|
|
 |
| ............................................................. |
|
|
| ........................................................ |
| From
the Editor |

|
Editorial
A. Abyad (Chief Editor) |
........................................................
|
|
Original contribution/Clinical Investigation
Diabetes
Mellitus - Knowledge, Management and Complications:
Survey report from Faisalabad-Pakistan
Ijaz Anwer, Ahmad Shahzad, Kashmira Nanji, Farah
Haider, Muhammad Masood Ahmad
Alanine
aminotransferase indicates excess weight and
dyslipidemia
Mehmet Rami Helvaci, Orhan Ayyildiz* Mustafa
Cem Algin, Yusuf Aydin, Abdulrazak Abyad, Lesley
Pocock
Comparative Analysis of Antimicrobial Peptides
Gene Expression in Susceptible/Resistant Mice
Macrophages to Leishmania major Infection
Hamid Daneshvar, Iraj Sharifi, Alireza Kyhani,
Amir Tavakoli Kareshk, Arash Asadi
Does
socio-economic status of the patients have effect
on clinical outcomes after coronary artery bypass
grafting surgery?
Forough Razmjooei, Afshin Mansourian, Saeed
Kouhpyma
Comparison
of the uterine artery Doppler indices during
pregnancy between gestational diabetes and diabetes
mellitus and healthy pregnant women
Nazanin Farshchian, Farhad Naleini, Amir Masoud
Jaafarnejhad,
Parisa Bahrami Kamangar
Survey
single dose Gentamicin in treatment of UTI in
children with range of 1 month to 13 years old
in Jahrom during 2015
Ehsan Rahmanian, Farideh Mogharab,
Vahid Mogharab
Evaluation
of control of bleeding by electro cauterization
of bleeding points of amplatz sheath tract after
percutaneous nephrolithotomy (PCNL) in Jahrom
Peymanieh hospital during year 2015-2016
Ali Reza Yousefi , Reza Inaloo
Comparison
of the three-finger tracheal palpation technique
with triple ID formula to determine endotracheal
tube depth in children 2-8 years in 2016-2017
Anahid Maleki, Alireza Ebrahim Soltani, Alireza
Takzare, Ebrahim Espahbodi,
Mehrdad Goodarzi , Roya Noori
Effect
of Sevoflurane and Propofol on pulmonary arterial
pressure during cardiac catheterization in children
with congenital heart diseases
Faranak Behnaz, Mahshid Ghasemi , Gholamreza
Mohseni, Azim Zaraki
Population and Community Studies
Prevalence
and risk factors of obesity in children aged
2-12 years in the Abu Dhabi Islands
Eideh Al-Shehhi, Hessa Al-Dhefairi, Kholoud
Abuasi, Noora Al Ali, Mona Al Tunaiji, Ebtihal
Darwish
Study
and comparison of psychological disorders in
normal students and students with multiple sclerosis
in Shahrekord
Neda Ardestani-Samani, Mohammad Rabiei, Mohammad
Ghasemi-Pirbalooti, Asghar Bayati, Saeid Heidari-Soureshjani
Comparative
study of self-concept, physical self-concept,
and time perspective between the students with
multiple sclerosis and healthy students in Shahrekord
Neda Ardestani-Samani, Mohammad Rabiei, Mohammad
Ghasemi-Pirbalooti, Asghar Bayati, Saeid Heidari-Soureshjani
Relationship
between Coping Styles and Religious Orientation
with Mental Health in the Students of the Nursing-Midwifery
Faculty of Zabol
Nasim Dastras, Mohsen Heidari Mokarrar, Majid
Dastras, Shirzad Arianmehr
Tuberculosis
in Abadan, Iran (2012-2016): An Epidemiological
Study
Ali-Asghar ValiPour, Azimeh Karimyan, Mahmood
Banarimehr, Marzieh Ghassemi, Maryam Robeyhavi,
Rahil Hojjati,
Parvin Gholizadeh
Family
Stability and Conflict of Spiritual Beliefs
and Superstitions among Yazdi People in Iran:
A Qualitative Study
Zahra Pourmovahed , Seyed Saied Mazloomy Mahmoodabad
; Hassan Zareei Mahmoodabadi ; Hossein Tavangar
; Seyed Mojtaba Yassini Ardekani ; Ali Akbar
Vaezi
A
comparative study of the self-actualization
in psychology and Islam
Simin Afrasibi, Zakieh Fattahi
The
effectiveness of cognitive - behavioral therapy
in reducing the post-traumatic stress symptoms
in male students survivors of earthquake in
the central district of Varzeghan
Sakineh Salamat, Dr.Ahad Ahangar, Robab Farajzadeh
Reviews
Effects
and mechanisms of medicinal plants on stress
hormone (cortisol): A systematic review
Kamal Solati, Saeid Heidari-Soureshjani, Lesley
Pocock
Comparing
Traditional and medical treatments for constipation
: A Review Article
Mohammad Yaqub Rajput
A review
of anti-measles and anti-rubella antibodies
in 15- 25 year old women in Jahrom City in 2011
Ehsan Rahmania , Farideh Mogharab, Vahid Mogharab
Review
of percutaneous nephrolithotomy in children
below 12 years old in Jahrom hospital, during
2010-2014
Ali Reza Yousefi , Reza Inaloo
Physical
and mental health in Islam
Bahador Mehraki, Abdollah Gholami
International Health Affairs
The Challenges
of Implementation of Professional Ethics Standards
in Clinical Care from the viewpoint of Nursing
Students and Nurses
Saeedeh Elhami, Kambiz Saberi, Maryam Ban, Sajedeh
Mousaviasl, Nasim Hatefi Moadab, Marzieh Ghassemi
Cognitive
Determinants of Physical Activity Intention among
Iranian Nurses: An Application of Integrative
Model of Behavior Prediction
Arsalan Ghaderi, Firoozeh Mostafavi, Behzad Mahaki,
Abdorrahim Afkhamzadeh,
Yadolah Zarezadeh , Erfan Sadeghi
Effect
of resilience-based intervention on occupational
stress among nurses
Hossein Jafarizadeh, Ebrahim Zhiyani, Nader
Aghakhani, Vahid Alinejad, Yaser Moradi
Education and Training
Calculation
of Salaries and Benefits of Faculty Members
in the Ministry of Health and Medical Education
of Iran
Abdolreza Gilavand
The
effect of education on self-care behaviors of
gastrointestinal side effects on patients undergoing
chemotherapy
Shokoh Varaei, Ehsan Abadi Pishe, Shadan Pedram
Razie, Lila Nezam Abadi Farahani
Creating
and Validating the Faith Inventory for Students
at Islamic Azad University of Ahvaz
Solmaz Choheili, Reza Pasha, Gholam Hossein
Maktabi, Ehsan Moheb
Creating
and Validating the Adjustment Inventory for
the Students of Islamic Azad University of Ahvaz
Homa Choheili, Reza Pasha, Gholam Hossein Maktabi,
Ehsan Moheb
Evaluating
the Quality of Educational Services from the
Viewpoints of Radiology Students of Ahvaz Jundishapur
University of Medical Sciences
Abdolreza Gilavand, Jafar Fatahiasl
An
Investigation of Psychosocial aspect of Iranian
Nursing Students' Clinical Setting
Mahsa Boozaripour , Zanyar Karimi, Sima Zohari
Anbohi, Amir Almasi-Hashiani, Fariba Borhani
Clinical Research and Methods
Comparison
of the Antibacterial Effects of Chlorhexidine
Mouth washes with Jaftex Mouth wash on Some
Common Oral Microorganisms (An in Vitro Study)
Ebrahim Babadi, Zahra Bamzadeh, Fatemeh Babadi
Study
of the effect of plasma jet on Fusarium isolates
with ability to produce DON toxins
Elham Galin Abbasian, Mansour Bayat, Arash chaichi
Nosrati, Seyed Jamal Hashemi, Mahmood Ghoranneviss
The
comparison of anti-inflammatory effect in two
methods of topical dexamethasone injection and
topical application of ginger alcoholic extract
after removing mandibular wisdom teeth
Sahar Zandi, Seyyed Muhammadreza Alavi, Kamran
Mirzaie, Ramin Seyedian, Narges Aria, Saman
Jokar
The effect
of curcumin on growth and adherence of major
microorganisms causing tooth decay
Leila Helalat, Ahmad Zarejavid, Alireza Ekrami,
Mohammd Hosein Haghighizadeh, Mehdi Shiri Nasab
|
|
Chief
Editor -
Abdulrazak
Abyad
MD, MPH, MBA, AGSF, AFCHSE
.........................................................
Editorial
Office -
Abyad Medical Center & Middle East Longevity
Institute
Azmi Street, Abdo Center,
PO BOX 618
Tripoli, Lebanon
Phone: (961) 6-443684
Fax: (961) 6-443685
Email:
aabyad@cyberia.net.lb
.........................................................
Publisher
-
Lesley
Pocock
medi+WORLD International
11 Colston Avenue,
Sherbrooke 3789
AUSTRALIA
Phone: +61 (3) 9005 9847
Fax: +61 (3) 9012 5857
Email:
lesleypocock@mediworld.com.au
.........................................................
Editorial
Enquiries -
abyad@cyberia.net.lb
.........................................................
Advertising
Enquiries -
lesleypocock@mediworld.com.au
.........................................................
While all
efforts have been made to ensure the accuracy
of the information in this journal, opinions
expressed are those of the authors and do not
necessarily reflect the views of The Publishers,
Editor or the Editorial Board. The publishers,
Editor and Editorial Board cannot be held responsible
for errors or any consequences arising from
the use of information contained in this journal;
or the views and opinions expressed. Publication
of any advertisements does not constitute any
endorsement by the Publishers and Editors of
the product advertised.
The contents
of this journal are copyright. Apart from any
fair dealing for purposes of private study,
research, criticism or review, as permitted
under the Australian Copyright Act, no part
of this program may be reproduced without the
permission of the publisher.
|
|
|
| November 2017
- Volume 15, Issue 9 |
|
|
Does socio-economic status
of patients have an effect on clinical outcomes
after coronary artery bypass grafting surgery
Forough Razmjooei (1)
Afshin Mansourian (2)
Saeed Kouhpyma (3)
(1) Department of General Surgery, Shiraz University
of Medical Sciences, Shiraz, Iran
(2) Department of Anesthesiology, Yasuj University
of Medical Sciences, Yasuj, Iran
(3) Department of cardiovascular surgery, Shiraz
University of Medical Sciences, Shiraz, Iran
Corresponding author:
Afshin Mansourian,
Department of Anesthesiology,
Yasuj University of Medical Sciences, Iran,
Email: Afshin.mansourian@yahoo.com
|
Abstract
Background:
Socioeconomic status (SES) is defined
as an individual’s social and financial
position in comparison with that of
other people. Cardiovascular disease is
more common in people with low SES. This
inverse relation between SES and Cardiovascular
disease risk in countries with high-income
is associated with some of the behavior
and psychology status in people with low
SES, such as smoking, malnutrition, and
stresses.
Objectives:
The purpose of our study was to evaluate
the effect of patient’s socioeconomic
status on clinical outcomes in CABG surgery.
Patients and
Methods: Since March 2014 to August
2015, 201 of 412 patients undergoing CABG
surgery had operations in private hospitals
who were categorized as patients with
good socioeconomic status because of their
financial position, life situation, and
the ability to afford a high price for
their operation. And 211 patients who
had operation in university hospitals
were named low socioeconomic status. Data
were compared using Kolmogorov-Smirnov,
Chi-square, Student T test and Mann-Whitney
U test, regarding structural differences
between groups. To determine factors influencing
Post-operative outcomes, methods of logistic
regression were used.
Results:
At the end of the study, The 30-day mortality
(p: 0.11), hospital mortality (p: 0.16),
dialysis need (p: 0.09), neurologic events
(CVA, LOC, Seizure) (p: 0.36), post-operative
arrhythmia (AF, PVC, PAC and other) (p:
0.81) of patients with good socioeconomic
status were not significantly different
from the patients having low socioeconomic
status. Hospital stay (p<0.01), wound
infection (p: 0.004), first day bleeding
(p:<0.0001), second day bleeding (p:<0.001),
third day bleeding (p:<0.001), Reoperation
need (p: 0.02) blood transfusion in first
day after surgery (p < 0.01), second
day after surgery (p < 0.0001), and
third day after surgery (p<0.001) were
significantly different in patients having
good socioeconomic status and patients
with low socioeconomic status.
Conclusions:
In our study, socioeconomic status had
a significant effect on: Hospital stay,
wound infection, first, second and third
day bleeding after surgery, Reoperation
need, blood transfusion in first, second
and third day after surgery. But it had
no effect on 30-day mortality and hospital
mortality, dialysis need, neurologic events
and post-operative arrhythmia.
Key words:
CABG surgery, cardiopulmonary bypass,
clinical outcomes, socioeconomic status
|
Socioeconomic status (SES) refers to various
aspects of social stratification and situation,
such as income, education, social class and
occupation. These aspects are somehow correlated
with each other but often used interchangeably
[1]. The cardiovascular disease (CVD) risk in
both genders is more common in patients with
low SES than patients with higher SES. This
inverse relation between SES and Cardiovascular
disease risk in rich-countries has interrelation
with some behaviors and psychology status in
people with low SES, such as smoking, malnutrition
and stresses. [2] Socioeconomic status (SES)
also has an effect on prognosis and survival
from disease, because it can provide special
conditions for patients. For many years this
relationship between social class and getting
better in the functional status of the heart,
after myocardial infarction has been reported
[3]. Various socio-economic factors can effect
on dietary status which influences anemia and
maybe it is a contributing cause in patients
[4]. In patients undergoing surgery, poor nutrition
significantly affects outcomes, and patients
with poor nutrition have poor outcomes after
surgery [5]. Seltzer after assessment of 500
medical-surgical patients found there is a fourfold
association between increasing complications
and a six fold increasing in mortality in patients
who have serum albumin level less than 35 g/L
[6]. Immune status and nutritional condition
are associated factors that could effect on
surgical outcomes in the patients [7]. Nutrition
can also affect mortality rate by (50%) in malnourished
old patients and (11%) in well-nourished old
patients [8]. In patients with stroke, low pre-stroke
SES had significant interrelation with post
stroke outcomes such as: 3-months mortality,
disability and dependence [9].
Because of the differences in clinical outcomes
in our two groups, socioeconomic status of patients
is important. So we designed this study to investigate
the role of economy on post-operative outcomes
in patients with CABG surgery.
In an attempt to clarify effect of socioeconomic
status on clinical outcomes in patients with
CABG surgery, we retrospectively analyzed the
surgical database of three institutions since
March 2014 to August 2015. 412 patients who
had conditions to include in our study, with
a similar surgery team (common surgeon and perfusionist)
were divided into two groups. The first 201
patients who had their operation in a private
hospital and who had higher socioeconomic status
were our first group. The second group were
categorized as having low socioeconomic status
were 211 other patients who had their operation
done in university hospitals. Patients in private
hospitals were capable of affording a high charge
for their operation and in university hospital
there was no charge. For safety of this study
local authority’s approval was received.
Clinical outcomes which we aimed to compare
in our two groups were defined as; hospital
length of stay, hospital death, wound infection,
dialysis need, neurologic events, re -exploration
need, bleeding volume in ICU, arrhythmia (AF,
PVC, PAC) during hospitalization, blood volumes
transfusion during first three day after operation
in ICU and 30-day mortality. For ensuring equality
in the two groups we excluded patients with:
renal insufficiency (Cr>1.5), liver dysfunction
(SGPT& SGOT>twofold more than normal),
heart insufficiency (EF<30%), patients with
previous neurologic events, immune deficiency
(WBC<2500), anti-coagulopathy (platelet<100000),
preoperative infection (WBC>10000), autoimmune
disorders, REDO operations, patients with specific
behavior from the study. Pre-operative variables
are shown in (Table 1). Significant statistical
difference was defined as p values smaller than
0.05. There were several significant statistical
differences in pre-operative and intra-operative
variables between patients with higher socioeconomic
status (private hospital) and patients with
low socioeconomic status (university hospitals)
when we use the Mann-Whitney estimator to determine
group differences (Table 1 and Table 2). Myocardial
revascularization by surgeons in all patients
was done through median sternotomy. For anticoagulation
throughout surgery a heparin dose was administered
to keep activated coagulation time greater than
400 s. Protamine dose 1:1 was selected to antagonize
heparin effect. In both groups, all patients’
(100%) operation was done with on pump surgery
and using extracorporeal circulation with mild
hypothermia (32° to 34°C). Ascending
aorta and venous two-stage cannulation were
used for bypassing and tepid crystalloid cardioplegia
(22-24°C) in two group was administered
to paralyise the heart. Generally, hematocrits
below 22 (Hb<7) on extracorporeal circulation
and Hb<10 after surgery in ICU was avoided,
and aggressively treated by blood transfusion
if it occurred. Internal mammary artery use
was high in the two groups (83.9% in private
hospital and 76% in university hospitals).
Patients
having
low
socioeconomic
status,
had
some
risk
profile
before
surgery
(Table
1)
such
as:
lesser
BSA,
height
and
weight,
higher
urgent
or
emergent
surgery
required
and
acute
myocardial
infarction
in
comparison
with
higher
socioeconomic
status
patients.
Although
they
were
better
in
some
other
risk
factors
before
surgery
such
as:
number
of
grafts,
Medical
history,
DM,
HLP
and
Smoking.
Analyzing
the
pre-operative
laboratory
data
between
the
two
groups
showed
that
patients
with
higher
Socioeconomic
status
had
more
kidney
and
liver
problems
(SGPT,
SGOT,
BUN
and
Cr
were
higher)
and
higher
hemoglobin
levels
(patients
with
low
SES
(53.4%)
tend
to
be
more
anemic
(p<0.0001)
than
patients
with
higher
SES
(35.3%)),
and
platelet
count
was
higher
too.
Hypertension
was
the
most
frequent
post
medical
history
disease
in
both
groups
with
no
difference
in
prevalence
comparison
(p=
0.13)
(Table
2).
During
the
CPB
and
surgery
we
had
some
differences
between
the
two
groups,
such
as:
use
of
internal
mammary
artery
(76%)
in
higher
SES
group
and
(83.9%)
in
low
SES
group.
Also
lowest
hemoglobin
during
CPB
was
lower
(p<0.001)
in
higher
SES
group
patients.
Blood
transfusion
(246.5±228
vs.
109.5±151
and
p<0.0001),
Aortic
clamp
time
(p<0.007)
and
pumping
time
(p<0.01)
were
lower
in
the
higher
SES
group
in
comparison
with
the
low
SES
group.
But
surgery
time
(p<0.001),
lowest
temperature
(p<0.001),
urine
output
(p<0.0001)
and
hemofiltration
(p<0.001)
were
higher
in
the
higher
SES
group
(Table
3).
Analyzing
the
post-operative
clinical
outcomes
between
the
two
groups
showed
that:
Hospital
mortality
(p:
0.16),
Dialysis
need
(p:
0.09),
Neurologic
events
(p:
0.36),
CVA
(p:
0.13),
LOC
(p:
0.28),
Seizure
(p:
0.32),
30-day
mortality
(p:
0.11),
total
Arrhythmias
(p:
0.81)
and
post-operative
PAC
(p:
0.19)
were
not
significantly
different
in
the
higher
SES
and
low
SES
groups.
But
Hospital
stay
(4.1
±0.73
vs.
5.03
±
2.7,
p<0.01),
wound
infection
(p<0.004),
first-day
bleeding
after
surgery
(p<0.0001),
third-day
bleeding
(p<0.001),
first-day
blood
transfusion
(p<0.01),
third-day
blood
transfusion
(p<0.001),
Reoperation
need
(p:
0.02),
post-operative
AF
(p:
0.05)
and
PVC
(p:
0.03),
were
significantly
lower
in
the
higher
SES
group
patients
in
comparison
with
the
low
SES
group.
But
bleeding
volume
(p<0.001)
and
blood
transfusion
volume
(p<0.0001)
during
second
day
after
surgery
were
significantly
higher
in
the
higher
SES
group
patients
(Table
4).
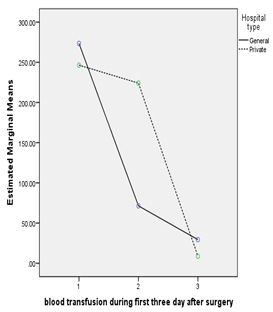
Figure
1
shows
blood
transfusion
volume
during
the
third
day
after
surgery.
Table
1.
Demographic
Data
before
Surgery
*Mean±
Standard
Deviation
Abbreviation:
BSA,
body
surface
area;
EF,
ejection
fraction;
MI,
myocardial
infarction;
DM,
diabetes
mellitus;
HTN,
hypertension;
HLP,
hyper
lypidemia;
COPD,
chronic
obstructive
pulmonary
disease
Table
2.
Laboratory
Data
before
Surgery
*Mean±
Standard
Deviation
Abbreviation:
WBC,
white
blood
cell;
BUN,
blood
urea
nitrogen;
CR,
creatinine;
SGPT,
serum
glutamate-pyruvate
transaminase;
SGOT,
serum
glutamic
oxaloacetic
transaminase.
Table
3:
Intra
operative
information
*Mean±
Standard
Deviation
Abbreviation:
LIMA,
left
internal
mammary
artery;
HB,
hemoglobin
Table
4:
Post-operative
clinical
outcomes
Analysis
in
the
two
groups
Figure
1:
blood
transfusion
volume
during
the
first
three
days
after
surgery
Footnote:
Some
patients
don’t
like
to
be
infused
by
other
people’s
blood
in
any
situation
because
of
their
religions.
The
effect
of
patients’
socio-economic
status
(SES)
on
nutrition
and
health
is
important.
SES
is
interrelated
with
the
health
base
on
lifestyles
which
is
the
circumstances
of
cardiovascular
disease.
It
means
that
low
SES
is
associated
with
some
risky
behaviors
like
smoking
or
less
physical
activity
and
poor
dietary
adaption
in
patients
which
makes
them
feel
hopeless
and
depressed
[11].
Yu,
Zhijie,
et
al
found
the
reverse
relationship
between
SES
and
cardiovascular
disease
risk
factor
[12].
Lynch,
et
al.
showed
the
developmental,
behavioral
and
psychological
effect
of
SES
in
the
childhood
period
in
that
it
was
reinforced
and
maintained
during
the
life
time[13].
Because
we
didn’t
have
similar
research
in
this
area,
there
was
an
uncertain
gap
between
our
knowledge
and
this
influence
on
outcomes.
For
this
study
we
used
survey
data
in
two
university
hospitals
and
one
private
hospital
to
examine
the
degree
of
patient
socio-economic
status
effect
on
post-operative
result
in
patients
undergoing
coronary
artery
bypass
grafting
surgery.
Clinical
outcomes
were
defined
as:
hospital
stay,
hospital
mortality,
dialysis
need,
wound
infection,
blood
transfusion,
bleeding,
30
day
mortality,
re-exploration
need,
neurologic
events
and
arrhythmia
that
was
gathered
from
a
cluster
of
the
patients
and
phone
calls
to
the
patients
or
their
visitors
and
compared
with
each
other
to
clarify
this
effect.
Our
result
showed
that
preoperative
socio-economic
status
of
the
patients
who
had
CABG
surgery
affected
clinical
outcomes
in
many
aspects.
Similar
to
our
result,
some
studies
have
concluded
that
socioeconomic
status
and
operative
status
has
been
associated
with
outcomes
[14-16].
Yu,
Tsung-Hsien
et
al,
reached
the
result
that
poorer
quality
of
services
were
associated
with
worse
outcomes
in
patients
with
low-income
who
had
CABG
surgery.
In
fact
there
was
less
tendency
in
individuals
with
low
income
toward
high-quality
healthcare
despite
Health
Insurance
programs
an
this
was
the
cause
of
worse
clinical
outcome
after
surgery
[17].
But
in
some
other
aspects
there
were
no
differences.
Some
studies
had
been
done
on
a
few
aspects
of
our
study.
Results
in
our
study
did
not
show
any
significant
difference
between
hospital
mortality
and
30-day
mortality
after
surgery
between
low
SES
and
higher
SES
patients
(p>0.05).
Unlike
our
study
Dzayee,
et
al
showed
in
their
cohort
study
that
Mortality
Rate
after
CABG
surgery
in
patients
with
lower
socioeconomic
position
was
higher
during
their
study
period[18].
Also
Yong,
et
al.
found
that
with
increase
in
patients’
income,
mortality
rate
was
decreased
slightly
(10.8%
mortality
in
patients
with
lowest
income
versus
9.4%
in
highest-income
patients).
Re-admission
after
thirty
days
in
higher
socioeconomic
status
patients
were
higher
(9.9%
in
lower-income
patients
versus
10.4%
in
higher-income)
[19].
And
Abbasi,
et
al’s
result
showed
that
Hospital
mortality
in
patients
with
low
socioeconomic
status
was
higher
in
comparison
with
high
socioeconomic
status
patients
due
to
the
acute
coronary
syndrome
[20].
But
similar
to
our
study
Shi,
William
Y,
et
al.
found
that
patients
from
remote
areas
undergoing
CABG
surgery
experienced
poorer
long-term
survival.
But
thirty-day
mortality
was
not
different
in
the
different
groups
(1.6%
vs.
1.6%,
p>0.99)
[21].
We
found
that
Hospital
length
of
stay
has
been
affected
by
patients
SES
((4.1
±0.73
vs.
5.03
±
2.7,
p<0.01).
As
in
our
conclusion
Poole,
et
al.
showed
in
their
study
that
Hospital
Length
of
stay
after
CABG
in
patients
with
depression
had
a
relationship
with
socioeconomic
status
[22].
SES
also
has
an
important
role
in
access
to
cardiac
care
services
and
significant
effects
on
one-year
mortality
after
MI
[23].
We
concluded
that
patients
SES
had
a
significant
role
in
choosing
hospital
type
(private
hospital
or
university
hospitals),
and
pre-operative
health
status
such
as:
BSA,
Weight
and
height,
acute
MI,
emergency
operation,
hemoglobin
level
(anemia),
platelet
count,
and
Cr
level
and
also
had
significant
effect
on
need
for
blood
products
during
surgery,
length
of
hospital
stay,
wound
infection,
re-exploration
need
for
bleeding,
bleeding
volume
and
blood
transfusion
volume
after
surgery
in
patients
who
had
CABG
surgery.
But
it
had
no
effect
on
hospital
and
30-day
mortality,
dialysis
need,
neurologic
events
and
arrhythmia.
Acknowledgments;
this
paper
is
a
part
of
research
towards
an
MSc
degree
at
School
of
Medicine,
Shiraz
University
of
medical
sciences.
There
was
no
conflict
of
interest.
We
would
like
to
thank
the
department
of
anesthesiology,
general
and
cardiovascular
surgery
and
also
perfusion
department
at
Shiraz
University
of
medical
sciences
for
helping
us
in
collecting
the
data.
1.
Ostrove,
J.M.
and
N.E.
Adler,
The
relationship
of
socio-economic
status,
labor
force
participation,
and
health
among
men
and
women.
Journal
of
Health
Psychology,
1998.
3(4):
p.
451-463.
2.
Clark,
A.M.,
et
al.,
Socioeconomic
status
and
cardiovascular
disease:
risks
and
implications
for
care.
Nature
Reviews
Cardiology,
2009.
6(11):
p.
712-722.
3.
Ickovics,
J.R.,
C.M.
Viscoli,
and
R.I.
Horwitz,
Functional
recovery
after
myocardial
infarction
in
men:
the
independent
effects
of
social
class.
Annals
of
Internal
Medicine,
1997.
127(7):
p.
518-525.
4.
Ahmed,
F.,
et
al.,
Anaemia
and
vitamin
A
deficiency
in
poor
urban
pregnant
women
of
Bangladesh.
Asia
Pacific
journal
of
clinical
nutrition,
2003.
12(4):
p.
460-466.
5.
Dempsey,
D.,
J.
Mullen,
and
G.
Buzby,
The
link
between
nutritional
status
and
clinical
outcome:
can
nutritional
intervention
modify
it?
The
American
journal
of
clinical
nutrition,
1988.
47(2):
p.
352-356.
6.
Seltzer,
M.H.,
et
al.,
Instant
nutritional
assessment.
Journal
of
Parenteral
and
Enteral
Nutrition,
1979.
3(3):
p.
157-159.
7.
Buzby,
G.P.,
et
al.,
Prognostic
nutritional
index
in
gastrointestinal
surgery.
The
American
Journal
of
Surgery,
1980.
139(1):
p.
160-167.
8.
Linn,
B.S.,
D.S.
Robinson,
and
N.G.
Klimas,
Effects
of
age
and
nutritional
status
on
surgical
outcomes
in
head
and
neck
cancer.
Annals
of
surgery,
1988.
207(3):
p.
267.
9.
Bettger,
J.P.,
et
al.,
The
association
between
socioeconomic
status
and
disability
after
stroke:
Findings
from
the
Adherence
eValuation
After
Ischemic
stroke
Longitudinal
(AVAIL)
registry.
BMC
public
health,
2014.
14(1):
p.
281.
10.
Dragano,
N.,
et
al.,
Neighbourhood
socioeconomic
status
and
cardiovascular
risk
factors:
a
multilevel
analysis
of
nine
cities
in
the
Czech
Republic
and
Germany.
BMC
public
health,
2007.
7(1):
p.
255.
11.
Lynch,
J.,
et
al.,
Socioeconomic
Status
and
progression
of
carotid
atherosclerosis
prospective
evidence
from
the
kuopio
ischemic
heart
disease
risk
factor
study.
Arteriosclerosis,
thrombosis,
and
vascular
biology,
1997.
17(3):
p.
513-519.
12.
Yu,
Z.,
et
al.,
Associations
between
socioeconomic
status
and
cardiovascular
risk
factors
in
an
urban
population
in
China.
Bulletin
of
the
World
Health
Organization,
2000.
78(11):
p.
1296-1305.
13.
Lynch,
J.W.,
et
al.
Do
cardiovascular
risk
factors
explain
the
relation
between
socioeconomic
status,
risk
of
all-cause
mortality,
cardiovascular
mortality,
and
acute
myocardial
infarction?
American
journal
of
epidemiology,
1996.
144(10):
p.
934-942.
14.
Bradshaw,
P.J.,
et
al.,
Outcomes
after
first
percutaneous
coronary
intervention
for
acute
myocardial
infarction
according
to
patient
funding
source.
BMC
health
services
research,
2014.
14(1):
p.
405.
15.
Efird,
J.T.,
et
al.
Operative
status
and
survival
after
coronary
artery
bypass
grafting.
in
Heart
Surg
Forum.
2014.
16.
Tang,
X.,
et
al.,
Neighborhood
socioeconomic
status
and
the
prevalence
of
stroke
and
coronary
heart
disease
in
rural
China:
A
populationbased
study.
International
Journal
of
Stroke,
2015.
10(3):
p.
388-395.
17.
Yu,
T.-H.,
Y.-C.
Hou,
and
K.-P.
Chung,
Do
low-income
coronary
artery
bypass
surgery
patients
have
equal
opportunity
to
access
excellent
quality
of
care
and
enjoy
good
outcome
in
Taiwan?
International
journal
for
equity
in
health,
2014.
13(1):
p.
64.
18.
Dzayee,
D.A.M.,
et
al.,
Short
and
Long
Term
Mortality
after
Coronary
Artery
Bypass
Grafting
(CABG)
Is
Influenced
by
Socioeconomic
Position
but
Not
by
Migration
Status
in
Sweden,
1995–2007.
PloS
one,
2013.
8(5):
p.
e63877.
19.
Yong,
C.M.,
et
al.,
Socioeconomic
Inequalities
in
Quality
of
Care
and
Outcomes
Among
Patients
With
Acute
Coronary
Syndrome
in
the
Modern
Era
of
Drug
Eluting
Stents.
Journal
of
the
American
Heart
Association,
2014.
3(6):
p.
e001029.
20.
Abbasi,
S.H.,
et
al.,
Socioeconomic
status
and
in-hospital
mortality
of
acute
coronary
syndrome:
Can
education
and
occupation
serve
as
preventive
measures?
International
journal
of
preventive
medicine,
2015.
6.
21.
Shi,
W.Y.,
et
al.,
Impact
of
socioeconomic
status
and
rurality
on
early
outcomes
and
mid-term
survival
after
CABG:
insights
from
a
multicentre
registry.
Heart,
Lung
and
Circulation,
2014.
23(8):
p.
726-736.
22.
Poole,
L.,
et
al.,
The
combined
association
of
depression
and
socioeconomic
status
with
length
of
post-operative
hospital
stay
following
coronary
artery
bypass
graft
surgery:
Data
from
a
prospective
cohort
study.
Journal
of
psychosomatic
research,
2014.
76(1):
p.
34-40.
23.
Alter,
D.A.,
et
al.,
Effects
of
socioeconomic
status
on
access
to
invasive
cardiac
procedures
and
on
mortality
after
acute
myocardial
infarction.
New
England
Journal
of
Medicine,
1999.
341(18):
p.
1359-1367.
|
|
.................................................................................................................

|
| |
|

