|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
|
|
|
........................................................
In Memoriam
Professor
Orhan Ekrem Müftüoglu
|
........................................................
Original
Contribution / Clinical Investigation
|







|
Cholelithiasis
and cholecystectomy may lower the low density
lipoprotein cholesterol in plasma
DOI: 10.5742/MEWFM.2017.93010
[pdf
version]
Mehmet Rami Helvaci, Mursel Davarci, Orhan Veli
Ozkan, Ersan Semerci, Abdulrazak Abyad, Lesley
Pocock
Serum
and follicular fluid vitamin D and follicular
response among infertile women undergoing ICSI
DOI: 10.5742/MEWFM.2017.93011
[pdf
version]
Sedighe Esmaeilzadeh, Maryam Aliasgharpour,
Parvaneh Mirabi, Azita Ghanbarpour
Maede Fasihian
Studying
the relation of quality of work life with socio-economic
status and general health among the employees
working in Students Welfare Fund of Ministry
of Health and Medical Education in 2016
DOI: 10.5742/MEWFM.2017.93012
[pdf
version]
Saeed Reza Azami, Nasrin Shaarbafchizadeh, Soheil
Mokhtari, Ali Maher
On the Effect
of Cognitive Behavioural Counseling on Sexual
Satisfaction of Mothers with Autistic Children:
A Randomized Clinical Trial
DOI:
[pdf version]
Leila Arbil, Mitra Kolivand, Farzaneh Golboni,
Effat MerghatiKhoei, Mansour Rezaei
Pre-operative
sublingual misoprostol and intra-operative blood
loss during total abdominal hysterectomy: a
randomized single-blinded controlled clinical
trial
DOI: 10.5742/MEWFM.2017.93013
[pdf
version]
Taravat Fakheri, Tayebe Noori
Investigating
the Effect of Endotracheal Tube Cuff Pressure
on Sore Throat, Hoarseness and Cough in Patients
with Coronary Artery Bypass Surgery
DOI: 10.5742/MEWFM.2017.93014
[pdf
version]
Ali Akbar Vaezi, Mohammad Hassan Mondegari Bamakan
Comparing
the Self-Esteem and Resiliency between Blind
and Sighted Children and Adolescents in Kermanshah
City
DOI: 10.5742/MEWFM.2017.93015
[pdf
version]
Saeedeh Bakhshi, Nafiseh Montazeri , Babak Nazari,
Arash Ziapour, Hashem Barahooyi,
Fatemeh Dehghan
|
........................................................
Population
and Community Studies
|







|
Frequency
of Uric Acid Levels, Symptomatic and Asymptomatic
Hyperuricemia among the Pakistani Population
DOI: 10.5742/MEWFM.2017.93016
[pdf
version]
Waris Qidwai, Masood Jawaid
Determinants
of Tooth Brushing among Primary School Students
DOI: 10.5742/MEWFM.2017.93017
[pdf
version]
Mohammad Mahboubi, Mohammad Ismail Motlagh,
Mehdi Mirzaei-Alavijeh, Farzad Jalilian, Hassan
Gharibnavaz,
Mohammad Fattahi
Depression
in patients suffering from gender dysphoria:
The hospitalized patients of Legal Medicine
Center in Southwest of Iran
DOI: 10.5742/MEWFM.2017.93018
[pdf
version]
Zahra Gorjian, Mohammad Zarenezhad, Mohhamad
Mahboubi, Saeid Gholamzadeh,
Nahid Mahmoodi
An epidemiological
study of suicide attempts and to determine the
correlation between attempted suicide causes
and demographic characteristics of people in
Kermanshah Province during a year
DOI: 10.5742/MEWFM.2017.93019
[pdf
version]
Hamid Reza Shetabi, Samira Rostami, Mohsen Mohammadi,
Mahsa Cheleii, Lida Saedi, Saba Amiri Nasab,
Shirin Zardui GolAnbari
The
effectiveness of life skills training on happiness,
mental health, and marital satisfaction in wives
of Iran-Iraq war veterans
DOI: 10.5742/MEWFM.2017.93038
[pdf
version]
Kamal Solati
The
Role of Self-Compassion Factors in Predicting
the Marital Satisfaction of Staff at Kermanshah
University of Medical Sciences
DOI:10.5742/MEWFM.2017.93020
[pdf
version]
Parisa Janjani, Lida Haghnazari, Farahnaz Keshavarzi,
Alireza Rai
Mediating
role of irrational beliefs in the relationship
between the quality of family communication
and marital satisfaction
DOI:10.5742/MEWFM.2017.93021
[pdf
version]
Parisa Janjani, Khodamorad Momeni, Alireza Rai,
Mohammad Reza Saidi
|
........................................................
Review Article
........................................................
International Health
Affairs
........................................................
Education
and Training
........................................................
Clinical
Research and Methods
|





|
Adaptive
LASSO Logistic Regression applied on gene expression
of prostate cancer
DOI: 10.5742/MEWFM.2017.93028
[pdf version]
Amir Hossein Hashemian, Maryam Ghobadi Asl,
Soodeh Shahsavari, Mansour Rezaei,
Hadi Raeisi Shahraki
The
prevalence of brain and neck injuries in patients
with maxillofacial fractures in teaching hospitals
of Rasht in 2016
DOI: 10.5742/MEWFM.2017.93029
[pdf
version]
Seyed Mohammad Talebzadeh, Ali Khalighi Sigaroudi,
Babak Alijani, Safa Motevasseli,
Saied Dashtyari, Mahsa Shariati, Zeinab Davoudmanesh
Cultural
competency: a concept analysis in TUMS (Tehran
University of Medical Science) DOI:
10.5742/MEWFM.2017.93030
[pdf version]
Foruzan Khatamidoost, Mandana Shirazy, Hamid
Khankeh, Nemat Allah Musapour
Majid Sadeghi, Kamran Soltani Arabshahi
The
Effect of Proprioceptive Neuromuscular Facilitation
(PNF) on Activities of Daily Living of client
with Cerebrovascular accident
DOI: 10.5742/MEWFM.2017.93031
[pdf
version]
Najafi Doulatabad Shahla, Afrasiabifar Ardashir,
Parandvar Yaghoub
Evaluation
of the ratio of T helper 17 and T regulatory
cells in patients with chronic idiopathic urticaria
DOI: 10.5742/MEWFM.2017.93032
[pdf
version]
Hossein Shahriari, Farahzad Jabbari, Seyyed
Abdolrahim Rezaee, Houshang Rafatpanah
Majid Jafari, Reza Farid Hosseini, Majid Asadi-Samani
|
........................................................
Model
and System of Primary Care
........................................................
Case
Series and Case Reports
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| September 2017
- Volume 15, Issue 7 |
|
|
Frequency of Uric Acid
Levels, Symptomatic and Asymptomatic Hyperuricemia
among the Pakistani Population
Waris Qidwai (1)
Masood Jawaid (2)
(1) MBBS, MCPS (FM), FCPS (FM), FRCGP (INT),
FCGP(SL), MFPH(UK)
The Tajuddin Chatoor, Professor and Chairman,
Department of Family Medicine
Service Line Chief, Family Health, Aga Khan
University, Karachi
(2) MBBS, MCPS, MRCS, FCPS, MHPE
Consultant Surgeon, Darul Sehat Hospital, Karachi
Correspondence:
Dr. Waris Qidwai, MBBS, MCPS (FM), FCPS (FM),
FRCGP (INT), FCGP(SL), MFPH(UK)
Professor and Chairman, Department of Family
Medicine
Service Line Chief, Family Health, Aga Khan
University, Karachi
Stadium Road, PO Box: 3500. Karachi-74800, Pakistan
Tel: 92-21-3486-4842 (Office) 92-3332317836
(Cell)
Mobile: 0301-8216783m Fax: 92-21-3493-429
Email: waris.qidwai@aku.edu
|
Abstract
Background:
Hyperuricemia is an independent risk factor
for cardiovascular disease, cerebrovascular
diseases, chronic kidney diseases, diabetes
mellitus, hypertension, obesity and dyslipidemia.
Its global burden suggests the widest
prevalence range in East Asia. No large
scale study exists to estimate the prevalence
of hyperuricemia across Pakistan. Hence,
this study aims to estimate the frequency
of hyperuricemia in Pakistan.
Patients and
Methods: It was a population-based
cross sectional survey conducted in health
care facilities across Pakistan. A total
of 2,727 complete responses were obtained
after taking informed consent. The questionnaire
included sociodemographic details and
serum uric acid levels of the patients.
This study regards hyperuricemia as serum
uric acid levels greater than 7 mg/dl
in males and greater than 6 mg/dl in females.
MultiSure blood glucose/uric acid Monitoring
System was used to measure serum uric
acid. Data was analysed using SPSS version
23.
Results: With
mean age of 43.60 years, 1,320 (48.4%)
participants were males while 1,407 (51.6%)
were females. Mean uric acid level in
male hyperuricemics was 8.11±1.25
mg/dl and in females was 7.44±1.19
mg/dl. The frequency of hyperuricemia
was 39% (n=1,061). Frequency of hyperuricemia
among males was 27.9% (n=367) and 49.3%
(n=694) among females. Of the hyperuricemic
population, 90.8% (n=963) were symptomatic.
Most common comorbidity was diabetes 35.5%
(n=388). Least common comorbidity was
Ischemic heart disease 2.1% (n=23). Patients
with no comorbidities were more likely
to be asymptomatic.
Conclusion:
The burden of hyperuricemia together with
increasing burden of metabolic syndrome,
obesity, ischemic heart disease and chronic
kidney disease is becoming alarming. The
rising statistics emphasize the dire need
to develop proficient prevention and management
strategies for hyperuricemia.
Key words:
Uric acid, Prevalence, Gout, Hyperuricemia,
Pakistan
|
Hyperuricemia (HU), or raised serum uric acid
(SUA), is the condition closely associated with
gout which is a form of inflammatory arthritis
triggered by the crystallization of uric acid
within the joints. Gout leads to substantial
morbidity and affects 1-2% of the world population.
[1]
Hyperuricemia itself evolves from nonfunctioning
uricase gene and contributes to increased risk
for cardiovascular diseases (CVDs); moreso in
women. [2] [3]
Although previous studies didn’t identify
hyperuricemia as an independent risk factor
for CVDs because of the presence of obesity,
dyslipidemia, hypertension, use of diuretics
and insulin resistance in parallel, [4] recent
literature has provided evidence for hyperuricemia
to be an independent risk factor for cardiovascular
diseases, cerebrovascular diseases, chronic
kidney diseases, type II diabetes mellitus,
hypertension, obesity and dyslipidemia. [5]
High SUA levels are associated with elevated
total serum antioxidant capacity among individuals
with atherosclerosis. High SUA levels may cause
atherosclerosis through disturbing lipid metabolism,
promoting the proliferation of vascular smooth
muscle cells, and by activating inflammation.
[6] Where insulin resistance plays a potentially
key role in the relationship between metabolic
syndrome, type 2 Diabetes and hyperuricemia,
it is likely that HU and insulin resistance
share a bidirectional causal effect. [7] The
early appearance of hyperuricemia is a reliable
predictor of later development of hypertension,
and in adults with essential hypertension the
comorbidity of hyperuricemia is very common.
[8]
Even with such a crucial influence of uric
acid levels on various body systems, it has
remained a lesser studied domain. Although,
local data exists to support association of
hyperuricemia with severe coronary artery disease
[9] and metabolic syndrome; [10] no large scale
study exists to estimate the prevalence of hyperuricemia
across Pakistan. Hence, this multicentre study
was conducted with the aims to estimate the
prevalence of hyperuricemia in Pakistan.
It was a population-based cross sectional survey,
conducted from January 1st to December 31st
2016, in different primary care clinics and
tertiary care hospitals across Pakistan. A total
of 3,000 individuals, of age 18 years and above,
were invited to participate in the study. However,
after eliminating 145 non-responders and 128
incompletely responded questionnaires, 2,727
genuine and complete responses were obtained
in our study. Written informed consent was obtained
from the patients. The questionnaire included
sociodemographic details (such as age, gender,
comorbidity), symptoms of hyperuricemia and
uric acid levels of the patients. This study
regards hyperuricemia as serum uric acid levels
greater than 7 mg/dl in males and greater than
6 mg/dl in females. [11] Comorbidities were
taken as per the diagnosis of the treating physician.
Where we present our population as symptomatic
for HU, we included chronic single/multiple
joint pain, urinary stones and tumor lysis syndrome
as symptoms of hyperuricemia in this study.
In order to assess uric acid levels, MultiSure
blood glucose/uric acid Monitoring System was
used in this study. MultiSure is a portable,
hand-held device with advanced biosensor technology
to accurately assess blood uric acid levels.
With a sample volume of 3 µL, MultiSure
has a measuring range of 3 - 20 mg/dL (1.1 ~
33.3 mmol/L) and a measuring time of 30 seconds.
[12]
Data was entered and descriptive analysis was
performed with SPSS software version 23. Frequency
of patients with HU was calculated. Mean age
and SUA levels were calculated. Stratification
with respect to gender and symptomatic or asymptomatic
was done and relation with morbidity and symptoms
of hyperuricemia was calculated via cross tabulation
and was presented in tabular form.
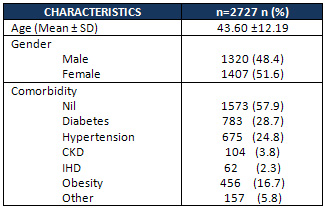
A
total
of
2,727
patients
participated.
With
a
mean
±
SD
age
of
43.60
±
12.19
years,
1,320
(48.4%)
were
males
while
1,407
(51.6%)
were
females.
Comorbidities
were
present
in
1,154
(42.3%)
patients
which
are
shown
in
detail
in
Table
1.
Table
1:
Characteristics
of
the
subjects
included
in
the
study
Mean
uric
acid
(MUA)
levels
of
the
entire
sample
were
6.11
±
1.7
mg/dl.
MUA
level
of
males
was
6.19
±
1.65
mg/dl
and
that
of
females
was
6.04
±
1.75
mg/dl.
The
prevalence
of
hyperuricemia
in
our
study
was
39%
(n=1,061).
Frequency
of
hyperuricemia
among
males
was
27.9%
(n=367)
and
49.3%
(n=694)
among
females.
Of
patients
with
HU,
9.2%
(n=98)
were
asymptomatic
at
the
time
of
study
while
90.8%
(n=963)
presented
with
symptoms
of
hyperuricemia.
MUA
level
of
clinically
symptomatic
population
was
7.67±1.24
mg/dl
and
of
asymptomatic
was
7.68±1.37
mg/dl.
The
proportion
of
patients
with
HU
presenting
with
various
comorbidities
and
their
MUA
levels
are
shown
in
Table
2.
Click
here
for
Table
2:
Uric
Acid
Level
in
different
populations
(mg/dl)
As
seen
in
Table
3,
comorbidities
were
more
common
in
patients
with
hyperuricemia;
only
32.9%
were
without
any
comorbidity.
The
most
common
comorbidity
was
diabetes;
36.6%
(n=388).
Although
IHD
was
the
least
commonly
witnessed
comorbidity
in
our
HU
patients
2.2%
(n=23);
it
was
seen
that
100%
of
IHD
patients
were
symptomatic
(Table
3).
Click
here
for
Table
3:
Asymptomatic
and
symptomatic
Hyperuricemia
among
different
comorbid
populations
We
reported
a
hyperuricemia
prevalence
of
39%
in
the
Pakistani
population
with
a
mean
uric
acid
(MUA)
level
of
6.11
±
1.7
mg/dl
among
all
subjects
while
7.67±1.26
mg/dl
MUA
level
among
hyperuricemic
subjects.
HU
was
found
to
be
more
prevalent
in
women
than
in
men
(49.3%
vs.
27.9%).
The
proportion
of
clinically
asymptomatic
HU
was
9.2%.
Most
of
our
HU
sample
had
one
or
more
comorbidities
and
was
symptomatic.
Most
common
comorbidity
in
our
patients
with
HU
was
Diabetes
Mellitus.
Although
Ischemic
Heart
Disease
was
the
least
common
comorbidity,
all
patients
of
IHD
were
symptomatic.
Except
for
chronic
kidney
disease
and
IHD,
all
other
comorbidities
were
significantly
related
to
SUA
levels
in
our
study.
This
is
the
first
report
of
hyperuricemia
prevalence
from
Pakistan
and
helps
determine
the
burden
of
this
condition
in
the
population.
These
latest
prevalence
estimates
help
determine
the
burden
of
the
condition
on
the
Pakistani
healthcare
system.
As
per
our
knowledge,
no
other
study
has
been
conducted
on
such
a
large
sample
including
population
from
various
cities
of
Pakistan.
However,
we
have
not
utilized
laboratory
methods
to
measure
uric
acids
levels
which
would
have
been
more
accurate
but
also
expensive,
and
only
utilized
portable
MultiSure
kit
(a
validated
test).[12]
Attempts
have
been
made
to
assess
the
global
burden
of
hyperuricemia
and
findings
suggested
widest
range
of
prevalence
in
East
Asia
with
Chinese
prevalence
of
6-25%,
Taiwanese
10-52%
and
Indonesian
prevalence
of
18%.
[1]
Even
in
an
Indian
obese
population,
HU
prevalence
is
44.6%,
however
they
report
more
hyperuricemic
males.
[13]
Furthermore,
as
per
The
National
Health
and
Nutrition
Examination
Survey
2007–2008,
the
prevalence
of
HU
in
the
United
States
general
population
is
21.4%.
[14]
In
a
local
study
involving
a
relatively
smaller
sample,
the
frequency
of
elevated
SUA
levels
was
47%.
[15]
Consistent
with
our
findings,
prevalence
of
metabolic
syndrome
and
its
components
increased
significantly
according
to
SUA
concentration
in
both
sexes
in
a
Korean
study.
[16]
Hyperuricemia
has
been
studied
to
be
somehow
responsible
for
the
proinflammatory
endocrine
imbalance
in
the
adipose
tissue,
which
is
an
underlying
mechanism
of
inflammation
and
consequent
insulin
resistance.
[17]
UA
levels
have
also
been
regarded
as
a
metabolic
biomarker
in
older
adults
for
early
detection
and
prevention
of
Metabolic
Syndrome.
[18]
A
meta-analysis
of
13
studies
showed
1.3%
incidence
of
ischemic
heart
disease
in
individuals
with
HU
and
an
overall
risk
of
IHD
death
increased
by
12%
for
each
increase
of
1
mg/dl
of
serum
uric
acid
level.
[19]
Another
five
year
long
Japanese
cohort
concluded
asymptomatic
HU
to
possess
a
significant
risk
for
developing
hypertension,
dyslipidemia,
obesity
and
chronic
renal
disease.
[20]
As
far
as
the
studies
on
recent
trend
of
chronic
kidney
diseases
are
concerned,
it
has
been
seen
that
both
elevated
SUA
levels
and
metabolic
syndrome
are
associated
with
increase
in
the
prevalence
of
CKD.
[21,
22]
In
a
longitudinal
cohort,
the
incidence
of
CKD
was
influenced
by
the
presence
of
hyperuricemia,
but
not
by
that
of
metabolic
syndrome.
However,
if
complicated
by
metabolic
syndrome,
HU
had
an
even
detrimental
effect.
[23]
In
view
of
the
crucial
role
of
HU
and
its
incapacitating
impacts
on
essential
bodily
systems
and
functions,
it
becomes
vital
to
first
assess
its
burden,
recognize
the
targeted
population
and
then
make
endeavours
in
bringing
about
relevant
management
strategies
to
detect
hyperuricemia
at
an
early
stage
and
prevent
its
consequent
complications.
This
study
has
taken
the
first
step
in
this
region.
With
such
a
high
prevalence
of
hyperuricemia
in
Pakistan,
this
study
leads
other
researchers
to
investigate
more
of
this
alarming
issue.
The
burden
of
hyperuricemia
together
with
increasing
burden
of
metabolic
syndrome,
obesity,
ischemic
heart
disease
and
chronic
kidney
disease
is
becoming
alarming.
Hyperuricemia
plays
a
pivotal
role
in
initiating
the
vicious
cycle
of
debilitating
involvement
of
almost
all
vital
body
systems.
The
rising
statistics
further
emphasize
the
significance
and
dire
need
for
the
development
of
proficient
prevention
and
management
strategies
for
hyperuricemia.
Acknowledgment:
This
study
is
supported
by
unconditional
research
grant
and
logistic
support
of
Hyperuricemia
Advisory
Council
(www.haconline.org)
and
PharmEvo
(Pvt)
Ltd.
1.
Smith
E,
March
L.
Global
prevalence
of
hyperuricemia:
a
systematic
review
of
population-based
epidemiological
studies.
Arthritis
Rheum.
2015;67:2690-2692.
2.
Kim
SY,
Guevara
JP,
Kim
KM,
Choi
HK,
Heitjan
DF,
Albert
DA.
Hyperuricemia
and
coronary
heart
disease:
a
systematic
review
and
metaanalysis.
Arthritis
Care
Res.
2010;62(2):170-180.
DOI:
10.1002/acr.20065.
3.
Rodrigues
SL,
Baldo
MP,
Capingana
P,
Magalhães
P,
Dantas
EM,
Molina
MD,
et
al.
Gender
distribution
of
serum
uric
acid
and
cardiovascular
risk
factors:
population
based
study.
Arq
Bras
Cardiol.
2012;98(1):13-21.
DOI:
10.1590/S0066-782X2011005000116.
4.
Burnier
M,
Brunner
HR:
Is
hyperuricemia
a
predictor
of
cardiovascular
risk?
Curr
Opin
Nephrol
Hypertens
1999;8:167-172.
5.
Yu
S,
Guo
X,
Yang
H,
Sun
Y.
Combination
of
hyperuricemia
and
metabolic
syndrome
is
an
independent
and
powerful
predictor
for
left
ventricular
hypertrophy
in
rural
Chinese.
Ann
Endocrinol
(Paris).
2015;76(3);264-271.
Elsevier
Masson.
6.
Liu
Z,
Chen
T,
Niu
H,
Ren
W,
Li
X,
Cui
L,
Li
C.
The
establishment
and
characteristics
of
rat
model
of
atherosclerosis
induced
by
hyperuricemia.
Stem
Cells
Int.
2016.
DOI:
10.1155/2016/1365257.
7.
Li
C,
Hsieh
MC,
Chang
SJ.
Metabolic
syndrome,
diabetes,
and
hyperuricemia.
Curr
Opin
Rheumatol.
2013;25(2):210-6.
DOI:
10.1097/BOR.0b013e32835d951e.
8.
Feig
DI,
Johnson
RJ.
Hyperuricemia
in
childhood
primary
hypertension.
Hypertension.
2003;42:247–252.
DOI:
10.1161/01.HYP.0000085858.66548.59.
9.
Qureshi
AE,
Hameed
S,
Noeman
A.
Relationship
of
serum
uric
acid
level
and
angiographic
severity
of
coronary
artery
disease
in
male
patients
with
acute
coronary
syndrome.
Pak
J
Med
Sci.
2013;29(5):1137-1141.
10.
Siddiqui
SA,
Shabbir
I.
Association
of
Hyperuricemia
with
Metabolic
Syndrome.
Pak
J
Med
Res.
2015;54(1):8-12.
11.
Liu
H,
Zhang
XM,
Wang
YL,
Liu
BC.
Prevalence
of
hyperuricemia
among
Chinese
adults:
a
national
cross-sectional
survey
using
multistage,
stratified
sampling.
J
Nephrol.
2014;27(6):653-8.
DOI:
10.1007/s40620-014-0082-z
12.
Tsai
J.
Blood
Glucose/Uric
Acid
Monitoring
System
–
Accuracy
study
testing
report
(for
uric
acid).
RD0301-A17-01
ApexBio
Taiwan.
2003.
13.
Remedios
C,
Shah
M,
Bhasker
AG,
Lakdawala
M.
Hyperuricemia:
a
reality
in
the
Indian
obese.
Obes
Surg.
2012;22(6):945-948.
DOI:10.1007/s11695-012-0655-7.
14.
Zhu
Y,
Pandya
BJ,
Choi
HK.
Prevalence
of
gout
and
hyperuricemia
in
the
US
general
population:
the
National
Health
and
Nutrition
Examination
Survey
2007–2008.
Arthritis
Rheum.
2011;63(10):3136-3141.
DOI:
10.1002/art.30520.
15.
Arain
AA,
Ali
M,
Shaikh
AA,
Ali
MH.
Hyperuricemia:
an
Emerging
Health
Problem
of
the
Society
Invites
Considerations.
Ortho
&
Rheum
Open
Access
J.
2017;6(1).
OROAJ.MS.ID.555679
(2017).
DOI:
10.19080/OROAJ.2017.06.555679
16.
Choi
H,
Kim
HC,
Song
BM,
Park
JH,
Lee
JM,
Yoon
DL,
Yoon
YM,
Rhee
Y,
Youm
Y,
Kim
CO.
Serum
uric
acid
concentration
and
metabolic
syndrome
among
elderly
Koreans:
The
Korean
Urban
Rural
Elderly
(KURE)
study.
Arch
Gerontol
Geriatr.
2016;64:51-58.
DOI:
http://dx.doi.org/10.1016/j.archger.2016.01.005
17.
Baldwin
W,
McRae
S,
Marek
G,
Wymer
D,
Pannu
V,
Baylis
C
et
al.
Hyperuricemia
as
a
mediator
of
the
proinflammatory
endocrine
imbalance
in
the
adipose
tissue
in
a
murine
model
of
the
metabolic
syndrome.
Diabetes.
2011;60(4):1258-1269.
DOI:
https://doi.org/10.2337/db10-0916
18.
Chang
JB,
Chen
YL,
Hung
YJ,
Hsieh
CH,
Lee
CH,
Pei
D
et
al.
The
role
of
uric
acid
for
predicting
future
metabolic
syndrome
and
type
2
diabetes
in
older
people.
J
Nutr
Health
Aging.
2017;21(3):329-335.
DOI:
10.1007/s12603-016-0749-3
19.
Kim
SY,
Guevara
JP,
Kim
KM,
Choi
HK,
Heitjan
DF,
Albert
DA.
Hyperuricemia
and
coronary
heart
disease:
a
systematic
review
and
meta-analysis.
Arthritis
Care
Res.
2010;62(2):170-80.
DOI:
10.1002/acr.20065
20.
Kuwabara
M,
Niwa
K,
Hisatome
I,
Nakagawa
T,
Roncal-Jimenez
CA,
Andres-Hernando
A
et
al.
Asymptomatic
Hyperuricemia
Without
Comorbidities
Predicts
Cardiometabolic
Diseases.
Hypertension.
2017;69(4):1036-1044.
DOI:
10.1161/HYPERTENSIONAHA.116.08998
21.
Dai
H,
Lu
S,
Tang
X,
Lu
M,
Chen
R,
Chen
Z
et
al.
Combined
association
of
serum
uric
acid
and
metabolic
syndrome
with
chronic
kidney
disease
in
hypertensive
patients.
Kidney
Blood
Press
Res.
2016;41(4):413-423.
DOI:
https://doi.org/10.1159/000443443
22.
Mahajbeen
W,
Khan
DA.
Independent
Relationship
of
Hyperuricemia
with
Chronic
Kidney
Disease.
J
Isl
Med
Dent
Col.
2014:3(1):7-10.
23.
Kuriyama
S,
Nishio
S,
Kidoguchi
S,
Honda
K,
Takahashi
Y,
Sugano
N
et
al.
A
Greater
Association
of
Hyperuricemia
than
of
Metabolic
Syndrome
with
the
New
Incidence
of
Chronic
Kidney
Disease.
Open
J
Nephrol.
2016;6(01):17.
DOI:
10.4236/ojneph.2016.61003
|
|
.................................................................................................................

|
| |
|

