|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
........................................................
|
|
Original contribution/Clinical Investigation
Diabetes
Mellitus - Knowledge, Management and Complications:
Survey report from Faisalabad-Pakistan
Ijaz Anwer, Ahmad Shahzad, Kashmira Nanji, Farah
Haider, Muhammad Masood Ahmad
Alanine
aminotransferase indicates excess weight and
dyslipidemia
Mehmet Rami Helvaci, Orhan Ayyildiz* Mustafa
Cem Algin, Yusuf Aydin, Abdulrazak Abyad, Lesley
Pocock
Comparative Analysis of Antimicrobial Peptides
Gene Expression in Susceptible/Resistant Mice
Macrophages to Leishmania major Infection
Hamid Daneshvar, Iraj Sharifi, Alireza Kyhani,
Amir Tavakoli Kareshk, Arash Asadi
Does
socio-economic status of the patients have effect
on clinical outcomes after coronary artery bypass
grafting surgery?
Forough Razmjooei, Afshin Mansourian, Saeed
Kouhpyma
Comparison
of the uterine artery Doppler indices during
pregnancy between gestational diabetes and diabetes
mellitus and healthy pregnant women
Nazanin Farshchian, Farhad Naleini, Amir Masoud
Jaafarnejhad,
Parisa Bahrami Kamangar
Survey
single dose Gentamicin in treatment of UTI in
children with range of 1 month to 13 years old
in Jahrom during 2015
Ehsan Rahmanian, Farideh Mogharab,
Vahid Mogharab
Evaluation
of control of bleeding by electro cauterization
of bleeding points of amplatz sheath tract after
percutaneous nephrolithotomy (PCNL) in Jahrom
Peymanieh hospital during year 2015-2016
Ali Reza Yousefi , Reza Inaloo
Comparison
of the three-finger tracheal palpation technique
with triple ID formula to determine endotracheal
tube depth in children 2-8 years in 2016-2017
Anahid Maleki, Alireza Ebrahim Soltani, Alireza
Takzare, Ebrahim Espahbodi,
Mehrdad Goodarzi , Roya Noori
Effect
of Sevoflurane and Propofol on pulmonary arterial
pressure during cardiac catheterization in children
with congenital heart diseases
Faranak Behnaz, Mahshid Ghasemi , Gholamreza
Mohseni, Azim Zaraki
Population and Community Studies
Prevalence
and risk factors of obesity in children aged
2-12 years in the Abu Dhabi Islands
Eideh Al-Shehhi, Hessa Al-Dhefairi, Kholoud
Abuasi, Noora Al Ali, Mona Al Tunaiji, Ebtihal
Darwish
Study
and comparison of psychological disorders in
normal students and students with multiple sclerosis
in Shahrekord
Neda Ardestani-Samani, Mohammad Rabiei, Mohammad
Ghasemi-Pirbalooti, Asghar Bayati, Saeid Heidari-Soureshjani
Comparative
study of self-concept, physical self-concept,
and time perspective between the students with
multiple sclerosis and healthy students in Shahrekord
Neda Ardestani-Samani, Mohammad Rabiei, Mohammad
Ghasemi-Pirbalooti, Asghar Bayati, Saeid Heidari-Soureshjani
Relationship
between Coping Styles and Religious Orientation
with Mental Health in the Students of the Nursing-Midwifery
Faculty of Zabol
Nasim Dastras, Mohsen Heidari Mokarrar, Majid
Dastras, Shirzad Arianmehr
Tuberculosis
in Abadan, Iran (2012-2016): An Epidemiological
Study
Ali-Asghar ValiPour, Azimeh Karimyan, Mahmood
Banarimehr, Marzieh Ghassemi, Maryam Robeyhavi,
Rahil Hojjati,
Parvin Gholizadeh
Family
Stability and Conflict of Spiritual Beliefs
and Superstitions among Yazdi People in Iran:
A Qualitative Study
Zahra Pourmovahed , Seyed Saied Mazloomy Mahmoodabad
; Hassan Zareei Mahmoodabadi ; Hossein Tavangar
; Seyed Mojtaba Yassini Ardekani ; Ali Akbar
Vaezi
A
comparative study of the self-actualization
in psychology and Islam
Simin Afrasibi, Zakieh Fattahi
The
effectiveness of cognitive - behavioral therapy
in reducing the post-traumatic stress symptoms
in male students survivors of earthquake in
the central district of Varzeghan
Sakineh Salamat, Dr.Ahad Ahangar, Robab Farajzadeh
Reviews
Effects
and mechanisms of medicinal plants on stress
hormone (cortisol): A systematic review
Kamal Solati, Saeid Heidari-Soureshjani, Lesley
Pocock
Comparing
Traditional and medical treatments for constipation
: A Review Article
Mohammad Yaqub Rajput
A review
of anti-measles and anti-rubella antibodies
in 15- 25 year old women in Jahrom City in 2011
Ehsan Rahmania , Farideh Mogharab, Vahid Mogharab
Review
of percutaneous nephrolithotomy in children
below 12 years old in Jahrom hospital, during
2010-2014
Ali Reza Yousefi , Reza Inaloo
Physical
and mental health in Islam
Bahador Mehraki, Abdollah Gholami
International Health Affairs
The Challenges
of Implementation of Professional Ethics Standards
in Clinical Care from the viewpoint of Nursing
Students and Nurses
Saeedeh Elhami, Kambiz Saberi, Maryam Ban, Sajedeh
Mousaviasl, Nasim Hatefi Moadab, Marzieh Ghassemi
Cognitive
Determinants of Physical Activity Intention among
Iranian Nurses: An Application of Integrative
Model of Behavior Prediction
Arsalan Ghaderi, Firoozeh Mostafavi, Behzad Mahaki,
Abdorrahim Afkhamzadeh,
Yadolah Zarezadeh , Erfan Sadeghi
Effect
of resilience-based intervention on occupational
stress among nurses
Hossein Jafarizadeh, Ebrahim Zhiyani, Nader
Aghakhani, Vahid Alinejad, Yaser Moradi
Education and Training
Calculation
of Salaries and Benefits of Faculty Members
in the Ministry of Health and Medical Education
of Iran
Abdolreza Gilavand
The
effect of education on self-care behaviors of
gastrointestinal side effects on patients undergoing
chemotherapy
Shokoh Varaei, Ehsan Abadi Pishe, Shadan Pedram
Razie, Lila Nezam Abadi Farahani
Creating
and Validating the Faith Inventory for Students
at Islamic Azad University of Ahvaz
Solmaz Choheili, Reza Pasha, Gholam Hossein
Maktabi, Ehsan Moheb
Creating
and Validating the Adjustment Inventory for
the Students of Islamic Azad University of Ahvaz
Homa Choheili, Reza Pasha, Gholam Hossein Maktabi,
Ehsan Moheb
Evaluating
the Quality of Educational Services from the
Viewpoints of Radiology Students of Ahvaz Jundishapur
University of Medical Sciences
Abdolreza Gilavand, Jafar Fatahiasl
An
Investigation of Psychosocial aspect of Iranian
Nursing Students' Clinical Setting
Mahsa Boozaripour , Zanyar Karimi, Sima Zohari
Anbohi, Amir Almasi-Hashiani, Fariba Borhani
Clinical Research and Methods
Comparison
of the Antibacterial Effects of Chlorhexidine
Mouth washes with Jaftex Mouth wash on Some
Common Oral Microorganisms (An in Vitro Study)
Ebrahim Babadi, Zahra Bamzadeh, Fatemeh Babadi
Study
of the effect of plasma jet on Fusarium isolates
with ability to produce DON toxins
Elham Galin Abbasian, Mansour Bayat, Arash chaichi
Nosrati, Seyed Jamal Hashemi, Mahmood Ghoranneviss
The
comparison of anti-inflammatory effect in two
methods of topical dexamethasone injection and
topical application of ginger alcoholic extract
after removing mandibular wisdom teeth
Sahar Zandi, Seyyed Muhammadreza Alavi, Kamran
Mirzaie, Ramin Seyedian, Narges Aria, Saman
Jokar
The effect
of curcumin on growth and adherence of major
microorganisms causing tooth decay
Leila Helalat, Ahmad Zarejavid, Alireza Ekrami,
Mohammd Hosein Haghighizadeh, Mehdi Shiri Nasab
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| November 2017
- Volume 15, Issue 9 |
|
|
Comparison of the three-finger
tracheal palpation technique with triple ID
formula to determine endotracheal tube depth
in children 2-8 years in 2016-2017
Anahid Maleki (1)
Alireza Ebrahim Soltani (2)
Alireza Takzare (1)
Ebrahim Espahbodi (1)
Mehrdad Goodarzi (1)
Roya Noori (3)
(1) Assistant Professor of Medicine, Faculty
of Medicine, Tehran University of Medical Sciences
(2) Associated Professor… of Medicine,
Faculty of Medicine, Tehran University of Medical
Sciences
(3) General physician, Tehran University of
Medical Sciences
Corresponding author:
Anahid Maleki
Assistant Professor of Medicine,
Faculty of Medicine, Tehran University of Medical
Sciences
Tehran, Iran
Email: A-maleki@tums.ac.ir
|
Abstract
Background and objective:
Correct placement of the endotracheal
tube is an important part of anesthesia
and special care, and it is especially
important in pediatric patients. The common
methods and tools used to determine the
proper depth of the tube trachea have
significant limitations. The aims of the
present study were to evaluate accuracy
and error rate of the three-finger tracheal
palpation technique and compare it with
triple ID formulae technique in children
aged 2-8 years in 2016-2017.
Methods:
In this study, 100 children aged 2 to
8 years who were nominated for elective
surgery with general anesthesia requiring
intubation, were selected after receiving
written consent from their parents about
their satisfaction with the study. Patients
were excluded from the study by exclusion
criteria including abnormal anatomy of
airways, or chest surface anatomy, history
of active respiratory or cold infection
in the past 3 weeks, history of chronic
respiratory disease, asthma, and allergy.
Each group consisted of 50 children and
in both groups of children with premedication
with metidazolam 0.5 mg / kg and ketamine
5 mg / kg orally. After entering the operating
room, the installation of standard monitoring
equipment, pulse oximetry, ECG, noninvasive
blood pressure, induction of anesthesia
in the operating room with sevoflurane
(8%) was instituted, and continued with
2 liters per minute of anesthesia. After
adequate anesthetic depth, venous thrombosis
was performed with angioquate 22, and
after thiopental injection of sodium 5
mg / kg, tracheal intubation began. In
the first group, an anesthetist tested
the tube with a formula of three times
the diameter of the tube and compared
with the auxiliary auscultation of the
tube. Also, the duration of intubation
was measured and recorded. In the second
group, an experienced anesthetist experienced
three-finger touch procedure, the endotracheal
tube was exposed from the chip and after
tubing passed through the supra sternal,
the tube was fixed. Then, the tube was
controlled by bilateral anesthetic tube
and the duration of intubation was measured
and recorded. The tube was transmitted
by an experienced anesthetist and was
touched by an anesthetist technician in
the supra-standard. Finally, the accuracy
and error rates of the two methods were
compared. The obtained data and probable
complications were recorded and analyzed
statistically.
Results:
Comparison of two methods in terms of
success rate (correct insertion of the
tube confirmed by bilateral lumbar auscultation)
showed that there was no significant difference
in determining the depth of the tracheal
tube between the two groups (p = 0.15).
The depth of the tube in the three-finger
touch procedure was significantly different
from the three-fold method (p = 0.00).
Also, the duration of intubation between
the two groups was significantly different
(p = 0.00). The two methods were similar
in the course of intubation, and no complications
occurred during intubation.
Discussion
and conclusion: Overall, this study
showed that the use of the three-finger
tracheal palpation technique was acceptable
as a standard method and compared with
the three-pipe formula, the percentage
of success was greater (100% versus 96%).
Also, this method has a lower error rate
than the three-fold method, but the rate
of intubation is three times greater than
that of a three-finger touch. Of course,
considering the low volume of the sample,
studies with a higher sample size seem
to be necessary to investigate the possible
complications and confirm the results
of this study.
Key words: Endotracheal Tube Intubation,
Three-finger Tracheal Palpation, Laryngoscopy
|
Correct placement of the endotracheal tube
is an important part of anesthesia and special
care, but incorrect placement is a common mistake
that can lead to major morbidity and mortality
(1-4). The correct placement occurs when the
distal end of the tube is placed in the middle
of the chip. If the tube is very superficial,
it will lead to its accidental outflow, and
if it is too deep, it will increase the risk
of barotraumas and pneumothorax (3, 4). The
placement of the tubes, especially in children,
is vital and more difficult, because the chip
is shorter in children and more susceptible
to hypoxemia (5).
Conventional instruments used to determine
the proper depth of the chip tube have considerable
limitations (6). Chest radiography is the gold
standard for the proper location of the chip
tube. Bronchoscopy of optic fiber is also useful,
but both are time-consuming, expensive and invasive
and are not always available (1, 2, 4, 7). Other
techniques, such as lung echo, chest movement,
capnography, the observation of the vapor in
the endotracheal tube and the tube placement
based on tube length are calculations that are
used (3, 8-10).
Of these, one of the methods used to correct
placement of chip tube is three-finger tracheal
palpation technique chip tube in the suprasternal
area, which has fewer restrictions, including
the fact that it does not require the equipment,
is cost-effective and available. Various studies
have compared this method with other methods
(10, 11). For example, in a 2014 study by Jonathan
J Gamble et al., which was conducted on 50 children,
it was concluded that using the chip touch technique
to guide the endotracheal tube has excellent
clinical results and the proper depth of the
endotracheal tube relative to formula PALS is
better (12). Accordingly, the aim of the present
study was to examine the accuracy and error
rate of a three-finger tracheal palpation technique
of chip in the suprasternal area and compare
it with the depth determination method using
triple ID formula.
Research method, population and sample
This study is a survey type. The population
of this study was 100 patients aged 2 to 8 years
old who referred to the operating room of the
children’s Hospital for elective surgery
in year 2016. According to the statistical formula
( = 0.5), =20, P0= 0%, P1 =14% and n1 / n2=1).
The sample size was calculated for each group
of 50 patients. These patients had inclusion
criteria (grade 1 patients, ages 2 to 8 years,
patients undergoing elective surgery requiring
general anesthesia and intubation, parental
consent for participation in the plan), and
any patient who had exclusion criteria (abnormal
anatomy of airways, history of active respiratory
infections or colds within 3 weeks), history
of chronic respiratory diseases, asthma and
allergies, lack of parental consent to participate
in the program, patients grade 2 and above)
were excluded.
Data collection method
Data collection form including patient’s
age, patient’s weight, sex, patient group
(group 1: a group in which the triple ID method
was used to determine endotracheal tube depth,
and group 2: the group in which three-finger
tracheal palpation technique is used to determine
the depth of the endotracheal tube), length
of intubation, tube size, tube depth (in the
first group, the number on the side of the lip
based on triple ID formula, and in the second
group, the number on the lips based on the three-finger
tracheal palpation technique of the chip), and
complications (expiratory sounds, exhaustion,
nausea and vomiting, loss of oxygen saturation,
bronchospasm or laryngospasm, coughing and respiratory
failure). Depending on the type of data, data
were recorded by direct observation, hearing,
and use of patient files.
Procedure
Each group consisted of 50 children. Oral medication
with midazolam 0.5 mg / kg of vitamin 5 mg /
kg was used in both groups of children. After
entering the operating room and after the installation
of standard monitoring equipment, pulse oximetry,
ECG, noninvasive blood pressure, anesthetic
induction in the operating room with Sevoflurane
(8%) was done and anesthesia continued in the
gas flow of 2 liters per minute. After adequate
anesthetic depth, venepuncture was performed
with Angiocate No 22 and after the injection
of thiopental sodium 5 mg/kg, the tube placement
was begun. In groups, an anesthetist fixed the
tube using triple ID formula and it was compared
with the auxiliary auscultation of the tube.
Also, the duration of intubation was measured
and recorded. In the second group, an experienced
anesthetist using three-finger tracheal palpation
technique touched endotracheal tube from the
chip, and after the sense of the tube passing
through the supra-district, the tube was fixed.
The tube was then controlled by auscultation
of the chip tube and the duration of the intubation
was measured and recorded. The tube was transmitted
by an experienced anesthetist and was touched
by an anesthetist technician in the supra-standard.
Finally, the accuracy and error rates of the
two methods were compared. The collected data
and probable complications were recorded and
analyzed statistically.
The collected data were analyzed by SPSS software
22 and the significance level of 0.05. In order
to analyze the variables in independent groups
for quantitative data without normal distribution,
Mann- U - Whitney test and for qualitative data,
Chi-square test was used.
In
the
first
group,
out
of
50
patients,
33
(72%)
were
male
and
14
(28%)
were
female,
and
in
the
second
group,
out
of
50
patients,
38
were
male
(76%)
and
12
female
(24%).
The
mean
age
in
the
first
group
(triple
ID
formula)
was
3.88
and
in
the
second
group
(three-finger
tracheal
palpation
technique)
was
4.9.
Also,
the
mean
weight
in
the
first
group
was
16.07
with
a
standard
deviation
of
6.38
and
in
the
second
group
17.77
with
a
standard
deviation
of
5.53.
The
findings
of
Chi-square
and
Mann-Whitney
tests
indicated
no
significant
difference
between
the
two
groups
in
terms
of
age
(p
=
0.64,
Mann-Whitney
U
=
1183),
gender
(p
=
0.41,
=
Pearson
Chi-Square)
and
weight
(p
=
0.38
Mann-Whitney
U
=
1125.50).
A
total
of
100
patients
were
examined.
Two
cases
of
unilateral
chest
echo
(auscultation)
were
observed,
both
of
which
occurred
in
the
first
group,
using
triple
ID
formula
to
determine
the
depth
of
the
endotracheal
tube.
In
the
second
group,
the
pulmonary
auscultation
was
bilateral
in
all
cases
(Table
1).
Chi-square
test
(P
=
0.15,
P
=
0.24
=
Pearson
Chi-Square)
indicates
that
there
is
no
significant
difference
between
the
two
groups
in
terms
of
bilateral
pulmonary
auscultation
(Table
2).
That
is,
it
can
be
said
that
the
two
groups
are
the
same
in
terms
of
bilateral
pulmonary
auscultation
to
control
the
location
of
the
tube.
The
mean
of
tube
depth
in
the
first
group
was
14.79
with
a
standard
deviation
of
1.24
and
in
the
second
group
it
was
94.9
with
a
standard
deviation
of
1.94
(Table
3).
Mann-Whitney
U-
test
(p
=
0.005,
Mann-Whitney
U-431.50,
P=0.00)
showed
a
significant
difference
between
the
two
groups
in
terms
of
tube
depth,
so
that
in
the
first
group
the
depth
of
the
tube
was
higher
than
the
second
group
(Table
4).
The
mean
of
duration
of
intubation
in
the
first
group
was
17.37
with
a
standard
deviation
of
23.3
and
in
the
second
group
it
was
21.82
with
a
standard
deviation
of
3.77
(Table
5).
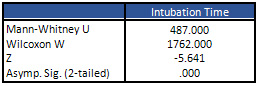
Mann-Whitney
test
(Mann-Whitney
U=487,
p
=
0.00)
indicates
a
significant
difference
between
the
two
groups
in
terms
of
the
duration
of
intubation,
so
that
the
duration
in
the
first
group
is
less
than
that
of
the
second
group
(Table
6
-
page
52).
In
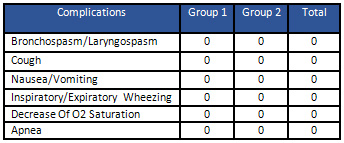
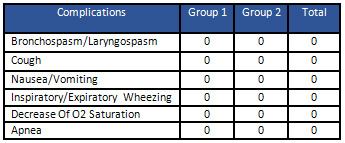
this
study,
complications
such
as
bronchospasm
or
laryngospasm,
coughing,
nausea
and
vomiting,
dementia
or
exhalation
and
respiratory
depression
were
investigated
in
both
groups.
As
shown
in
Table
7,
the
incidence
of
these
complications
did
not
occur
in
the
two
groups
and
the
two
groups
were
the
same
for
the
incidence
of
these
complications.
Table
1:
The
pulmonary
auscultation
indices
between
the
two
groups
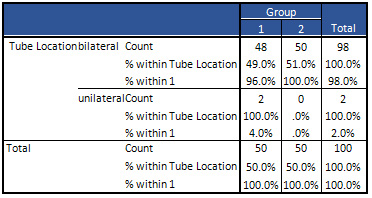
Table
2:
Chi-square
test
between
two
groups
in
terms
of
bilateral
pulmonary
auscultation
a.
2
cells
(50.0%)
have
expected
count
less
than
5.
The
minimum
expected
count
is
1.00.
b.
Computed
only
for
a
2x2
table
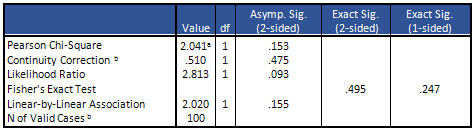
Table
3:
Indices
related
to
mean
of
tube
depth
between
two
groups
Table
4:
Mann-Whitney
test
between
two
groups
in
terms
of
mean
of
tube
depth
Table
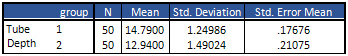
5:
Indices
related
to
the
mean
of
duration
of
intubation
between
the
two
groups
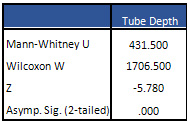
Table
6:
Mann-Whitney
test
between
two
groups
in
terms
of
mean
of
tube
depth
Table
7:
Incidence
of
complications
between
the
two
groups
In
this
study,
which
was
done
in
a
survey
of
methods,
100
patients
were
randomly
divided
into
two
groups
and
were
evaluated.
The
first
group
included
the
use
of
triple
ID
formula
for
determining
the
depth
of
the
tracheal
tube,
and
the
second
group
included
the
use
of
a
three-finger
tracheal
palpation
technique
of
chip
tube
in
the
suprastanchal
touch
site
to
determine
the
depth
of
the
tube.
The
main
objective
of
this
study
was
to
compare
the
appropriate
placement
in
these
two
methods.
For
this,
in
both
groups,
after
the
tubing
(tube
placement),
the
pulmonary
auscultation
was
used
to
confirm
the
correct
placement.
The
findings
showed
that
there
was
no
significant
difference
between
the
two
groups
in
terms
of
age,
gender
and
weight,
and
the
two
groups
were
similar
in
terms
of
these
factors.
Therefore,
it
would
be
possible
to
judge
the
results
of
other
factors
without
considering
these
variables.
The
unwanted
side
effects
that
we
were
expecting
such
as
nausea
and
vomiting,
coughing,
respiratory
failure,
inspiratory
and
expiratory
wheezing,
and
bronchospasm
or
laryngospasm
did
not
differ
significantly
between
the
two
groups
and
the
incidence
of
these
complications
in
either
of
the
two
groups
was
not
observed.
Among
other
important
issues
examined
in
this
study,
was
the
correct
placement
of
the
endotracheal
tube
confirmed
by
the
bilateral
pulmonary
auscultation,
and
as
it
was
observed,
its
success
rate
was
100%
in
the
three-finger
tracheal
palpation
technique
and
in
the
triple
ID
formula
was
96%,
but
in
triple
ID
formula
the
tubing
(tube
placement)
was
more
rapid
than
the
three-finger
touching
group.
In
the
case
of
examining
the
depth
of
the
endotracheal
tube
(the
distance
from
the
lips),
which
was
one
of
the
main
factors
in
this
study,
it
was
also
found
that
the
depth
of
the
three-finger
tracheal
palpation
group
was
clearly
less
than
that
of
the
triple
ID
formula
group.
In
the
studies,
touch
technique
has
been
shown
to
be
superior
to
some
methods.
For
example,
in
the
study
of
Mckay
WP
et
al.,
the
chip
touch
technique
was
compared
with
the
method
of
using
the
patient’s
teeth
to
determine
the
depth
of
the
endotracheal
tube,
which
touch
method
with
a
77%
success
rate
(compared
to
57%),
led
to
proper
placement
(11).
Also,
in
the
study
of
Jenes
Moll
et
al.,
by
comparing
the
two
methods
of
touching
the
cuff
and
the
method
of
using
the
tube
markers,
it
was
concluded
that
in
the
touch
method,
the
tip
of
the
tube
to
the
carina
is
shorter
and
this
distance
is
more
predictable
than
the
method
of
using
markers
(10).
A
study
by
Okoyama
M
et
al.
showed
that
the
cuff
touch
technique
was
a
reliable,
simple,
and
fast
technique
to
ensure
proper
position
of
the
endotracheal
tube
in
children
(13).
As
you
can
see
in
this
study,
the
touch
method
has
a
lower
error
rate
than
the
triple
ID
formula.
In
addition,
in
the
touch
method,
the
depth
of
the
tube
was
less
than
triple
ID
formula.
In
the
studies,
the
auscultation
method
was
also
used
to
ensure
proper
tube
placement,
but
the
chest
radiography
as
a
gold
standard
was
introduced
to
ensure
proper
tube
placement
(tubing)
(1,
2,
4).
For
example,
in
a
study,
Koshy
S
et
al.,
found
that
using
chest
radiography
with
98.5%
success
is
introduced
as
the
preferred
method
for
confirming
the
appropriate
placement
of
the
tracheal
tube
at
the
top
of
the
other
methods.
In
contrast,
Anderson
KH
introduces
the
autistic
method
as
a
routine
method
for
controlling
the
placement
of
an
endotracheal
tube
in
a
review
article
after
introducing
reliable
methods
for
confirmation
of
appropriate
placement
(15).
Finally,
it
should
be
noted
that
among
the
advantages
found
in
this
study
was
the
measurement
of
factors
including
the
length
of
tubing,
the
depth
of
the
tube
and
the
correct
placement
of
the
tube
and
complications
such
as
nausea
and
vomiting,
coughing,
respiratory
failure,
bronchospasm
and
laryngospasm.
In
the
mentioned
studies,
these
factors
were
not
studied
simultaneously.
Therefore,
it
is
suggested
that
this
should
be
considered
in
future
studies
and
perhaps
by
more
accurate
studies,
with
higher
sample
sizes,
we
can
get
more
accurate
results.
Other
suggestions
of
this
study
for
future
research
include
doing
studies
with
higher
sample
size
to
achieve
more
accurate
results,
in
the
age
group
of
less
than
2
years
and
over
8
years,
and
comparing
the
results
with
the
present
study,
comparing
the
three-finger
tracheal
palpation
technique
with
other
methods
and
studies
in
patients
with
non-active
surgery
and
in
patients
with
ASA
class
higher
than
1.
Overall,
this
study
showed
that
the
use
of
the
three-finger
tracheal
palpation
technique
is
acceptable
as
a
standard
method,
and
has
a
higher
success
rate
(100%
versus
96%)
compared
to
the
triple
ID
formula.
Also,
this
method
has
a
lower
error
rate
than
the
triple
ID
formula,
but
the
rate
of
intubation
in
triple
ID
formula
is
more
than
the
three-finger
tracheal
palpation
technique.
Of
course,
to
confirm
these
results,
it
seems
necessary
to
repeat
them
in
studies
with
a
higher
sample
size.
1.
Bekemeyer
WB,
Crapo
RO,
Calhoon
S
et
al.Efficacy
of
chest
radiography
in
a
respiratory
intensive
care
unit.
A
prospective
study.
Chest.
1985
88(5):691-696.
2.
Dronen
S,
Chadwick
O,
Nowak
R.
et
al.
Endotracheal
tip
position
in
the
arrested
patient.
Ann
Emerg
Med.
1982
11(2):116-117.
3.
McCoy
EP,
Russell
WJ,
Webb
RK
et
al.
Accidental
bronchial
intubation.
An
analysis
of
AIMS
incident
reports
from
1988
to
1994
inclusive.
Anaesthesia.
1997
52(1):24-31.
4.
Owen
RL,
Cheney
FW.
Endobronchial
intubation:
a
preventable
complication.
Anesthesiology
1987
67(2):255-257.
5.
Morgan
GA,
Steward
DJ.
Linear
airway
dimensions
in
children:
including
those
from
cleft
palate.
Can
Anaesth
Soc
J.
1982
29(1):1-8.
6.
Marciniak
B,
Fayoux
P,
Hebrard
A
et
al.
Airway
management
in
children:
ultrasonography
assessment
of
tracheal
intubation
in
real
time.
Anesth
Analg
2009
108:461-465.
7.
Schmölzer
GM,
O’Reilly
M,
Davis
PG
et
al.
Confirmation
of
correct
tracheal
tube
placement
in
newborn
infants.
Resuscitation
2013
84(6):731-737.
8.
Betbesé
AJ,
Pérez
M,
Bak
E
et
al.A
prospective
study
of
unplanned
endotracheal
extubation
in
intensive
care
unit
patients.
Crit
Care
Med.
1998
26(7):1180-1186.
9.
Miller
D.
R.
Miller’s
Anesthesia,
eighth
edition,
3.
Elsevier,
Philadelphia,
2015
1670-1671.
10.
Moll
J,
Erb
TO,
Frei
FJ.
Assessment
of
three
placement
techniques
for
individualized
positioning
of
the
tip
of
the
tracheal
tube
in
children
under
the
age
of
4
years.
Paediatr
Anaesth
2015
25:379-385.
11.
McKay
WP,
Klonarakis
J,
Pelivanov
V
et
al.
Tracheal
palpation
to
assess
endotracheal
tube
depth:
an
exploratory
study.
Can
J
Anaesth
2014
61(3):229-234.
12.
Gamble
JJ,
McKay
WP,
Wang
AF
et
al.
Three-finger
tracheal
palpation
to
guide
endotracheal
tube
depth
in
children.
Paediatr
Anaesth
2014
24(10):1050-1055.
13.
Okuyama
M,
Imai
M,
Sugawara
K
et
al.
Finding
appropriate
tube
position
by
the
cuff
palpation
method
in
children.
Masui
1995
44(6):845-848.
14.
Koshy
T,
Misra
S,
Chatterjee
N
et
al.
Accuracy
of
a
Chest
X-Ray-Based
Method
for
Predicting
the
Depth
of
Insertion
of
Endotracheal
Tubes
in
Pediatric
Patients
Undergoing
Cardiac
Surgery.
J
Cardiothorac
Vasc
Anesth
2016
30(4):947-53.
15.
Anderson
KH.
Methods
for
ensuring
correct
tracheal
intubation.
a
review.
Ugeskr
Laeger
1991
153(4):267-269.
|
|
.................................................................................................................

|
| |
|

