|
Pre-operative sublingual
misoprostol and intra-operative blood loss during
total abdominal hysterectomy: a randomized single-blinded
controlled clinical trial
Anisodowleh Nankali
(1)
Taravat Fakheri (1)
Maryam Hematti (1)
Tayebe Noori (2)
(1) Department of Obs & Gyn, School
of Medicine, Kermanshah University of Medical
Sciences, Kermanshah, Iran
(2) Research Committee of Student, Kermanshah
University of Medical Sciences, Kermanshah,
Iran
Correspondence:
Taravat Fakheri,
Department of Obs & Gyn,
Imam Reza Hospital, Kermanshah University of
Medical Sciences,
Kermanshah, Iran
Email: fakheritaravats@yahoo.com
|
Abstract
Objective:
To determine the efficacy of sublingual
misoprostol on intra-operative blood loss
during Total Abdominal Hysterectomy (TAH),
need for blood transfusion, hemoglobin
drop, operation length, and hospital stay.
Methods:
In this single-blinded randomized clinical
trial, 60 patients who were candidates
for TAH due to uterine fibroid or abnormal
uterine bleeding were included. They were
randomly divided to receive either misoprostol
400 mcg (30 cases) or vitamin B6 (30 cases)
once sublingually 1 hour before TAH. All
the procedures were performed by a single
surgeon. The volume of blood loss, hemoglobin
change, the need for blood transfusion,
operation and hospital stay duration were
recorded.
Results: The
two groups were comparable regarding Body
Mass Index (BMI) and age, gravidity, and
parity. Mean (±SD) blood loss volume
was lower in misoprostol group (370.13±
158.84) compared to control group (466±
204.7); P= 0.046. Hemoglobin level 24
hours after TAH had higher mean value
in the misoprostol group (11.72) than
in the control group (10.54 g/dL); P=
0.003. Mean hospital stay duration was
shorter in the misoprostol group (3.25±
1.32 days) vs. control group (3.43±
0.5 days), P= 0.003. No significant difference
was observed regarding need for blood
transfusion during the operation between
misoprostol (1/30 patients) vs. control
group (4/30 patients). No fever was identified
in either group after operation.
Conclusion:
Sublingual misoprostol (400 mcg) administered
1 hour before TAH was effective in reducing
blood loss volume, hemoglobin drop, and
hospitalization duration.
Key words:
Total abdominal hysterectomy; hemorrhage;
misoprostol
|
Uterine myomas are the most prevalent gynecologic
benign tumors in women of reproductive age (1).
Large symptomatic myomas which do not respond
to medical therapies in women who have completed
childbearing are considered for total abdominal
hysterectomy. In fact, uterine fibroids are
the most common indication for hysterectomies.
Either in some regions of the world, hysterectomy
is considered as the definitive treatment for
large uterine fibroids (2). Another common condition
for which hysterectomy is the definitive management
is abnormal uterine bleeding (AUB) when medical
managements fail to improve the condition.
TAH can be associated with several complications
including major hemorrhage, thromboembolism,
bladder injury, etc. Severe hemorrhage of more
than 400 mL which may require blood transfusion
is the most common complication of TAH, along
with infectious complications (3). This complication
is estimated to occur in about 2% of the procedures
(4).
Several medical and surgical methods have been
used. Shrinkage of the fibroids using hormonal
manipulation by gonadotropin-releasing hormone
(GnRH) analogues for 3 months before surgery
has been shown to decrease the volume of fibroids
and reduce their vascularity (5). Vasopressin
is another option demonstrated in trials to
be an effective method for this purpose (6).
However, side effects of these therapies along
with high costs may render these therapies unavailable
or not appropriate for most patients.
One of the medical therapies that has gained
attention for pre-hysterectomy use is prostaglandin
E1 synthetic analogue, misoprostol. It has significant
uterotonic properties. The older studies focusing
on this agent have been conducted during labor
and cesarean section (7-11) with promising outcomes.
This practice has extended to hysterectomy and
some limited trials have been done accordingly.
One study assessed rectal misoprostol combined
with oxytocin before laparoscopy-assisted vaginal
hysterectomy (12) and showed that combination
of these two uterotonic agents was efficacious
in decreasing blood loss as well as procedure
time. But another study did not demonstrate
such effect (13). Two studies have investigated
pre-operative sublingual misoprostol for blood
loss during TAH (2, 14). One of these trials
(2) which recruited 132 women undergoing TAH
and administered 400 mcg misoprostol 30 minutes
before TAH, concluded that the group for which
misoprostol was used had lower blood loss (356
mL) compared to placebo group (435 mL). The
authors concluded that misoprostol was an effective
intervention for reducing blood loss during
TAH. However, the other trial (14) studying
32 women with the same dose of misoprostol and
the same administration route did not support
the beneficial effect of misoprostol.
In view of the aforementioned findings, it
seems that more studies are required for better
elucidation of this topic. Hence, we intended
to assess the efficacy of sublingual misoprostol
as a single dose administered before TAH on
intra-operative blood loss.
This was a randomized single-blinded controlled
clinical trial. The study population consisted
of women with large uterine fibroids who were
candidates for TAH with or without salpingo-oophorecyomy
(16 cases with uterine myoma and 14 cases with
AUB in the misoprostol group; 11 patients with
uterine myoma and 19 with AUB in the control
group). Exclusion criteria were previous history
of endometriosis, diabetes mellitus, obesity
(BMI > 30 kg/m2), history of myomectomy,
psychiatric disorders, taking GnRH agonists
before operation, invasive endometrial or cervical
cancers or ovarian malignancies. Also, any contraindication
for misoprostol use including mitral stenosis,
cardiac diseases, glaucoma, sickle cell anemia,
severe hypertension, diastolic blood pressure
of more than 100 mmHg, severe asthma, or severe
allergic reactions to prostaglandins were excluded.
The day before TAH, demographic characteristics
including age, weight, height, gravidity, and
parity were recorded. In addition, blood pressure,
body temperature, pulse rate at rest, and hemoglobin
level were recorded. The vital sign measurements
were made again before anesthesia induction
and any abnormalities were documented.
A total of 60 patients were included. Using
a random number table, the subjects were randomized
into one of the study groups. One group received
two tablets of misoprostol 200 mcg (Cytotec®,
Pfizer, NY, US) sublingually one hour before
TAH. The control group received two vitamin
B6 tablets sublingually.
The operations were done under general anesthesia
by a board-certified gynecologist. The variables
recorded were blood transfusion during and after
TAH (considering the hemodynamic situation of
the patient), operation duration (measured from
skin incision to skin closure), number of sterile
gauzes used during the procedure, the volume
of suction container, hemoglobin level 24 hours
after TAH, temperature after the operation,
and hospital stay duration. To measure the blood
loss volume, the gravimetric method was used
(15). In this method, the blood loss volume
(m) is calculated as adding the volume of suction
container (a) and weight difference of dry (b)
and moist (c) gauzes: m= a + (c-b)
Statistical analyses
Descriptive indices including frequency, percentage,
mean and its standard deviation were used to
express data. The normal distribution of the
continuous variables was determined using the
Kolmogorov-Smirnov test and histogram. In order
to compare quantitative variables with normal
distribution, the Student t test was used. The
comparison of continuous variables with non-normal
distribution was made using the Mann-Whitney
U test. To compare nominal variables, the Chi-square
test of the Fischer’s exact test was used.
The significance level was set at 0.05. All
analyses were performed using SPSS software
(ver. 20.0, IBM).
Ethics
The study protocol and objectives were explained
to the patients. Written consent was obtained
prior to enrollment. The Ethics Committee of our
medical university approved the study protocol.
This study was registered in the website of Iranian
Clinical Trial No. IRCT201610224025N8.
Baseline variables
Mean (±SD) age of the sample was 47.9
(±5.23) years (range, 37 to 66). Mean
(±SD) BMI (body mass index) value was
27.59 (3.82) kg/m2 (range, 22.3 to 37.3). The
two groups were comparable regarding age, weight,
height, BMI, gravidity, and parity (Table 1).
Mean (±SD) pre-operative hemoglobin values
in misoprostol and control group were respectively
11.86 (±2.26) and 11.80 (±1.81)
g/dL, P= 0.9.
Table 1: Comparison of demographic variables
between sublingual misoprostol and control (vitamin
B6) groups
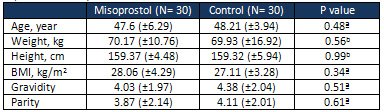
Data are presented as mean (±SD);
ª Student t test; b Mann-Whitney U test
Peri-operative variables
The mean (±SD) body temperature just
before anesthesia induction was significantly
higher in the misoprostol group (37.44±
0.55ºC) than in the control group (35.9
±6.78ºC); P= 0.01. Table 2 presents
comparison of the measured variables during
TAH between the two groups. Observed suction
container volume and blood loss volume were
significantly lower in the misoprostol group
compared to control group. Regarding need for
blood transfusion, one patient in the misoprostol
group and four patients in the control group
required transfusion (P= 0.16). TAH duration
was marginally shorter in the misoprostol group
(99.39± 17.79 min) compared to the control
group (109.5± 21.74 min): P= 0.058.
Table 2: Comparison of the variables related
to blood loss volume during total abdominal
hysterectomy between sublingual misoprostol
and control groups
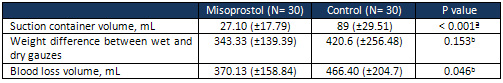 Data are presented as mean (SD); ª
Mann-Whitney U test; b Student’s t test
Data are presented as mean (SD); ª
Mann-Whitney U test; b Student’s t test
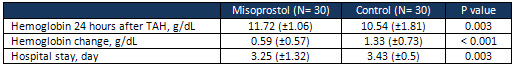
Post-operative variables
None of the patients in either group developed
fever after the operation. Table 3 shows hemoglobin
level 24 hours after the operation, change in
hemoglobin, and hospital stay. Hemoglobin drop
was significantly more prominent in the control
group. Also, hospitalization duration was shorter
in the misoprostol group.
Table 3: Comparison of hemoglobin change
after total abdominal hysterectomy and hospitalization
duration between sublingual misoprostol and
control groups
Hysterectomy
is
considered
the
most
common
gynecologic
procedure
performed
(3).
Hemorrhage
is
one
of
the
main
complications
of
hysterectomy
and
some
factors
affect
this
complication.
Perhaps,
the
most
important
factor
is
the
route
of
hysterectomy.
Blood
loss
in
abdominal
hysterectomy
is
more
severe
than
vaginal
or
laparoscopic
method
(16).
In
addition,
other
factors
that
can
affect
the
volume
of
blood
loss
are
technical
considerations,
obesity,
medications
(aspirin),
anatomy,
etc(3).
As
hemorrhage
increases
the
risk
of
blood
transfusion
and
post-operative
morbidities,
prevention
of
significant
blood
loss
is
one
of
the
main
priorities
in
TAH.
Efforts
have
been
done
in
order
to
determine
the
efficacy
of
various
pre-operative
methods
in
preventing
significant
blood
loss.
One
of
these
methods
is
use
of
uterotonic
medications
such
as
misoprostol.
As
stated
earlier
the
early
studies
which
used
misoprostol
in
this
field
relate
to
post-partum
hemorrhage
control
(either
alone
or
in
combination
with
oxytocin)
with
mixed
results
(7,
9-11).
More
studies
favor
the
usefulness
of
misoprostol
for
post-partum
hemorrhage
control.
Based
on
these
observations,
experts
started
to
study
misoprostol
in
gynecologic
procedures
such
as
abdominal
myomectomy
(1,
12,
17)
owing
to
its
uterotonic
effects
as
well
as
increasing
uterine
artery
resistance
(2).
The
results
of
these
studies
were
promising
as
reflected
in
a
systematic
review
on
283
patients
in
2015
and
noted
that
mean
difference
of
blood
loss
between
misoprostol
and
placebo
groups
was
-148.55
mL
per
operation
(95
%
CI,
-233.10
to
-64),
p
<
0.001
(18).
Based
on
the
current
findings,
misoprostol
was
an
effective
method
in
decreasing
blood
loss
and
hospital
stay
duration.
Although
the
need
for
blood
transfusion
was
not
statistically
significant,
more
patients
in
the
control
group
required
blood
transfusion
and
only
one
patient
in
the
misoprostol
group
required
such
intervention.
Although
studies
about
misoprostol
use
in
obstetrics
and
myomectomy
are
sufficient,
limited
studies
about
misoprostol
use
in
TAH,
as
the
most
common
gynecologic
procedure,
has
been
done.
In
a
previous
study
(2),
the
authors
studied
sublingual
misoprostol
for
TAH
(administered
half
an
hour
before
operation)
performed
in
132
women.
Mean
blood
loss
in
the
misoprostol
group
(356
mL)
was
significantly
lower
than
in
the
control
group
(435
mL).
This
finding
is
compatible
with
what
we
observed
herein.
According
to
our
findings,
hemoglobin
level
assayed
24
hours
after
TAH
was
significantly
higher
in
the
misoprostol
group.
This
is
in
agreement
with
the
previous
study
(2)
which
reported
mean
hemoglobin
level
of
10.5
in
the
misoprostol
group
which
was
higher
compared
to
the
control
group
(9.5
g/dL).
The
authors
did
not
find
any
significant
difference
regarding
hospital
stay.
In
contrast,
we
observed
that
patients
in
the
misoprostol
group
had
significantly
shorter
hospital
stay.
Another
study
(14)
investigated
sublingual
misoprostol
in
32
TAH
patients.
They
reported
that
blood
loss
in
the
misoprostol
group
was
on
average
570
mL
and
not
much
different
from
the
placebo
group
which
was
521
mL.
Also,
intra-operative
and
post-operative
rates
of
blood
transfusion
were
not
different
between
the
groups.
In
contrast
to
our
findings,
the
authors
of
the
mentioned
study
did
not
find
any
changes
in
hemoglobin
level.
The
misoprostol
dosage
(400
mcg)
and
route
of
administration
(sublingual)
is
identical
in
our
study
and
two
pertinent
previous
studies
(2,
14).
Misoprostol
dosage
and
administration
route
are
important
factors
in
studies.
Different
methods
of
administration
include
sublingual,
rectal,
or
vaginal
routes.
Bioavailability
of
misoprostol
is
higher
in
sublingual
method
compared
to
other
methods
(19).
Sublingual
misoprostol
(400
mcg)
administered
1
hour
before
TAH
was
effective
in
reducing
blood
loss
volume,
hemoglobin
drop,
and
hospitalization
duration.
Acknowledgement
This
paper
was
taken
from
the
thesis
of
Tayebe
Noori
as
a
requirement
to
receive
PhD
in
gynecology
from
Kermanshah
University
of
Medical
Sciences.
1.
Abdel-Hafeez
M,
Elnaggar
A,
Ali
M,
Ismail
AM,
Yacoub
M.
Rectal
misoprostol
for
myomectomy:
A
randomised
placebo-controlled
study.
Aust
N
Z
J
Obstet
Gynaecol
2015;55(4):363-8.
2.
Biswas
J,
Chaudhuri
P,
Mandal
A,
Bandyopadhyay
SN,
Dasgupta
S,
Pal
A.
Effect
of
a
single
preoperative
dose
of
sublingual
misoprostol
on
intraoperative
blood
loss
during
total
abdominal
hysterectomy.
Int
J
Gynaecol
Obstet
2013;122(3):244-7.
3.
Clarke-Pearson
DL,
Geller
EJ.
Complications
of
hysterectomy.
Obstet
Gynecol
2013;121(3):654-73.
4.
Maresh
MJ,
Metcalfe
MA,
McPherson
K,
Overton
C,
Hall
V,
Hargreaves
J,
et
al.
The
VALUE
national
hysterectomy
study:
description
of
the
patients
and
their
surgery.
Bjog
2002;109(3):302-12.
5.
Lethaby
A,
Vollenhoven
B,
Sowter
M.
Pre-operative
GnRH
analogue
therapy
before
hysterectomy
or
myomectomy
for
uterine
fibroids.
Cochrane
Database
Syst
Rev
2000(2):Cd000547.
6.
Okin
CR,
Guido
RS,
Meyn
LA,
Ramanathan
S.
Vasopressin
during
abdominal
hysterectomy:
a
randomized
controlled
trial.
Obstet
Gynecol
2001;97(6):867-72.
7.
Chaudhuri
P,
Majumdar
A.
Sublingual
misoprostol
as
an
adjunct
to
oxytocin
during
cesarean
delivery
in
women
at
risk
of
postpartum
hemorrhage.
Int
J
Gynaecol
Obstet
2015;128(1):48-52.
8.
Chaudhuri
P,
Mandi
S,
Mazumdar
A.
Rectally
administrated
misoprostol
as
an
alternative
to
intravenous
oxytocin
infusion
for
preventing
post-partum
hemorrhage
after
cesarean
delivery.
J
Obstet
Gynaecol
Res
2014;40(9):2023-30.
9.
El
Sharkwy
IA.
Carbetocin
versus
sublingual
misoprostol
plus
oxytocin
infusion
for
prevention
of
postpartum
hemorrhage
at
cesarean
section
in
patients
with
risk
factors:
a
randomized,
open
trail
study.
Archives
of
gynecology
and
obstetrics.
2013
Dec
1;288(6):1231-6.
10.
Tewatia
R,
Rani
S,
Srivastav
U,
Makhija
B.
Sublingual
misoprostol
versus
intravenous
oxytocin
in
prevention
of
post-partum
hemorrhage.
Arch
Gynecol
Obstet
2014;289(4):739-42.
11.
Owonikoko
KM,
Arowojolu
AO,
Okunlola
MA.
Effect
of
sublingual
misoprostol
versus
intravenous
oxytocin
on
reducing
blood
loss
at
cesarean
section
in
Nigeria:
a
randomized
controlled
trial.
J
Obstet
Gynaecol
Res
2011;37(7):715-21.
12.
Chang
FW,
Yu
MH,
Ku
CH,
Chen
CH,
Wu
GJ,
Liu
JY.
Effect
of
uterotonics
on
intra-operative
blood
loss
during
laparoscopy-assisted
vaginal
hysterectomy:
a
randomised
controlled
trial.
Bjog
2006;113(1):47-52.
13.
Park
H,
Yoon
BS,
Seong
SJ,
Kim
JY,
Shim
JY,
Park
CT.
Can
misoprostol
reduce
blood
loss
in
laparoscopy-assisted
vaginal
hysterectomy?
Aust
N
Z
J
Obstet
Gynaecol
2011;51(3):248-51.
14.
Chai
J,
Hon
E,
Li
CF,
Pun
TC,
Yeung
SB,
Ho
PC.
A
pilot
study
of
pre-operative
misoprostol
in
reducing
operative
blood
loss
during
hysterectomy.
Eur
J
Obstet
Gynecol
Reprod
Biol
2011;158(1):72-5.
15.
Johar
RS,
Smith
RP.
Assessing
gravimetric
estimation
of
intraoperative
blood
loss.
J
Gynecol
Surg
1993;9(3):151-4.
|

