|
Cholelithiasis and cholecystectomy
may lower the low density lipoprotein cholesterol
in plasma
Mehmet Rami Helvaci (1)
Mursel Davarci (2)
Orhan Veli Ozkan (3)
Ersan Semerci (3)
Abdulrazak Abyad (4)
Lesley Pocock (5)
(1) Specialist of Internal Medicine, M.D.
(2) Specialist of Urology, M.D.
(3) Specialist of General Surgery, M.D.
(4)Middle-East Academy for Medicine of Aging,
Chairman, M.D., MPH, MBA, AGSF
(5) medi-WORLD International
Correpondence:
Mehmet Rami Helvaci, M.D.
07400, ALANYA, Antalya, Turkey
Phone: 00-90-506-4708759
Email: mramihelvaci@hotmail.com
|
Abstract
Background:
We tried to understand whether or not
there is a significant relationship between
cholelithiasis and cholecystectomy and
plasma lipids.
Methods: The study was performed in the
Internal Medicine Polyclinics on routine
check up patients. All cases with cholelithiasis
or already performed cholecystectomy for
cholelithiasis were put into the first
group and age and sex-matched control
cases were put into the second group.
Results: One
hundred and forty-four cases either with
cholelithiasis or already performed cholecystectomy
for cholelithiasis were detected among
3,437 cases, totally (4.1%). One hundred
and sixteen (80.1%) of them were females
with a mean age of 53.6 years. Obesity
was significantly higher (54.8% versus
43.7%, p<0.01) in the cholelithiasis
group, and the mean body mass indexes
were 31.0 versus 28.9 kg/m2 in them, respectively
(p<0.01). Prevalence of hypertension
(26.3% versus 13.1%, p<0.001) and hypertriglyceridemia
(25.0% versus 18.0%, p<0.05) were also
higher in the cholelithiasis group, significantly.
On the other hand, hyperbetalipoproteinemia
was significantly lower in the cholelithiasis
group (9.7% versus 18.0%, p<0.05).
Conclusions:
There are significant relationships between
cholelithiasis and parameters of the metabolic
syndrome including age, female sex, obesity,
hypertension, and hypertriglyceridemia,
so cholelithiasis may also be found among
the terminal consequences of the metabolic
syndrome. On the other hand, cholelithiasis
may actually be a natural defence mechanism
of the body to decrease amount of cholesterol
absorbed via decreasing amount of bile
acids secreted during entrance of food
into the duodenum since cholelithiasis
and cholecystectomy may lower the low
density lipoprotein cholesterol in the
plasma.
Key words: Cholelithiasis, cholecystectomy,
metabolic syndrome, low density lipoprotein
cholesterol
|
Chronic endothelial damage may be the most
common type of vasculitis and the leading cause
of aging, morbidity, and mortality in human
beings. Much higher blood pressure (BP) of the
afferent vasculature may be the major underlying
cause by inducing recurrent injuries on endothelium,
and probably whole afferent vasculature including
capillaries are involved in the process. Thus
the term of venosclerosis is not as famous as
atherosclerosis in the literature. Secondary
to the chronic endothelial inflammation, edema,
and fibrosis, vascular walls become thickened,
their lumens are narrowed, and they lose their
elastic nature that reduces blood flow and increases
systolic BP further. Some of the well-known
causes and indicators of the inflammatory process
are sedentary life style, animal-rich diet,
overweight, smoking, alcohol, hypertriglyceridemia,
hyperbetalipoproteinemia, dyslipidemia, impaired
fasting glucose, impaired glucose tolerance,
white coat hypertension, and other chronic inflammatory
processes including rheumatologic disorders,
prolonged infections, and cancers for the development
of irreversible consequences including obesity,
hypertension, diabetes mellitus (DM), cirrhosis,
peripheric artery disease (PAD), chronic obstructive
pulmonary disease (COPD), chronic renal disease
(CRD), coronary artery disease (CAD), mesenteric
ischemia, osteoporosis, and stroke, all of which
terminate with early aging and death. Although
early withdrawal of causative factors may prevent
terminal consequences, after development of
cirrhosis, COPD, CRD, CAD, PAD, or stroke, endothelial
changes cannot be reversed, completely due to
their fibrotic nature. They were researched
under the titles of metabolic syndrome, aging
syndrome, or accelerated endothelial damage
syndrome in the literature, extensively (1-4).
On the other hand, gallstones are also found
among one of the most common health problems
in developed countries (5), and they are particularly
frequent in women above the age of 40 years
(6). Most of the gallstones are found in the
gallbladder with the definition of cholelithiasis.
Its pathogenesis is uncertain and appears to
be influenced by genetic and environmental factors
(7). Excess weight is a well-known and age-independent
risk factor for cholelithiasis (8). Delayed
bladder emptying, decreased small intestinal
motility, and sensitivity to cholecystokinin
were associated with obesity and cholelithiasis
(9). An increased risk was confirmed in obese
diabetics with hypertriglyceridemia (10), and
plasma cholesterol levels were also found related
with cholelithiasis (11). Even more conflicting
results were reported about the associations
between cholelithiasis and smoking (12-14).
We tried to understand whether or not there
is a significant relationship between cholelithiasis
and cholecystectomy and plasma lipids.
The study was performed in the Internal Medicine
Polyclinics of the Dumlupinar and Mustafa Kemal
Universities on routine check up patients between
August 2005 and November 2007. We took consecutive
patients below the age of 70 years to avoid
debility induced weight loss in elders. Their
medical histories including smoking habit, hypertension,
DM, dyslipidemia, and already used medications
and performed operations were learnt, and a
routine check up procedure including fasting
plasma glucose (FPG), triglyceride, high density
lipoprotein cholesterol (HDL-C), low density
lipoprotein cholesterol (LDL-C), and an abdominal
ultrasonography were performed. Patients with
devastating illnesses including type 1 DM, malignancies,
acute or chronic renal failure, chronic liver
diseases, hyper- or hypothyroidism, and heart
failure were excluded to avoid their possible
effects on weight. Current daily smokers for
the last six months and cases with a history
of five pack-years were accepted as smokers.
Cigar or pipe smokers were excluded. Body mass
index (BMI) of each case was calculated by the
measurements of the same physician instead of
verbal expressions since there is evidence that
heavier individuals systematically underreport
their weight (15). Weight in kilograms is divided
by height in meters squared, and underweight
is defined as a BMI of lower than 18.5, normal
weight as lower than 24.9, overweight as lower
than 29.9, and obesity as a BMI of 30.0 kg/m2
or higher (16). Cases with an overnight FPG
level of 126 mg/dL or greater on two occasions
or already receiving antidiabetic medications
were defined as diabetics (16). An oral glucose
tolerance test with 75-gram glucose was performed
in cases with a FPG level between 110 and 125
mg/dL, and diagnosis of cases with a 2-hour
plasma glucose level 200 mg/dL or greater is
DM (16). Patients with dyslipidemia were detected,
and we used the National Cholesterol Education
Program Expert Panel’s recommendations
for defining dyslipidemic subgroups (16). Dyslipidemia
is diagnosed when LDL-C is 160 or higher and/or
triglyceride is 200 or higher and/or HDL-C is
lower than 40 mg/dL. Office BP was checked after
a 5-minute rest in seated position with a mercury
sphygmomanometer on three visits, and no smoking
was permitted during the previous 2 hours. A
10-day twice daily measurement of blood pressure
at home (HBP) was obtained in all cases, even
in normotensives in the office due to the risk
of masked hypertension after a 10-minute education
session about proper BP measurement techniques
(17). The education included recommendation
of upper arm while discouraging wrist and finger
devices, using a standard adult cuff with bladder
sizes of 12 x 26 cm for arm circumferences up
to 33 cm in length and a large adult cuff with
bladder sizes of 12 x 40 cm for arm circumferences
up to 50 cm in length, and taking a rest at
least for a period of 5 minutes in the seated
position before measurement. An additional 24-hour
ambulatory BP monitoring was not required due
to the equal efficacy of the method with HBP
measurement to diagnose hypertension (18). Eventually,
hypertension is defined as a BP of 135/85 mmHg
or greater on HBP measurements (17). Cholelithiasis
was diagnosed ultrasonographically. Eventually,
all cases either with presenting cholelithiasis
or already performed cholecystectomy for cholelithiasis
were put into the first group and age and sex-matched
control cases were put into the second group.
Prevalence of smoking, normal weight, overweight,
obesity, hypertension, DM, hypertriglyceridemia,
hyperbetalipoproteinemia, and dyslipidemia and
mean BMI values were detected in both groups
and compared. Mann-Whitney U test, Independent-Samples
t test, and comparison of proportions were used
as the methods of statistical analyses.
Although the exclusion criteria, 119 cases
with cholecystectomy for cholelithiasis and
25 cases with already presenting asymptomatic
cholelithiasis were detected among 3,437 cases,
totally (4.1%). One hundred and sixteen (80.1%)
of them were females with a mean age of 53.6
years, so cholelithiasis is mainly a disorder
of females in their fifties. Prevalence of smoking
was similar in the cholelithiasis and control
groups (18.0% versus 19.4%, p>0.05, respectively).
There was not any patient with underweight.
Interestingly, 92.3% (133 cases) of the cholelithiasis
group had excess weight and only 7.6% (11 cases)
had normal weight. Obesity was significantly
higher (54.8% versus 43.7%, p<0.01) and normal
weight was significantly lower (7.6% versus
18.0%, p<0.01) in the cholelithiasis group.
Mean BMI values were 31.0 and 28.9 kg/m2, (p<0.01)
in the two groups. Probably parallel to the
higher mean BMI values, prevalence of hypertension
(26.3% versus 13.1%, p<0.001) and hypertriglyceridemia
(25.0% versus 18.0%, p<0.05) were also higher
in the cholelithiasis group, significantly.
Although the prevalence of DM (20.8% versus
19.4%, p>0.05) and dyslipidemia (31.9% versus
29.8%, p>0.05) were also higher in the cholelithiasis
groups, differences were nonsignificant probably
due to the small sample sizes of the groups.
On the other hand, hyperbetalipoproteinemia
was significantly lower in the cholelithiasis
group (9.7% versus 18.0%, p<0.05) (Table
1).
Table 1: Comparison of cases with and without
cholelithiasis
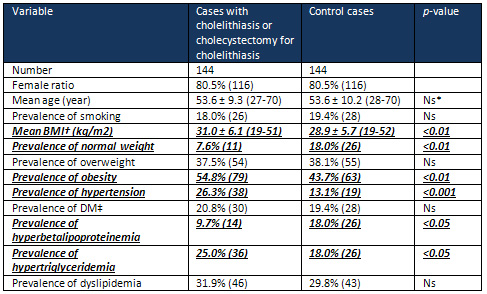
*Nonsignificant (p>0.05) †Body mass
index ‡Diabetes mellitus
Bile
is
formed
in
the
liver
as
an
isosmotic
solution
of
bile
acids,
cholesterol,
phospholipids,
bilirubin,
and
electrolytes.
Bile
flow
is
generated
by
the
active
transport
of
bile
salts
and
electrolytes
and
the
accompanying
obligate
passive
movement
of
water.
The
liver
synthesizes
water-soluble
bile
acids
from
water-insoluble
cholesterol.
Bile
acids
are
excreted
in
bile,
which
flows
from
the
intrahepatic
collecting
system
into
the
proximal
or
common
hepatic
duct.
About
50%
of
bile
secreted
in
the
fasting
state
passes
into
the
gallbladder
via
the
cystic
duct
and
the
rest
flows
directly
into
the
distal
or
common
bile
duct.
So
gallbladder
filling
is
facilitated
during
fasting.
Up
to
90%
of
water
in
the
gallbladder
bile
is
absorbed
as
an
electrolyte
solution,
and
bile
remaining
in
the
gallbladder
is
a
concentrated
solution
consisting
primarily
of
bile
acids.
So
during
fasting,
bile
acids
are
concentrated
in
the
gallbladder,
and
a
small
amount
of
bile
flows
from
the
liver.
Food
entering
the
duodenum
stimulates
gallbladder
contraction,
releasing
much
of
body
pool
(3
to
4
g)
of
bile
acids
into
the
small
intestine.
Bile
flows
into
the
duodenum
to
mix
with
food
content
and
to
perform
its
several
functions
including
solubilization
of
dietary
cholesterol,
fats,
and
fat-soluble
vitamins
to
facilitate
their
absorption
in
the
form
of
mixed
micelles,
causing
water
secretion
by
the
colon
as
they
enter
that
organ
thus
promoting
catharsis,
excretion
of
bilirubin
as
degradation
products
of
heme
compounds
from
worn-out
red
blood
cells,
excretion
of
drugs,
ions,
and
endogenously
produced
compounds
from
the
body,
and
secretion
of
various
proteins
important
in
gastrointestinal
function.
About
90%
of
bile
acids
is
absorbed
in
the
terminal
ileum
into
the
portal
venous
circulation
by
active
transport.
Bile
salts
are
efficiently
extracted
by
the
liver,
and
secreted
back
into
bile.
Bile
acids
undergo
enterohepatic
circulation
10
to
12
times
per
day.
During
each
pass,
a
small
amount
of
primary
bile
acids
reaches
the
colon,
where
anaerobic
bacteria
containing
7alpha-hydroxylase
form
secondary
bile
acids.
The
most
clinical
disorders
of
the
extrahepatic
biliary
tract
are
related
to
gallstones.
In
the
USA,
20%
of
people
above
the
age
of
65
years
have
gallstones,
and
each
year
more
than
500,000
patients
undergo
cholecystectomy.
Factors
that
increase
the
probability
of
gallstones
include
age,
female
sex,
and
obesity.
Highly
water-insoluble
cholesterol
is
the
major
component
of
most
gallstones.
Biliary
cholesterol
is
solubilized
in
the
bile
salt-phospholipid
micelles
and
phospholipid
vesicles
which
greatly
increase
the
cholesterol-carrying
capacity
of
bile.
The
amount
of
cholesterol
carried
in
micelles
and
vesicles
varies
with
the
bile
salt
secretion
rate.
Supersaturation
of
cholesterol
in
bile
is
a
necessary
condition
of
cholesterol
gallstone
formation.
Virtually
all
gallstones
form
within
the
gallbladder
but
stones
may
form
in
the
bile
duct
after
cholecystectomy
or
behind
strictures
as
a
result
of
stasis.
In
another
perspective,
cholelithiasis
may
actually
be
a
natural
defence
mechanism
of
the
body
to
decrease
amount
of
cholesterol
absorbed
via
decreasing
amount
of
bile
acids
secreted
during
entrance
of
food
into
the
duodenum.
Similarly,
bile
acid
sequestrants
including
cholestyramine
and
cholestipol
effectively
lower
serum
LDL-C
by
binding
bile
acids
in
intestine
and
interrupting
enterohepatic
circulation
of
them.
Excess
weight
leads
to
both
structural
and
functional
abnormalities
of
many
organ
systems
of
the
body.
Recent
studies
revealed
that
adipose
tissue
produces
biologically
active
leptin,
tumor
necrosis
factor-alpha,
plasminogen
activator
inhibitor-1,
and
adiponectin
which
are
closely
related
with
the
development
of
complications
(19).
For
example,
the
cardiovascular
field
has
recently
shown
a
great
interest
in
the
role
of
inflammation
in
the
development
of
atherosclerosis
and
numerous
studies
indicated
that
inflammation
plays
a
significant
role
in
the
pathogenesis
of
atherosclerosis
and
thrombosis
(20,
21).
Adipose
tissue
is
involved
in
the
regulation
of
cytokines
(22).
On
the
other
hand,
individuals
with
excess
weight
will
have
an
increased
circulating
blood
volume
as
well
as
an
increased
cardiac
output,
thought
to
be
the
result
of
increased
oxygen
demand
of
the
excessive
fat
tissue.
The
prolonged
increase
in
circulating
blood
volume
can
lead
to
myocardial
hypertrophy
and
decreased
compliance,
in
addition
to
the
common
comorbidity
of
hypertension.
In
addition
to
the
hypertension,
the
prevalence
of
high
FPG,
high
serum
total
cholesterol,
and
low
HDL-C,
and
their
clustering
were
all
raised
with
the
higher
BMI
(23).
Combination
of
these
cardiovascular
risk
factors
will
eventually
lead
to
an
increase
in
left
ventricular
stroke
work
with
higher
risks
of
arrhythmias,
cardiac
failure,
and
sudden
cardiac
death.
Similarly,
the
incidence
of
CHD
and
stroke
have
increased
with
a
higher
BMI
in
other
studies
(23,
24),
and
risk
of
death
from
all
causes
including
cancers
increases
throughout
the
range
of
moderate
and
severe
excess
weight
for
both
genders
in
all
age
groups
(25).
As
another
consequence
of
excess
weight
on
health,
the
cholelithiasis
cases
had
a
significantly
higher
mean
BMI
value
in
the
present
study
(31.0
versus
28.9
kg/m2,
p<0.01)
similar
to
the
previous
reports
(8,
9).
Probably
as
a
consequence
of
the
significantly
higher
BMI,
the
prevalence
of
hypertension
(26.3%
versus
13.1%,
p<0.001)
and
hypertriglyceridemia
(25.0%
versus
18.0%,
p<0.05)
were
also
higher
in
the
cholelithiasis
group.
The
relationship
between
excess
weight
and
elevated
BP
and
hypertriglyceridemia
has
already
been
described
in
the
metabolic
syndrome
or
aging
syndrome,
or
accelerated
endothelial
damage
syndrome
(26),
and
clinical
manifestations
of
the
syndrome
include
obesity,
dyslipidemia,
hypertension,
insulin
resistance,
and
proinflammatory
as
well
as
prothrombotic
states
(27).
The
above
confirmed
increased
risk
of
cholelithiasis
in
obese
diabetics
with
hypertriglyceridemia
may
also
be
an
indicator
of
its
association
with
the
metabolic
syndrome
(10,
26).
Although
the
presence
of
some
conflicting
results
in
the
literature
(12-14),
we
did
not
find
any
significant
association
between
cholelithiasis
and
smoking
in
the
present
study
(p>0.05).
Although
the
waist
circumference,
BMI,
hypertension,
fasting
glycemia,
insulinemia
and
insulin
resistance
index
indicated
significant
differences
in
the
cholelithiasis
and
cholecystectomy
group
in
patients
with
the
metabolic
syndrome,
there
was
no
significant
differences
for
the
lipid
parameters
in
another
study
(28).
Plasma
concentration
of
total
cholesterol,
triglycerides,
and
LDL-C
were
significantly
reduced
in
patients
on
day
3
of
surgery
and
6
months
after
the
cholecystectomy
in
another
study
(29).
Significantly
higher
prevalence
of
cholelithiasis
was
found
among
patients
with
nonalcoholic
fatty
liver
disease
(NAFLD)
(47%
versus
26%,
p<
0.0001),
and
type
2
DM,
overweight,
obesity,
and
cholelithiasis
were
identified
as
independent
predictors
of
NAFLD
(30).
Fifty
six
percent
of
patients
with
cholelithiasis
had
NAFLD
compared
with
33%
of
patients
without
(p<
0.0001)
(30).
Age
above
50
years,
triglycerides
above
1.7
mmol/l,
overweight,
obesity,
and
total
cholesterol
concentration
were
the
independent
predictors
of
cholelithiasis
(30).
So
NAFLD
may
represent
a
pathogenetic
link
between
the
metabolic
syndrome
and
cholelithiasis
(30).
Serum
LDL-C
values
of
patients
with
cholelithiasis
above
the
age
of
40
years
were
significantly
elevated
(p<0.05)
in
another
study
(31).
Patients
with
type
2
DM
had
higher
probability
of
having
cholelithiasis,
and
age,
female
sex,
and
higher
BMI
were
independently
associated
with
cholelithiasis
(32).
Authors
have
concluded
that
obesity
may
lead
to
fatty
infiltration
of
multiple
organs
causing
organ
dysfunction,
and
BMI
was
associated
with
steatocholecystitis
in
another
study
(33).
As
a
conclusion,
there
are
significant
relationships
between
cholelithiasis
and
parameters
of
the
metabolic
syndrome
including
age,
female
sex,
obesity,
hypertension,
and
hypertriglyceridemia,
so
cholelithiasis
may
also
be
found
among
the
terminal
consequences
of
the
metabolic
syndrome.
On
the
other
hand,
cholelithiasis
may
actually
be
a
natural
defence
mechanism
of
the
body
to
decrease
the
amount
of
cholesterol
absorbed
via
decreasing
amount
of
bile
acids
secreted
during
entrance
of
food
into
the
duodenum
since
cholelithiasis
and
cholecystectomy
may
lower
LDL-C
in
the
plasma.
1.
Eckel
RH,
Grundy
SM,
Zimmet
PZ.
The
metabolic
syndrome.
Lancet
2005;
365:
1415-1428.
2.
Helvaci
MR,
Kaya
H,
Sevinc
A,
Camci
C.
Body
weight
and
white
coat
hypertension.
Pak
J
Med
Sci
2009;
25:
6:
916-921.
3.
Helvaci
MR,
Aydin
LY,
Aydin
Y.
Digital
clubbing
may
be
an
indicator
of
systemic
atherosclerosis
even
at
microvascular
level.
HealthMED
2012;
6:
3977-3981.
4.
Helvaci
MR,
Aydin
Y,
Gundogdu
M.
Atherosclerotic
effects
of
smoking
and
excess
weight.
J
Obes
Wt
Loss
Ther
2012;
2:
7.
5.
Tazuma
S.
Gallstone
disease:
Epidemiology,
pathogenesis,
and
classification
of
biliary
stones
(common
bile
duct
and
intrahepatic).
Best
Pract
Res
Clin
Gastroenterol
2006;
20:
1075–1083.
6.
Katsika
D,
Grjibovski
A,
Einarsson
C,
Lammert
F,
Lichtenstein
P,
Marschall
HU.
Genetic
and
environmental
influences
on
symptomatic
gallstone
disease:
a
Swedish
study
of
43,141
twin
pairs.
Hepatology
2005;
41:
1138–1143.
7.
Lammert
F,
Sauerbruch
T.
Mechanisms
of
disease:
the
genetic
epidemiology
of
gallbladder
stones.
Nat
Clin
Pract
Gastroenterol
Hepatol
2005;
2:
423–433.
8.
Erlinger
S.
Gallstones
in
obesity
and
weight
loss.
Eur
J
Gastroenterol
Hepatol
2000;
12:
1347–1352.
9.
Mathus-Vliegen
EM,
Van
Ierland-Van
Leeuwen
ML,
Terpstra
A.
Determinants
of
gallbladder
kinetics
in
obesity.
Dig
Dis
Sci
2004;
49:
9–16.
10.
Fraquelli
M,
Pagliarulo
M,
Colucci
A,
Paggi
S,
Conte
D.
Gallbladder
motility
in
obesity,
diabetes
mellitus
and
coeliac
disease.
Dig
Liver
Dis
2003;
35:
12–16.
11.
Devesa
F,
Ferrando
J,
Caldentey
M,
Borghol
A,
Moreno
MJ,
Nolasco
A,
et
al.
Cholelithiasic
disease
and
associated
factors
in
a
Spanish
population.
Dig
Dis
Sci
2001;
46:
1424–1436.
12.
Kono
S,
Eguchi
H,
Honjo
S,
Todoroki
I,
Oda
T,
Shinchi
K,
et
al.
Cigarette
smoking,
alcohol
use,
and
gallstone
risk
in
Japanese
men.
Digestion
2002;
65:
177–183.
13.
Okamoto
M,
Yamagata
Z,
Takeda
Y,
Yoda
Y,
Kobayashi
K,
Fujino
MA.
The
relationship
between
gallbladder
disease
and
smoking
and
drinking
habits
in
middle-aged
Japanese.
J
Gastroenterol
2002;
37:
455–462.
14.
Jorgensen
T.
Gall
stones
in
a
Danish
population.
Relation
to
weight,
physical
activity,
smoking,
coffee
consumption,
and
diabetes
mellitus.
Gut
1989;
30:
528–534.
15.
Bowman
RL,
DeLucia
JL.
Accuracy
of
self
reported
weight:
a
meta-analysis.
Behav
Ther
1992;
23:
637-635.
16.
Third
Report
of
the
National
Cholesterol
Education
Program
(NCEP)
Expert
Panel
on
Detection,
Evaluation,
and
Treatment
of
High
Blood
Cholesterol
in
Adults
(Adult
Treatment
Panel
III)
final
report.
Circulation
2002;
106:
3143–3421.
17.
O’Brien
E,
Asmar
R,
Beilin
L,
Imai
Y,
Mallion
JM,
Mancia
G,
et
al.
European
Society
of
Hypertension
recommendations
for
conventional,
ambulatory
and
home
blood
pressure
measurement.
J
Hypertens
2003;
21:
821–848.
18.
Helvaci
MR,
Seyhanli
M.
What
a
high
prevalence
of
white
coat
hypertension
in
society!
Intern
Med
2006;
45:
671–674.
19.
Funahashi
T,
Nakamura
T,
Shimomura
I,
Maeda
K,
Kuriyama
H,
Takahashi
M,
et
al.
Role
of
adipocytokines
on
the
pathogenesis
of
atherosclerosis
in
visceral
obesity.
Intern
Med
1999;
38:
202–206.
20.
Widlansky
ME,
Gokce
N,
Keaney
JF
Jr,
Vita
JA.
The
clinical
implications
of
endothelial
dysfunction.
J
Am
Coll
Cardiol
2003;
42:
1149–1160.
21.
Ridker
PM.
High-sensitivity
C-reactive
protein:
Potential
adjunct
for
global
risk
assessment
in
the
primary
prevention
of
cardiovascular
disease.
Circulation
2001;
103:
1813–1818.
22.
Yudkin
JS,
Stehouwer
CD,
Emeis
JJ,
Coppack
SW.
C-reactive
protein
in
healthy
subjects:
associations
with
obesity,
insulin
resistance,
and
endothelial
dysfunction:
a
potential
role
for
cytokines
originating
from
adipose
tissue?
Arterioscler
Thromb
Vasc
Biol
1999;
19:
972–978.
23.
Zhou
B,
Wu
Y,
Yang
J,
Li
Y,
Zhang
H,
Zhao
L.
Overweight
is
an
independent
risk
factor
for
cardiovascular
disease
in
Chinese
populations.
Obes
Rev
2002;
3:
147–156.
24.
Zhou
BF.
Effect
of
body
mass
index
on
all-cause
mortality
and
incidence
of
cardiovascular
diseases--report
for
meta-analysis
of
prospective
studies
open
optimal
cut-off
points
of
body
mass
index
in
Chinese
adults.
Biomed
Environ
Sci
2002;
15:
245–252.
25.
Calle
EE,
Thun
MJ,
Petrelli
JM,
Rodriguez
C,
Heath
CW
Jr.
Body-mass
index
and
mortality
in
a
prospective
cohort
of
U.S.
adults.
N
Engl
J
Med
1999;
341:
1097–1105.
26.
Helvaci
MR,
Kaya
H,
Gundogdu
M.
Association
of
increased
triglyceride
levels
in
metabolic
syndrome
with
coronary
artery
disease.
Pak
J
Med
Sci
2010;
26:
667-672.
27.
Tonkin
AM.
The
metabolic
syndrome(s)?
Curr
Atheroscler
Rep
2004;
6:
165–166.
28.
Cojocaru
C,
Pandele
GI.
Metabolic
profile
of
patients
with
cholesterol
gallstone
disease.
Rev
Med
Chir
Soc
Med
Nat
Iasi
2010;114:
677-682.
29.
Malik
AA,
Wani
ML,
Tak
SI,
Irshad
I,
Ul-Hassan
N.
Association
of
dyslipidaemia
with
cholelithiasis
and
effect
of
cholecystectomy
on
the
same.
Int
J
Surg
2011;
9:
641-642.
30.
Koller
T,
Kollerova
J,
Hlavaty
T,
Huorka
M,
Payer
J.
Cholelithiasis
and
markers
of
nonalcoholic
fatty
liver
disease
in
patients
with
metabolic
risk
factors.
Scand
J
Gastroenterol
2012;
47:
197-203.
31.
Batajoo
H,
Hazra
NK.
Analysis
of
serum
lipid
profile
in
cholelithiasis
patients.
J
Nepal
Health
Res
Counc
2013;
11:
53-55.
32.
Sodhi
JS,
Zargar
SA,
Khateeb
S,
Showkat
A,
Javid
G,
Laway
BA,
et
al.
Prevalence
of
gallstone
disease
in
patients
with
type
2
diabetes
and
the
risk
factors
in
North
Indian
population:
a
case
control
study.
Indian
J
Gastroenterol
2014;
33:
507-511.
33.
Yoon
JH,
Kim
YJ,
Baik
GH,
Kim
YS,
Suk
KT,
Kim
JB,
et
al.
The
Impact
of
Body
Mass
Index
as
a
Predictive
Factor
of
Steatocholecystitis.
Hepatogastroenterology
2014;
61:
902-907.
|

