide
and
low-dose
dexamethasone
(POM+
LoDEX)
in
relapsed/refractory
multiple
myeloma
(RRMM)
with
moderate
or
severe
renal
impairment
(RI)
including
patients
(pts)
undergoing
hemodialysis.
American
Society
of
Clinical
Oncology;
2014.
51.
Lacy
MQ,
Hayman
SR,
Gertz
MA,
Short
KD,
Dispenzieri
A,
Kumar
S,
et
al.
Pomalidomide
(CC4047)
plus
low
dose
dexamethasone
(Pom/dex)
is
active
and
well
tolerated
in
lenalidomide
refractory
multiple
myeloma
(MM).
Leukemia.
2010;24(11):1934-9.
52.
Dimopoulos
M,
Sonneveld
P,
Siegel
D,
Palumbo
A,
San-Miguel
J.
Carfilzomib
and
pomalidomide
in
patients
with
relapsed
and/or
refractory
multiple
myeloma
with
baseline
risk
factors.
Annals
of
Oncology.
2015:mdv325.
53.
Chanan-Khan
A,
Swaika
A,
Paulus
A,
Kumar
S,
Mikhael
J,
Rajkumar
S,
et
al.
Pomalidomide:
the
new
immunomodulatory
agent
for
the
treatment
of
multiple
myeloma.
Blood
cancer
journal.
2013;3(9):e143.
54.
Wolf
JL,
Siegel
D,
Goldschmidt
H,
Hazell
K,
Bourquelot
PM,
Bengoudifa
BR,
et
al.
Phase
II
trial
of
the
pan-deacetylase
inhibitor
panobinostat
as
a
single
agent
in
advanced
relapsed/refractory
multiple
myeloma.
Leukemia
&
lymphoma.
2012;53(9):1820-3.
55.
San-Miguel
JF,
Hungria
VT,
Yoon
S-S,
Beksac
M,
Dimopoulos
MA,
Elghandour
A,
et
al.
Panobinostat
plus
bortezomib
and
dexamethasone
versus
placebo
plus
bortezomib
and
dexamethasone
in
patients
with
relapsed
or
relapsed
and
refractory
multiple
myeloma:
a
multicentre,
randomised,
double-blind
phase
3
trial.
The
lancet
oncology.
2014;15(11):1195-206.
56.
Collins
SM,
Bakan
CE,
Swartzel
GD,
Hofmeister
CC,
Efebera
YA,
Kwon
H,
et
al.
Elotuzumab
directly
enhances
NK
cell
cytotoxicity
against
myeloma
via
CS1
ligation:
evidence
for
augmented
NK
cell
function
complementing
ADCC.
Cancer
Immunology,
Immunotherapy.
2013;62(12):1841-9.
57.
Lonial
S,
Vij
R,
Harousseau
J-L,
Facon
T,
Moreau
P,
Mazumder
A,
et
al.
Elotuzumab
in
combination
with
lenalidomide
and
low-dose
dexamethasone
in
relapsed
or
refractory
multiple
myeloma.
Journal
of
Clinical
Oncology.
2012;30(16):1953-9.
58.
van
Rhee
F,
Szmania
SM,
Dillon
M,
van
Abbema
AM,
Li
X,
Stone
MK,
et
al.
Combinatorial
efficacy
of
anti-CS1
monoclonal
antibody
elotuzumab
(HuLuc63)
and
bortezomib
against
multiple
myeloma.
Molecular
cancer
therapeutics.
2009;8(9):2616-24.
59.
Plesner
T,
Arkenau
H-T,
Gimsing
P,
Krejcik
J,
Lemech
C,
Minnema
MC,
et
al.
Phase
1/2
study
of
daratumumab,
lenalidomide,
and
dexamethasone
for
relapsed
multiple
myeloma.
Blood.
2016;128(14):1821-8.
60.
Lokhorst
HM,
Plesner
T,
Laubach
JP,
Nahi
H,
Gimsing
P,
Hansson
M,
et
al.
Targeting
CD38
with
daratumumab
monotherapy
in
multiple
myeloma.
N
Engl
J
Med.
2015;2015(373):1207-19.
61.
Arkenau
T,
Lokhorst
H,
Gimsing
P,
Krejcik
J,
Lemech
C,
Minnema
MC,
et
al.
Preliminary
safety
and
efficacy
data
of
daratumumab
in
combination
with
lenalidomide
and
dexamethasone
in
relapsed
or
refractory
multiple
myeloma.
Am
Soc
Hematology;
2013.
62.
Tai
Y-T,
de
Weers
M,
Li
X-F,
Song
W,
Nahar
S,
Bakker
JM,
et
al.
Daratumumab,
a
Novel
Potent
Human
Anti-CD38
Monoclonal
Antibody,
Induces
Significant
Killing
of
Human
Multiple
Myeloma
Cells:
Therapeutic
Implication.
Am
Soc
Hematology;
2009.
63.
Kumar
A,
Loughran
T,
Alsina
M,
Durie
BG,
Djulbegovic
B.
Management
of
multiple
myeloma:
a
systematic
review
and
critical
appraisal
of
published
studies.
The
Lancet
oncology.
2003;4(5):293-304.
64.
Child
JA,
Morgan
GJ,
Davies
FE,
Owen
RG,
Bell
SE,
Hawkins
K,
et
al.
High-dose
chemotherapy
with
hematopoietic
stem-cell
rescue
for
multiple
myeloma.
New
England
Journal
of
Medicine.
2003;348(19):1875-83.
65.
Blade
J,
Vesole
DH,
Gertz
M.
Transplantation
for
multiple
myeloma:
who,
when,
how
often.
Blood.
2003;102(10):3469-77.
66.
Attal
M,
Harousseau
J-L,
Stoppa
A-M,
Sotto
J-J,
Fuzibet
J-G,
Rossi
J-F,
et
al.
A
prospective,
randomized
trial
of
autologous
bone
marrow
transplantation
and
chemotherapy
in
multiple
myeloma.
New
England
Journal
of
Medicine.
1996;335(2):91-7.
67.
Moreau
P,
Hulin
C,
Macro
M,
Caillot
D,
Chaleteix
C,
Roussel
M,
et
al.
Bortezomib,
thalidomide
and
dexamethasone
(VTD)
is
superior
to
bortezomib,
cyclophosphamide
and
dexamethasone
(VCD)
prior
to
autologous
stem
cell
transplantation
for
patients
with
de
novo
multiple
myeloma.
Results
of
the
prospective
IFM
2013-04
trial.
Am
Soc
Hematology;
2015.
68.
McCarthy
PL,
Owzar
K,
Hofmeister
CC,
Hurd
DD,
Hassoun
H,
Richardson
PG,
et
al.
Lenalidomide
after
stem-cell
transplantation
for
multiple
myeloma.
New
England
Journal
of
Medicine.
2012;366(19):1770-81.
69.
Attal
M,
Lauwers-Cances
V,
Marit
G,
Caillot
D,
Moreau
P,
Facon
T,
et
al.
Lenalidomide
maintenance
after
stem-cell
transplantation
for
multiple
myeloma.
New
England
Journal
of
Medicine.
2012;366(19):1782-91.
70.
Attal
M,
Lauwers-Cances
V,
Hulin
C,
Facon
T,
Caillot
D,
Escoffre
M,
et
al.
Autologous
transplantation
for
multiple
myeloma
in
the
era
of
new
drugs:
a
phase
III
study
of
the
Intergroupe
Francophone
du
Myelome
(IFM/DFCI
2009
trial).
Am
Soc
Hematology;
2015.
71.
Benboubker
L,
Dimopoulos
MA,
Dispenzieri
A,
Catalano
J,
Belch
AR,
Cavo
M,
et
al.
Lenalidomide
and
dexamethasone
in
transplant-ineligible
patients
with
myeloma.
New
England
Journal
of
Medicine.
2014;371(10):906-17.
72.
Gavriatopoulou
M,
Terpos
E,
Kastritis
E,
Dimopoulos
MA.
Current
treatments
for
renal
failure
due
to
multiple
myeloma.
Expert
opinion
on
pharmacotherapy.
2016;17(16):2165-77.
73.
Burnette
BL,
Leung
N,
Rajkumar
SV.
Renal
improvement
in
myeloma
with
bortezomib
plus
plasma
exchange.
New
England
Journal
of
Medicine.
2011;364(24):2365-6.
74.
Hutchison
CA,
Bradwell
AR,
Cook
M,
Basnayake
K,
Basu
S,
Harding
S,
et
al.
Treatment
of
acute
renal
failure
secondary
to
multiple
myeloma
with
chemotherapy
and
extended
high
cut-off
hemodialysis.
Clinical
Journal
of
the
American
Society
of
Nephrology.
2009;4(4):745-54.
75.
Nayak
L,
Lazarus
H.
Renal
allografts
in
plasma
cell
myeloma
hematopoietic
cell
graft
recipients:
on
the
verge
of
an
explosion?
Bone
marrow
transplantation.
2013;48(3):338.
76.
Mitsiades
CS,
Mitsiades
NS,
McMullan
CJ,
Poulaki
V,
Shringarpure
R,
Hideshima
T,
et
al.
Transcriptional
signature
of
histone
deacetylase
inhibition
in
multiple
myeloma:
biological
and
clinical
implications.
Proceedings
of
the
National
Academy
of
Sciences
of
the
United
States
of
America.
2004;101(2):540-5.
77.
Hideshima
T,
Richardson
PG,
Anderson
KC.
Mechanism
of
action
of
proteasome
inhibitors
and
deacetylase
inhibitors
and
the
biological
basis
of
synergy
in
multiple
myeloma.
Molecular
cancer
therapeutics.
2011;10(11):2034-42.
78.
San-Miguel
JF,
Richardson
PG,
Günther
A,
Sezer
O,
Siegel
D,
Bladé
J,
et
al.
Phase
Ib
study
of
panobinostat
and
bortezomib
in
relapsed
or
relapsed
and
refractory
multiple
myeloma.
Journal
of
Clinical
Oncology.
2013;31(29):3696-703.
79.
Richardson
PG,
Weller
E,
Lonial
S,
Jakubowiak
AJ,
Jagannath
S,
Raje
NS,
et
al.
Lenalidomide,
bortezomib,
and
dexamethasone
combination
therapy
in
patients
with
newly
diagnosed
multiple
myeloma.
Blood.
2010;116(5):679-86.
80.
Badros
A,
Burger
AM,
Philip
S,
Niesvizky
R,
Kolla
SS,
Goloubeva
O,
et
al.
Phase
I
study
of
vorinostat
in
combination
with
bortezomib
for
relapsed
and
refractory
multiple
myeloma.
Clinical
Cancer
Research.
2009;15(16):5250-7.
81.
Kikuchi
J,
Wada
T,
Shimizu
R,
Izumi
T,
Akutsu
M,
Mitsunaga
K,
et
al.
Histone
deacetylases
are
critical
targets
of
bortezomib-induced
cytotoxicity
in
multiple
myeloma.
Blood.
2010;116(3):406-17.
|
|
.................................................................................................................

|
| |
|

