|
Effect of Sevoflurane
and Propofol on pulmonary arterial pressure
during cardiac catheterization in children with
congenital heart diseases
Faranak Behnaz (1)
Mahshid Ghasemi (2)
Gholamreza Mohseni (3)
Azim Zaraki (4)
(1) Assistant
Professor of Anesthesiology, Shohada hospital,
Shahid Beheshti University, Tehran, Iran
(2) Assistant Professor of Anesthesiology, Shahid
Beheshti University of medical sciences, Tehran,
Iran
(3) Associate Professor of Anesthesiology, Shohada
Hospital, Shahid Beheshti Medical science University,
Tehran, Iran
(4) Resident of Anesthesiology, Modarres hospital,
Shahid Beheshti Medical Science University,
Tehran, Iran
Corresponding author:
Gholamreza
Mohseni
Associate professor of anesthesiology,
Shohada Hospital,
Shahid Beheshti Medical Science University,
Tehran, Iran
Email:
mohsen85ir@yahoo.com
|
Abstract
Background:
The aim of this study was to investigate
the effect of sevoflurane and propofol
on pulmonary arterial pressure during
cardiac catheterization in children with
congenital heart diseases.
Methods:
In order to reach the research goals,
80 patients with congenital heart disease
who had referred to Modarres Hospital,
Iran for cardiac catheterization were
selected as sample. They were divided
into two groups for treatment with propofol
or sevoflurane. In children in the sevoflurane
group, anesthesia began initially with
higher concentrations of sevoflurane (4-6%)
and spontaneous respiration by face mask
with suitable size and gradually the concentration
of gas was reduced by increasing the anesthetic
depth and anesthesia was continued with
1 MAC inhaled Sevoflurane based on age
and individual characteristics of each
patient and spontaneous respiration. In
the other group, propofol drug (50-70
g/ kg/min) was injected by perfusion pump.
Cardiac catheterization was performed
by injection of lidocaine into the catheter
entrance i.e. the femoral vessel when
the anesthetic depth reached to Ramsay
Sedation Score = 3 and BIS = 65-85. Meanwhile,
in the groups of sevoflurane and Propofol,
systolic and diastolic blood pressurein
pulmonary patients was recorded before
andduring catheterization. T-test was
used to analyze the data.Results: The
findings showed that there was no significant
reduction in systolic and diastolic pulmonary
arterial pressure in the sevoflurane group
in the pretest or posttest, while in the
propofol group, systolic and diastolic
blood pressure were significantly reduced
in the pulmonary artery.
Conclusion:
According to the results, it can be
concluded that Propofol is considered
more appropriate than Sevoflurane for
cardiac catheterization in children with
congenital heart disease and anesthesiologists
can use Propofol as a suitable alternative
for sevoflurane.
Key words:
Congenital heart disease, Anesthesia,
Pulmonary artery pressure, Clinical symptoms
|
One of the most common congenital diseases
of children is abortion of the heart. Among
the congenital anomalies in infants, the cardiovascular
system causes most deaths. The incidence of
congenital heart disease is approximately 8%
in 1,000 live births, and if one of the first-degree
relatives is afflicted with CHD, the incidence
reaches 2-6% (Bernstein, 2,000). Pulmonary artery
pressure (PHT) occurs in many congenital heart
diseases, and the status of the pulmonary vascular
system is often the key to clinical manifestations,
period of illness, and curative treatment with
surgical methods (Barst, 2001; Qureshi, 2002).
By definition, the increase of 25 mm Hg in average
pulmonary arterial pressure at rest time and
more than 30 mm Hg during activity is said to
be pulmonary arterial pressure, whether it is
due to increased blood flow or increased vascular
resistance (Barst, 2001). The increase in pulmonary
vascular resistance leads to double-sided or
right-to-left shunting through a congenital
communication defect that occurs between the
systemic and pulmonary blood stream, which is
defined as the Isenmenger syndrome, which is
proven by cardiac catheterization (Bernstein,
2000). Patients with PHT may be resistant to
medical treatment and ultimately progress to
cardiac dysfunction and death, so assessing
the severity of illness and the ability to predict
the likelihood of death is an important factor
in decision-making in these patients.
The goal of sedation during cardiac catheterization
in sick children is immobilization, numbness
and stability in the respiratory and cardiac
system (Lebovic et al., 1992). Induction of
anesthesia, intubation and respiration through
the device during cardiac catheterization may
result in severe changes in respiratory and
cardiac indices. For this reason, the use of
relaxation method for cardiac catheterization
while conscious is preferable to the general
anesthetic method. The anesthesiologist plays
an important role in this regard (Reich et al.,
1989). Regarding the inhalation anesthetics,
although halothane was thought to be a mild
inhaler inducing good intubation for many years,
however, since the introduction of sevoflurane
in the early 90’s, sevoflurane has been
widely used instead of halothane (Jellish Et
al., 2005). Now, this question is discussed
as to whether sevoflurane can create conditions
for an effective and rapid intubation such as
thiopental and succinylcholine alone. There
are many studies suggesting the successful use
of sevoflurane in the intubation condition (Woods,
2005).
Thwaites et al. (1999) showed that sevoflurane
can be a satisfactory alternative to the standard
method of Succinylcholine chloride and Propofol
when children are under non-emergency conditions.
Still, studies in this area seem to be inadequate
(Woods, 2005).
Propofol is a relatively new intravenous anesthetic.
This drug is very useful for calming, relaxation,
and at higher doses, it is a great general anaesthetic.
Propofol is a sleeping drug with an unknown
mechanism and is responsible for impaired cardiovascular
and is respiratory system dependent on dose.
It also has direct antinociceptive effect, and
does not have analgesic effects like benzodiazepines
(Greff, 1999).
Propofol is used to make calm and conscientious
sleepiness to induce and to maintain conscious
calmness. The pharmacokinetics of this drug
have made it an effective agent for Conscious
calmness (Liberman et al., 1985). Its mechanism
of action is to increase gamma aminobutyric
acid, activating chlorine canals as a result
of the activity of inhibitory neurons in the
hippocampus. In addition, it prevents the release
of acetylcholine in the hippocampus and prefrontal
cortex.
The main benefits of this drug include the
onset of fast effects, the lack of active metabolites,
and rapid liver cleansing after intravenous
injection (Patterson et al., 1991). This medication
in elderly patients may be associated with a
reduction in high blood pressure and, consequently,
a decrease in tissue hemorrhage and oxygenation
(Kirkpatrick et al., 1988). Other studies have
reported hemodynamic impairment of Propofol
injection in children (Short, 1991). The reduction
in hypoproteinemia caused by Propofol injection
in children at the onset of anesthesia may be
between 28- 31% (Goh et al., 2005), and the
reduction in blood pressure induced by Propofol
injection in cardiovascular patients may be
very severe (Patrick et al., 1985).
In a study, the effects of anesthesia with
ketamine and Propofol in children with congenital
heart disease were investigated for cardiac
catheterization (Zeynep Tosun et al., 2006).
In this study, the amount of intraoperative
movement in the second group receiving less
ketamine was slightly higher than the first
group, but this difference was not statistically
significant, while the duration of waking patients
in the same group was shorter with a lower dose
of ketamine. In other items, the hemodynamic
changes, respiratory conditions, and arterial
blood gas were the same in both groups. The
researchers concluded that a combination of
both doses of ketamine and Propofol for cardiac
catheterization was effective in these children,
although children who received more ketamine
were statistically significantly later awake
and conscious, but this was acceptable to the
researchers.
In another study, the effects of Propofol and
ketamine were investigated on systemic blood
and pulmonary flow in children undergoing cardiac
catheterization. In this study, patients were
divided into three groups without intra-cardiac
shunt, with left to right shunt and right to
left shunt. The findings showed that in all
patients, all of the three groups who were under
continuous infusion of Propofol had a significant
decrease in the mean systemic arterial pressure.
In two groups of patients who had cardiac shunt,
Propofol infusion resulted in a clear reduction
of systemic vascular resistance and a significant
increase in systemic blood flow, while the resistance
of pulmonary vessels and blood flow did not
change significantly.
These changes significantly and statistically
reduced the ratio of pulmonary blood flow to
the systemic, resulting in a decrease of left-to-right
shunt and an increase of right-to-left shunt.
After infusion of ketamine, the mean systemic
arterial pressure was increased significantly
in all groups of patients, while the median
pulmonary arterial pressure, resistance to pulmonary
and systemic arteries remained unchanged (Zeynep
Tosun et al., 2006).
The effects of sevoflurane on pulmonary arterial
pressure or pulmonary vascular resistance, as
well as the possible effects on the pulmonary
blood flow have been highlighted in studies
that have mainly been focused on reducing pulmonary
arterial pressure and reducing pulmonary arterial
pressure, but these effects on the pulmonary
artery that has been damaged previously, or
pulmonary arterial pressure has been increased,
it is not so noticeable. In the initial studies
to evaluate the effects of sevoflurane, 21 individuals
who were healthy and without need for surgery
were voluntarily subjected to anesthesia with
sevoflurane, isoflurane or combination of sevoflurane
and 60% nitrous oxide. Studies and performed
tests in these subjects showed that sevoflurane
did not change much on heart rate, reduced the
resistance of arterial vessels and systemic
vessels, and decreased the resistance of the
pulmonary artery and increased blood flow (Hala
et al., 2016). Alawi Tabatabaei (2016) compared
the effects of two anesthetic methods with combination
of ketamine/sevoflurane and ketamine/Propofol
combination on cardiovascular variables in children
with diagnostic cardiac angiography. They concluded
that the use of ketamine and Propofol or ketamine
and sevoflurane did not significantly differ
in hemodynamic indexes of patients. However,
it should be emphasized that patients receiving
sevoflurane had higher systolic blood pressure
and shorter recovery time. Regarding the relatively
high use of sevoflurane and Propofol and the
lack of studies in this field, this study aimed
to investigate the effect of sevoflurane and
Propofol on pulmonary arterial pressure during
cardiac catheterization in children with congenital
heart disease.
The study was a single-blind clinical trial.
The research population was all patients with
congenital heart disease in the age range of
three months to 12 years and 80 patients with
congenital heart disease were selected by available
sampling method who were referred to Modarres
Hospital, Iran for diagnostic and therapeutic
measures under cardiac catheterization. The
samples were divided into two groups: Propofol
and sevoflurane.
The sample size was 80 individuals based on
similar research (p0.05) and a test power of
80%. The criteria for entering the study included:
the age of patients between 3 months and 12
years old, congenital heart disease, stable
hemodynamic symptoms, absence of pulmonary,
renal, hepatic, and co-abnormalities, etc.,
no history of drug allergy or allergies to food,
ASA class 2-3, lack of infectious diseases and
withdrawal criteria included: respiratory distress,
apnea or a clear drop in arterial oxygen saturation,
severe hemodynamic impairment and need for treatment
during catheterization, stable cardiac arrhythmia
requiring interventional therapy, ventilation
disorder requiring interventional and respiratory
support and seizure during prognosis. Ethical
Criteria in this study was approved by the ethics
committee of Shahid Beheshti University of Medical
Sciences.
After diagnosis of the patient as an appropriate
case, the necessary explanations were given
to the parents of the patient about the method
of implementation and the benefits and possible
complications of participating in the project,
and written consent was obtained from them.
Intervention was performed without cost to the
patient. Before the intervention, parents were
asked to fill out a demographic questionnaire
including gender, age, and history of previous
treatments, background history of the disease
and the duration of the symptoms.
Regarding moral considerations, the patient’s
parents were assured that their lack of cooperation
with the doctor and the hospital would not affect
their treatment and all patient information
would be kept confidential. After entering the
heart catheterization department, details of
the followed cases were recorded comprising
hemodynamic baseline values, such as heart rate,
and respiratory rate per minute, cystic and
diastolic blood pressures, arterial pulse oxygen
saturation in the room, the presence or absence
of cyanotype of the child, as well as tests,
blood, biochemistry and electrolyte and liver
enzymes, thyroid and renal function tests, as
well as those observed in scans and grafts.
The use of any medication or nutritional supplement,
a history of drug allergy or allergy to food,
and other cases was also noted and recorded
in the patient records. All patients were to
be NPO according to the age and specific characteristics
of the period before lung catheterization, in
which case their parents were provided with
explanations and warnings. One hour before catheterization,
0.5 mg/kg oral midazolam was prescribed as a
premedication. Peripheral venous catheter was
embedded before the start of the procedure.
In children in the sevoflurane group, anesthesia
initially began with higher concentrations of
sevoflurane (4-6%) and spontaneous respiration
by face mask and gradually reduced the concentration
of gas by increasing the anesthetic depth, and
continuous anesthesia with 1 MAC of inhalant
sevoflurane based on age and individual characteristics
of each patient and spontaneous breathing.
In the other group, Propofol 50-70 g/kg/min
was injected through a perfusion pump, and when
the depth of anesthesia reached the appropriate
level (Ramsay Sedation Score = 3 and BIS = 65-85),
the cardiac catheterization was performed with
lidocaine injection at the catheter entrance
i.e. femoral vessels. Systemic hemodynamic symptoms,
systolic and diastolic blood pressure of the
pulmonary artery were recorded after catheter
entrance into the pulmonary artery. In analyzing
data, mean, standard deviations, frequency,
tables and charts were used to categorize and
summarize the collected data. In the study of
statistical pre-requisites, considering the
number of observations in each distribution,
the Kolmogorov-Smirnov test was used to verify
the distribution of data. According to statistical
hypotheses, paired t- test was used (p<0.05)
using statistical package version 22. In all
analyses, the significance level was considered
as p <0.05.
The
participants
in
this
study
consisted
of
35
females
(43%)
and
45
males
(57%).
The
mean
age
for
sevoflurane
was
0.24
±
2.1
years
and
in
the
Propofol
group
was
7.4
±
0.54
years.
Table
1
shows
the
changes
in
systolic
and
diastolic
blood
pressure
from
pre-test
to
post-test.
Table
1:
Descriptive
statistics
of
the
research
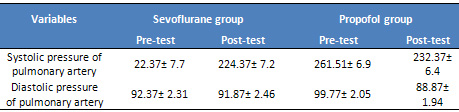
Pulmonary
artery
systolic
blood
pressure
The
results
of
Kolmogorov-Smirnov
test
showed
that
the
distribution
of
data
was
normal
(P>0.05).
In
this
study,
systolic
blood
pressure
in
patients
with
pulmonary
artery
was
measured.
Then,
two
anesthetic
drugs,
sevoflurane
and
Propofol,
was
imposed
on
patients
under
cardiac
catheterization
depending
on
the
type
of
group.
Then,
the
systolic
blood
pressure
of
the
pulmonary
artery
was
re-recorded.
In
the
next
step,
the
blood
pressure
of
post-test
was
compared
with
pre-test
using
paired
t-test
to
determine
whether
a
change
has
been
established
in
pulmonary
artery
systolic
blood
pressure
after
anesthetic
drugs
or
not
(Table
2).
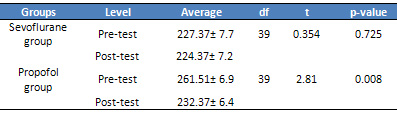
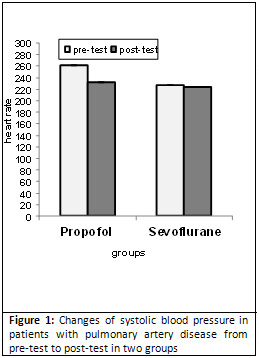
As
can
be
seen
in
the
table,
pulmonary
artery
systolic
blood
pressure
in
the
Sevoflurane
group
in
pre-test
group
was
227,
which
was
decreased
to
224
in
the
post-test,
but
this
decrease
was
not
statistically
significant
(Fig.
1,
p
=
0.725).
While
in
the
Propofol
group,
the
pulmonary
artery
systolic
blood
pressure
was
261
in
the
pretest,
which
was
decreased
to
232
in
the
post-test
and
this
decrease
was
statistically
significant
(Figure
1,
p
=
0.008).
Table
2:
Paired
t-test
for
evaluating
pre-test
and
post-test
of
systolic
blood
pressure
in
patients
with
pulmonary
artery
disease
Pulmonary
artery
diastolic
blood
pressure
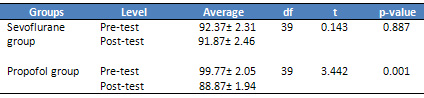
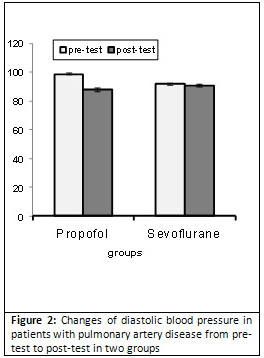
The
results
of
Kolmogorov-Smirnov
test
showed
that
the
distribution
of
data
was
normal
(P>
0.05).
The
paired
t-test
results
are
presented
in
Table
3.
As
seen
in
the
table,
the
diastolic
blood
pressure
of
the
pulmonary
artery
was
92
in
the
sevoflurane
group
in
the
pre-test,
which
was
decreased
to
91
in
the
posttest,
but
this
decrease
was
not
statistically
significant
(Fig.
2,
p=0.887).
While
in
the
Propofol
group,
the
diastolic
blood
pressure
of
the
pulmonary
artery
was
99
in
pre-test,
which
was
decreased
to
88
in
the
post-test
and
this
decrease
was
statistically
significant
(Figure
2,
p
=
0.001).
Table
3:
Paired
t-test
for
evaluating
pre-test
and
post-test
of
diastolic
blood
pressure
in
patients
with
pulmonary
artery
disease
| DISCUSSION
AND
CONCLUSION
|
The
aim
of
this
study
was
to
evaluate
the
effect
of
sevoflurane
and
Propofol
on
pulmonary
arterial
pressure
during
cardiac
catheterization
in
children
with
congenital
heart
disease.
The
results
showed
that
the
effect
of
Propofol
was
statistically
significant
on
the
reduction
of
systolic
and
diastolic
pulmonary
arterial
pressure
during
cardiac
catheterization
while
the
effect
of
Sevoflurane
was
not
significant.
The
comparison
of
the
mean
values
showed
that
pulmonary
artery
systolic
blood
pressure
was
decreased
from
261
mmHg
to
232
mmHg
and
the
pulmonary
artery
diastolic
blood
pressure
ranged
from
99
to
88
mmHg.
Propofol
leads
to
a
greater
reduction
in
blood
pressure
than
Sevoflurane
(Peishun
et
al.,
2016).
The
findings
of
this
study
were
in
line
with
the
results
of
previous
studies.
For
example,
Kariman
Majd
et
al.
(2006)
examined
the
effect
of
various
proportions
of
Propofol
and
ketamine
on
hemodynamic
changes
in
patients.
Their
findings
showed
that
the
Propofol
group
experienced
a
greater
reduction
in
pulmonary
artery
systolic
and
diastolic
blood
pressure
in
comparison
to
the
ketamine
group.
Kirkpatrick
et
al.
(1988)
also
found
that
blood
pressure
reduction
is
very
intense
in
the
elderly
after
induction
with
Propofol,
and
the
drop
in
pressure
is
lower
in
the
younger
group.
In
other
studies,
the
effects
of
Sevoflurane
and
Propofol
have
been
compared.
For
example,
Inh
et
al.
(2009)
investigated
and
compared
inhaled
inductive
anesthetics
and
preservation
of
anesthesia
(VIMA)
with
sevoflurane
with
complete
intravenous
anesthesia
(TIVA)
with
Propofol
and
remifentanil
for
adrenalin,
norepinephrine,
cortisol,
and
Glucose
and
IL-6
plasma
in
four
levels
of
basal
level,
induction
of
anesthesia,
secretion
and
separation
of
the
device.
The
findings
showed
that
the
levels
of
glucose,
cortisol,
adrenaline
and
noradrenaline
in
the
TIVA
group
were
significantly
lower
than
the
VIMA
group.
But
there
was
no
difference
between
the
two
groups
at
IL-6
level.
Weale
et
al.
(2003)
found
that
in
a
clinical
trial
on
49
children
under
the
age
of
5
years,
remifentanil
infusion
(1
g/kg/min
and
further)
can
prevent
glucose
increase
associated
with
phase
before
heart
surgery
bypass.
There
are
many
hypotheses
about
the
effect
of
these
drugs
on
hyperglycemia
during
surgery.
Studies
in
pigs
and
humans
have
shown
that
sevoflurane
reduces
insulin
secretion
and,
as
a
result,
reduces
the
use
of
glucose
(Tanaka
et
al.,
2005).
Also,
anesthesia
with
sevoflurane
in
comparison
with
Propofol
provides
better
glycolysis
in
skeletal
muscle
cells
in
induction
of
ischemia
with
tourniquet
(Carles
et
al.,
2008).
In
contrast,
Propofol
decreases
the
activity
of
sympathetic
nerves
(Ebert
et
al.,
1992).
Apparently,
the
mechanism
of
glucose
metabolism
is
different
in
anesthesia
with
Propofol
with
anesthesia
surgery
with
sevoflurane
(Kitamura
et
al.,
2009).
The
probable
mechanism
of
Propofol
effect
can
be
expressed
in
such
a
way
that
it
can
inhibit
the
activity
of
the
sympathetic
nervous
system
more
than
parasympathetic.
In
fact,
bradycardia
and
ascites
have
been
observed
after
induction
of
anesthesia,
which
sometimes
leads
to
recommend
prescribing
anticholinergic
drugs
at
a
time
when
there
is
a
potential
for
vagus
stimulation
with
Propofol
prescription.
Propofol
reduces
the
resistance
of
peripheral
arteries
and
blood
pressure,
which
is
most
commonly
observed
with
the
same
thiopental
value.
Vessel
smooth
muscle
relaxation
by
Propofol
is
essentially
related
to
the
activity
of
vascular
spasm
nerves
in
the
sympathetic
nervous
system.
The
effect
of
the
negative
inotropy
of
Propofol
may
be
the
result
of
inhibition
of
intracellular
calcium
intake.
The
effect
of
Propofol
on
blood
pressure
may
be
worse
in
patients
with
hypovolemic,
elderly,
and
left
ventricular
dysfunctional
patients
with
coronary
artery
disease.
Despite
the
decrease
in
blood
pressure,
heart
rate
often
remains
fast
and
unchanged
(Reves
et
al.,
2000).
Some
studies
concluded
that
cognitive
function
in
the
sevoflurane
group
was
better
than
the
Propofol
group
in
elderly
subjects
after
general
surgery
(Kheirkhah,
2014).
According
to
the
results
of
this
study,
it
can
be
concluded
that
for
cardiac
catheterization
in
children
with
congenital
heart
disease,
Propofol
is
more
appropriate
than
sevoflurane.
Anesthesiologists
can
use
Propofol
as
a
good
alternative
to
sevoflurane.
1-
Alavi
Tabatabai,
Maryam
(2016).
Comparing
the
effect
of
two
methods
of
anesthesia
with
combination
of
ketamine
/
sevoflurane
and
ketamine
/
Propofol
on
cardiovascular-respiratory
variables
in
diagnostic
cardiac
angiography
patients
of
Pediatric
Medical
Center
Hospital
in
2014,
Medical
Ph.D.,
School
of
Medicine,
Tehran
University
of
Medical
Sciences,
Tehran,
Iran.
2-
Kheirkhah,
Parviz.
(2014).
Comparison
of
Anesthetic
Effects
with
Sevoflurane
and
Propofol
on
Early
Cognitive
Function
in
Elderly
(55-65)
Years,
PhD,
thesis
of
Anesthesiology,
Kashan
University
of
Medical
Sciences.
3-
Bernstein,
D.
(2000).
The
cardiovascular
system:
in:
Behrman
RE,
Kliegman
RM,
Jenson
HB,
editors.
Nelson
textbook
of
pediatrics.
16th.
Philadelphia;
WB
sunders,
pp
1367-1455
4-
Barst.
Rj.
(2001).
Clinical
management
of
patients
with
pulmonary
hypertension;
in:
Allen
Hd,
Gutgesell
Hp,
Clark
Eb,
Driscoll
DJ,
editors.
Moss
and
Adams
heart
disease
in
infants,
children,
and
adolescents.
6th
ed.
Philadelphia;
Lippincot
Williams
&
Wilkins,
1347-1361
5-
Carles
M,
Dellamonica
J,
Roux
J,
Lena
D,
Levraut
J,
Pittet
JF,
Boileau
P,
Raucoules-Aime
M.
Sevoflurane
but
not
propofol
increases
interstitial
glycolysis
metabolites
availability
during
tourniquet-induced
ischaemia
reperfusion.
Br
J
Anaesth
2008;
100:29–35.
6-
Ebert
TJ,
Muzi
M,
Berens
R,
Goff
D,
Kampine
JP.
Sympathetic
responses
to
induction
of
anesthesia
in
humans
with
propofol
or
etomidate.
Anesthesiology
1992;
76:725–33
7-
Goh
PK,
Chiu
CL,
Wang
CY,
et
al.
Randomized
double
blind
comparison
of
ketamine-propofol,
fentanyl
mask
airway
insertion
conditions.
Anaesth
intensive
care,
2005;
33(2):
223-8.
8-
Greff
M.
Colorectal
cancer
screening
in
France:
guidelines
and
professional
reality.
Endoscopy
1999;
31:471.
9-
Liberman
DA,
Wuerker
CK,
Katon
RM.
Cardiopulmonary
risk
of
esophagogasteroduodenoscopy:
role
of
endoscope
diameter
and
systemic
sedation.
Gastroentology,
1985;
88:468-72.
10-
Jellish
WS,
Owen
K,
Edelstein
S,
Fleuder
E,
Leoneti
JP.
Standard
anesthetic
technique
for
middle
ear
surgical
Procedures:
A
comparison
of
desflurane
and
sevoflurane.
Otolaryngeal
Head
Neck
Surgery,
2005;
133(2):
269-74
11-
Hala
M.S.
Eldeen
MD
,
Medhat
M
Messeha,
Comparative
study
between
the
effect
of
sevoflurane
and
ketamine-midazolam
on
the
cardiac
troponin
I
level
and
hemodynamic
variables
in
pediatric
therapeutic
cardiac
catheterization
for
pulmonic
stenosis,
Ains
Shams
journal
of
anesthesiology,
2016,
9(1),
12-17
12-
Kariman
Majd
MH,
Emadi
A,
Nasiri
E,
et
al.
Comparative
effects
of
Propofol
and
Ketamine
in
different
dosage
on
patients
hemodynamic
changes
under
anesthesia.
J
Mazandaran
Univ
Med
Sci,
2006;
16(54):7-13
13-
Kitamura
T,
Ogawa
M,
Kawamura
G
et
al.
The
effects
of
sevoflurane
and
propofol
on
glucose
metabolism
under
aerobic
conditions
in
fed
rats.
Anesth
Analg
2009;
109:
1479–85.
14-
Kirkpatrick
T,
cockshott
ID,
Douglas
EJ,
et
al.
Pharmacokinetics
of
Propofol
(diprivan)
in
elderly
patients.
Br
J
Anaesth
1988;60(2):14650.
15-
Lebovic
S,
Reich
DL,
Steinberg
LG,
et
al.
Comparison
of
Propofol
Versus
Ketamine
for
Anesthesia
in
Pediatric
Patients
Undergoing
Cardiac
Catheterization.
Anesth
Analg,
1992;
74:490-4
16-
Patterson
KW,
Casey
PB,
Murray
JP,
et
al.
Propofol
sedation
for
outpatient
upper
gastrointestinal
endoscopy:
comparison
with
Midazolam.
Br
J
Anesth,
1991;67:108-11.
17-
Patrick
MR,
Blair
IJ,
Feneck
RO,
et
al.
A
comparison
of
the
haemodynamic
effects
of
propofol
and
thiopentone
in
patients
with
coronary
artery
disease.
Postgrade
Med
J,
1985;61:23-7.
18-
Peishun
Qin,
Dingxin
Kang,
Xiaowei
Qian,
Lexiao
Jin.
Propofol
versus
sevoflurane
anesthesia
in
adults:
a
systematic
review
and
meta-analysis,
Int
J
Clin
Exp
Med
2016;9(7):13634-13641
19-
Qureshi,
SA.
(2002).
Catheterization
and
angiocardiography:
in:
Anderson
RH,
Baker
EJ,
Macartney
RF,
Rigby
ML,
Shinebourne
EA,
Tynn
M,
editors.
Pediatric
cardiology.
Vol
a,
2nd
ed.
London:
Churchill
Livingston,
pp
567-618.
20-
Reves
JG,
Glass
PSA,
Lubarsky
DA.
Nonbarbiturate
intravenous
anesthetics.
In:
Miller
RD
(ed).
Anesthesia.
Philadelphia.
Churchill
Livingstone,
2000;
228-272.
21-
Reich
DL,
Silvay
G.
Ketamine:
an
update
on
the
first
25
years
of
clinical
experience.
Can
J
Anaesth,
1989;
36:186-97
22-
Short
SM,
Aun
CS.
Haemodynamic
effects
of
propofol
in
children.
Anaesthesia,
1991;
46(9):783-50.
23-
Tanaka
T,
Nabatame
H,
Tanifuji
Y.
Insulin
secretion
and
glucose
utilization
are
impaired
under
general
anesthesia
with
sevoflurane
as
well
as
isoflurane
in
a
concentration-independent
manner.
J
Anesth,
2005;
19:277–
81.
24-
Thwaites
AJ
,
Edmends
S,
Tomlinson
AA,
Kendall
JB,
Smith
I.
Double-blind
comparison
of
sevoflurane
vs
propofol
and
succinylcholine
for
tracheal
intubation
in
in
children.
Br
J
Anaesth,
1999;
83:
410–4
25-
Woods
AW,
Allam
S.
Tracheal
intubation
without
the
use
of
neuromuscular
blocking
agents.
Br
J
Anaesth,
2005;
94:
150-158.
26-
Weale
N.K,
Rogers
C.A,
Cooper
R
et
al.
Effect
of
remifentanil
infusion
rate
on
stress
response
to
the
prebypass
phase
of
paediatric
cardiac
surgery.
British
Journal
of
Anaesthesia,
2004;
92(2):
187-94.
27-
Zeynep
Tosun,
MD
,
Aynur
Akin,
MD,
Gulen
Guler,
MD,
Aliye
Esmaoglu,
MD,
Adem
Boyaci,
MD.
DexmedetomidineKetamine
and
PropofolKetamine
Combinations
for
Anesthesia
in
Spontaneously
Breathing
Pediatric
Patients
Undergoing
Cardiac
Catheterization,
Journal
of
Cardiothoracic
and
Vascular
Anesthesia,
2006;
20(4),
515–519.
|

